You’re probably reading this because something feels... off. Maybe it’s a sharp twinge you didn't have last week, or perhaps you reached up to check those little plastic strings and came back with nothing but questions. Honestly, it’s a weirdly stressful situation. The IUD (intrauterine device) is supposed to be the "set it and forget it" holy grail of birth control, but when you start worrying about iud out of place symptoms, that peace of mind evaporates pretty fast.
It happens. Not often, but it happens.
About 2% to 10% of IUDs end up expelling, which is just a medical way of saying your uterus decided to evict its tenant. Your uterus is a powerful muscle, and sometimes it just doesn't want a piece of T-shaped plastic hanging out in there. If it moves even a few millimeters, it’s not just a matter of discomfort; it can actually tank the device’s effectiveness, leaving you unprotected.
The Signs You Shouldn't Ignore
Let's get straight to the point: what does it actually feel like when an IUD shifts?
First off, you might feel the plastic itself. This is a huge red flag. You should be able to feel the strings—which usually feel like thin fishing line or dental floss—but you should never, ever feel the hard plastic tip of the IUD poking through your cervix. If you do, it’s moved. It’s out of position. Stop what you're doing and call your doctor because that thing is on its way out.
Pain is the other big one. Now, I’m not talking about the mild cramping you get for a few days after insertion. This is different. We’re talking about new, localized, or "sharp" cramping that feels like your period is coming on even when it’s nowhere near that time of the month. According to data from the American College of Obstetricians and Gynecologists (ACOG), abnormal pain is one of the primary reasons patients seek a position check.
📖 Related: Why the EMS 20/20 Podcast is the Best Training You’re Not Getting in School
Heavy or irregular bleeding is another sneaky symptom. If you have a hormonal IUD like Mirena or Kyleena, your periods are usually supposed to get lighter or disappear entirely. If suddenly you’re spotting every day or having a heavy "crash" bleed, the IUD might have shifted into the lower uterine segment or the cervical canal. Your body is reacting to the displacement.
The Mystery of the Missing Strings
Check your strings. Seriously.
Doctors usually recommend doing this once a month. If the strings feel way longer than they used to, the IUD has likely slipped down. If they’re gone? Well, two things could have happened. Either the strings have curled up into the cervical canal (which is common and usually fine), or the whole device has moved. Or, in rare cases of perforation, it could have moved through the uterine wall.
Don't panic. Perforation is incredibly rare, occurring in roughly 1 out of every 1,000 insertions. It usually happens during the insertion process, not months later, but it’s still something providers like those at the Mayo Clinic watch for if a patient presents with severe, localized pelvic pain.
Why Does It Move Anyway?
It’s not usually anything you did. You didn't "dislodge" it by using a tampon or having vigorous sex. Usually, it's just anatomy.
👉 See also: High Protein in a Blood Test: What Most People Get Wrong
If you have a small uterine cavity or if you have uterine fibroids, there’s less "real estate" for the IUD to sit comfortably. Also, if you’re younger—specifically under 20—research suggests you might have a slightly higher risk of expulsion. Why? Because the uterus might be more prone to strong contractions that push the device toward the exit.
The "Malposition" Nuance
There is a difference between an IUD that is "expelled" and one that is "malpositioned."
A malpositioned IUD might still be inside the uterus but sitting too low or turned sideways. While some studies, like those published in the American Journal of Obstetrics & Gynecology, suggest that even a slightly low-sitting IUD can still prevent pregnancy, most clinicians prefer to re-seat or replace it. If it's not where it's supposed to be, it's not working at the 99% efficacy rate you're paying for.
What to Do Right This Second
If you have iud out of place symptoms, the very first rule is: Use a backup method of birth control. Basically, assume you are not protected. Use condoms until a professional confirms the placement with an ultrasound.
- Do not try to pull it out yourself. I know it’s tempting if you can feel the plastic poking you, but you can cause a lot of trauma to the cervix or even an infection.
