It starts small. You’re lying in bed at 3:00 AM, staring at the ceiling, wondering why your heart is racing for absolutely no reason. You aren't stressed about work. You didn't have a late espresso. But there you are, wide awake, feeling a strange, creeping sense of dread. Most people call it "getting older" or "just stress," but more often than not, it’s the beginning of a decade-long hormonal shift that remains shockingly misunderstood.
If you try to list all symptoms of perimenopause, you’ll realize pretty quickly that the "textbook" definition is a joke.
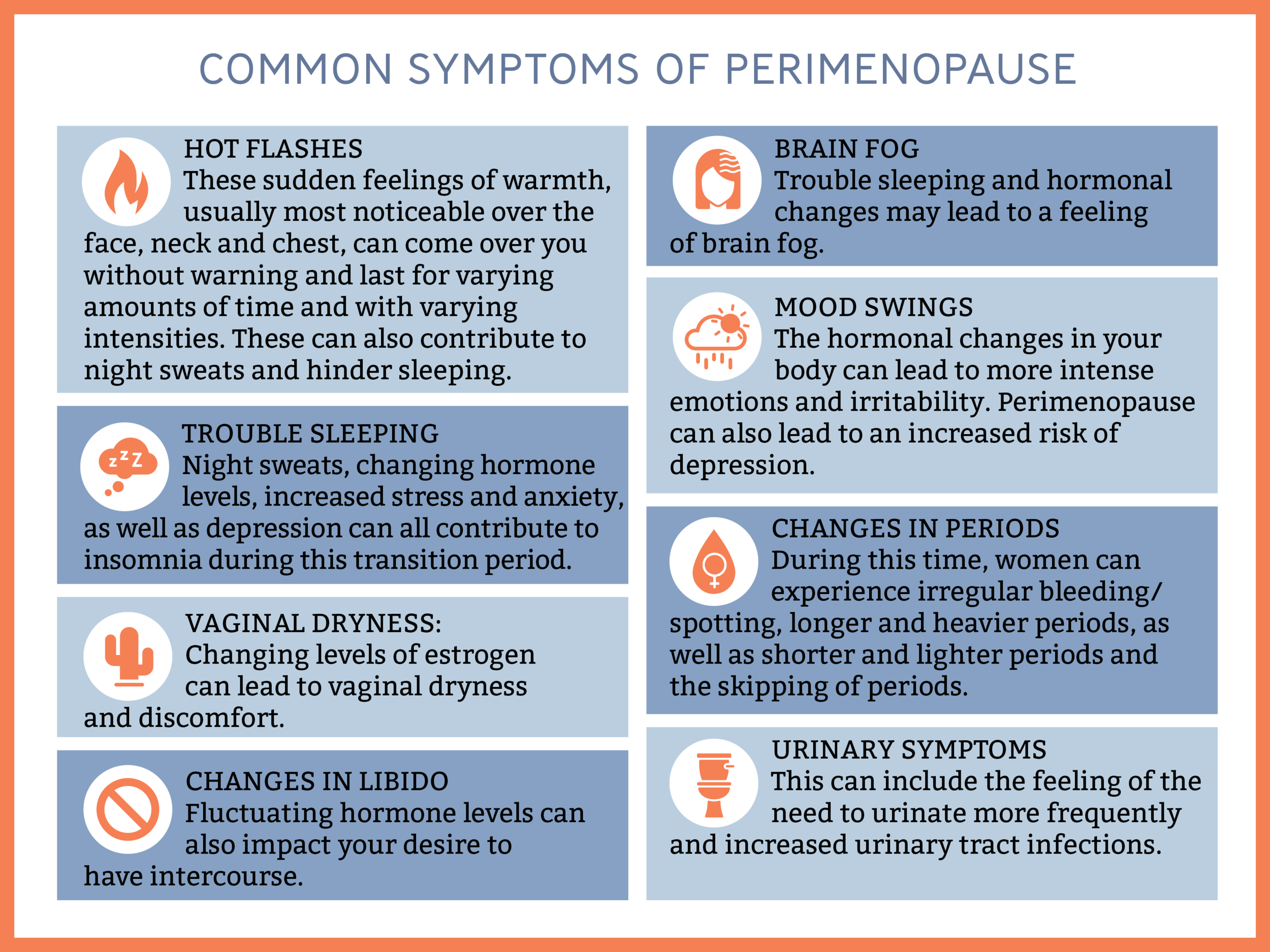
Doctors often focus on the big two: hot flashes and irregular periods. But for many women, those aren't even the first signs. It’s the "invisible" stuff—the brain fog that makes you forget your best friend's name, the sudden joint pain that feels like you ran a marathon in your sleep, or the "rage" that comes out of nowhere because someone breathed too loudly.
The Chaos of the Transition
Perimenopause isn't a single event. It’s a process. Specifically, it’s the time leading up to menopause when the ovaries gradually begin to make less estrogen. According to the North American Menopause Society (NAMS), this transition can last anywhere from four to ten years.
During this time, your hormones aren't just dropping; they are fluctuating wildly. Think of it like a roller coaster where the tracks are breaking. One day your estrogen is sky-high, the next it’s plummeted. This volatility is why you can feel like a completely different person from Tuesday to Thursday.