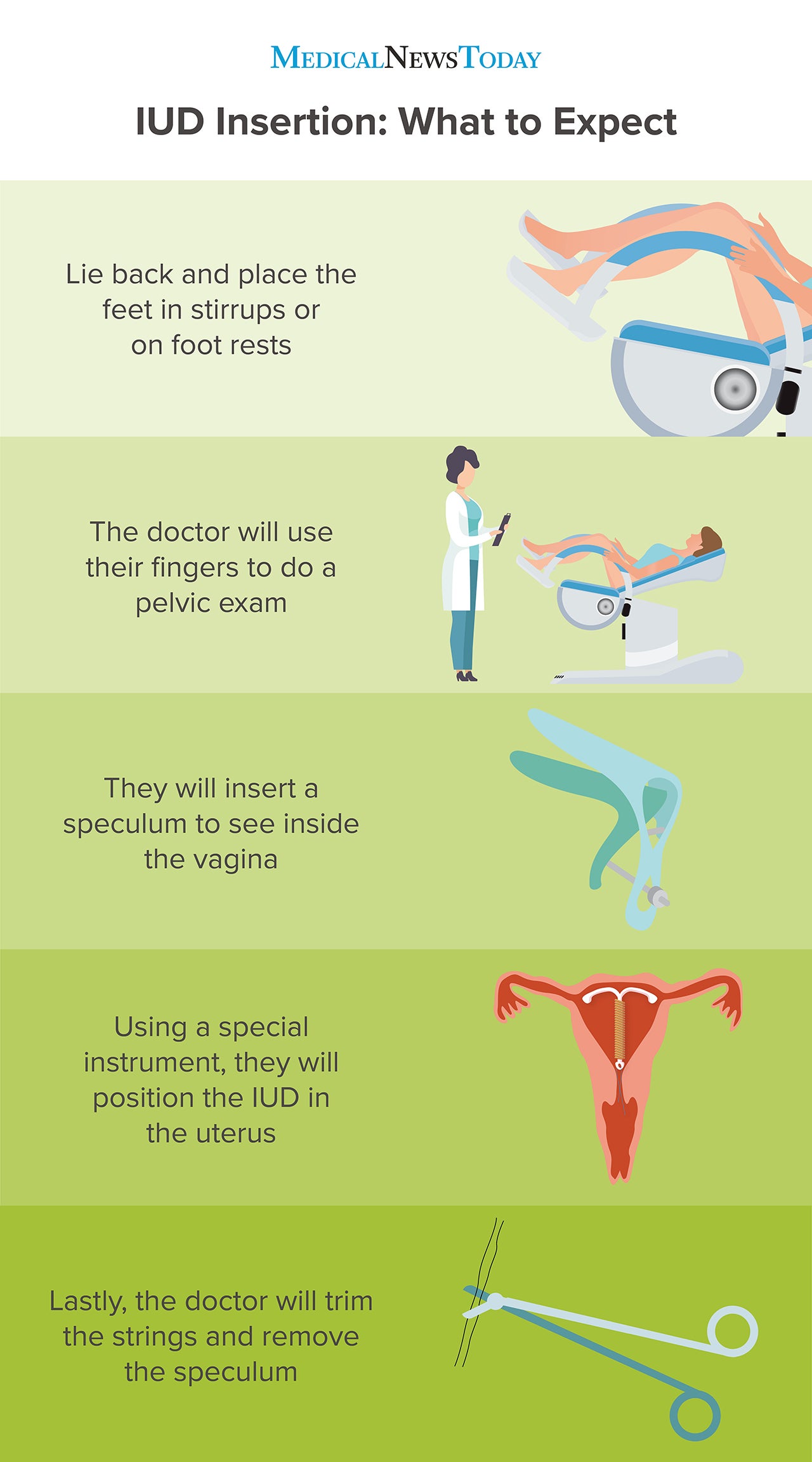
- Book an "IUD Check" appointment. Your doctor will do a speculum exam first. If they can’t see the strings, they’ll order a transvaginal ultrasound. This is the gold standard for seeing exactly where that little T is hiding.
- Monitor for fever. If you have pain and a fever, that’s an emergency. It could indicate an infection or a perforation. Head to urgent care.
Real Talk: The "Embedded" IUD
Sometimes the IUD doesn't move out, it moves in.
✨ Don't miss: How to take out IUD: What your doctor might not tell you about the process
This is called an embedded IUD, where the arms of the device get stuck in the muscular wall of the uterus (the myometrium). This usually causes persistent, nagging pain or cramping that doesn't go away with Ibuprofen. It’s a bit trickier to remove and might require a slightly more involved office procedure or, in very rare cases, hysteroscopy (where they use a tiny camera to find it).
It sounds scary, but it’s manageable. Doctors handle this all the time.
Moving Forward and Next Steps
Once you’ve confirmed the IUD is out of place, you have a choice to make. You can have a new one inserted immediately after the old one is removed, or you can switch methods. If your body expelled it once, there is a slightly higher chance (about 20-30%) it might happen again. Some people find that switching from a larger IUD like Mirena to a smaller one like Skyla helps, as the smaller frame might fit their anatomy better.
Actionable Next Steps:
- Perform a self-check: Wash your hands, squat, and use your longest finger to feel for the strings near your cervix. If they feel significantly longer, shorter, or absent, take note.
- Track your symptoms: Use a cycle tracking app to note any "off-cycle" cramping or sudden changes in bleeding patterns over the last 30 days.
- Schedule an ultrasound: If your strings are missing but you aren't in pain, request a "string check ultrasound" specifically. This ensures the technician looks for the device’s location within the uterine cavity.
- Switch to backup: Use barrier protection (condoms) immediately if you suspect displacement, and continue until a medical professional confirms the IUD is fundal (at the top of the uterus).
Ultimately, your intuition matters. If you feel like something is wrong, it probably is. Don't let anyone tell you that "cramping is just part of it" if the pain feels new or different. Get the check-up, get the ultrasound, and get your peace of mind back.