Most people don't realize that we have estrogen receptors all over our bodies. Our brains, our hearts, our bones, and even our skin. When those levels get wonky, everything else follows suit.
To Truly List All Symptoms of Perimenopause, We Have to Look Beyond Hot Flashes
Let's get into the weeds. If you're looking for a checklist to take to your GP, you need the weird stuff too.
📖 Related: Does Ginger Ale Help With Upset Stomach? Why Your Soda Habit Might Be Making Things Worse
The Psychological Shift
Honestly, the mental health aspect is what catches most people off guard. We’re talking about anxiety that feels like it’s vibrating under your skin. Panic attacks in women who have never had one. Depression that feels "heavy" and unresponsive to usual coping mechanisms. This isn't just "moodiness." It’s a neurological response to declining estradiol.
The Sleep Sabotage
It isn't just about night sweats. Sure, waking up in a pool of water is a classic sign. But there’s also the initial insomnia (can’t fall asleep) and the maintenance insomnia (waking up at 4:00 AM every night). Often, this is linked to a drop in progesterone, which is our body's natural "chilling out" hormone.
Physical Changes You Didn't Expect
- Burning Mouth Syndrome: It sounds fake, but it’s a real, documented symptom where your tongue or gums feel scalded.
- Formication: The sensation of insects crawling on your skin. It’s incredibly unsettling.
- The "Frozen Shoulder": Adhesive capsulitis is strangely common in perimenopausal women.
- Tinnitus: A sudden ringing in the ears that won't quit.
- Gum Issues: Your teeth might feel sensitive, or your gums might start bleeding more easily because of thinning mucosal membranes.
Why Your Doctor Might Miss It
Here is the frustrating reality: there is no single blood test that "proves" you are in perimenopause.
Since your hormones are swinging up and down hourly, a blood draw on Monday might show "normal" levels, even if you felt like a train wreck on Sunday. Many women are told their labs are fine and are handed a prescription for antidepressants instead of hormone therapy. While antidepressants can help some, they don't address the underlying hormonal depletion.
Experts like Dr. Mary Claire Haver and Dr. Louise Newson have been vocal about this gap in medical education. They argue that perimenopause should be diagnosed based on symptoms and age (usually 40+), not just a snapshot of FSH (Follicle-Stimulating Hormone) levels.
👉 See also: Horizon Treadmill 7.0 AT: What Most People Get Wrong
The Cognitive Impact: "Where Are My Keys?"
Brain fog is a terrifying symptom. You’re in the middle of a sentence and the word just... vanishes. You find your phone in the refrigerator. You feel like you're moving through a thick mist.
Research from the University of Rochester Medical Center has shown that these cognitive complaints are legitimate. It’s not "early-onset dementia." Estrogen is a fuel source for the brain. It helps with glucose metabolism in the cerebral cortex. When that fuel source becomes unreliable, the brain has to work harder to do the same tasks.
It’s exhausting.
Heart and Bone Health
We need to talk about the stuff you can't feel. When you list all symptoms of perimenopause, you have to include the silent ones. Estrogen is cardioprotective. It helps keep your blood vessels flexible. As it drops, your risk for cardiovascular disease and high cholesterol ticks upward.
The same goes for your bones. You can lose up to 20% of your bone density in the five to seven years around menopause. If you’re suddenly experiencing weird aches or "electric shock" sensations in your limbs, your body is flagging that things are changing.
Navigating the Treatment Jungle
So, what do you actually do?
✨ Don't miss: How to Treat Uneven Skin Tone Without Wasting a Fortune on TikTok Trends
First, track everything. Use an app or a physical journal to note down every weird thing—from the itchy ears to the sudden crying jags. This data is your best weapon in a clinical setting.
Hormone Replacement Therapy (HRT)
For a long time, HRT was treated like a boogeyman because of the 2002 Women's Health Initiative (WHI) study. But modern medicine has re-evaluated that data. For most healthy women under 60, the benefits of HRT (protecting the heart, bones, and brain) far outweigh the risks. Transdermal estrogen (patches or gels) and micronized progesterone are now the gold standard.
Lifestyle Tweaks That Actually Work
- Strength Training: You have to lift heavy things. It’s non-negotiable for bone density and metabolic health now.
- Protein Intake: Your body becomes less efficient at processing protein. Aim for 25-30 grams per meal.
- Magnesium Glycinate: It’s a game-changer for sleep and anxiety for a lot of people.
- Cutting Back on Alcohol: This is the hard one. Alcohol spikes cortisol and worsens hot flashes. Many women find that even one glass of wine ruins their sleep during perimenopause.
Practical Steps for Your Next Move
Don't wait until you're in a full-blown crisis to seek help. If you're in your late 30s or early 40s and "feel off," trust your gut.
Start by finding a menopause specialist. The The Menopause Society (formerly NAMS) has a "Find a Practitioner" tool on their website. These are doctors, NPs, and PAs who have gone through extra certification to understand this specific transition.
When you go to your appointment, bring your list. Be firm. If a doctor tells you you're "too young" for perimenopause at 42, find a different doctor. It is entirely possible to start this transition in your late 30s.
Focus on the "Big Three" pillars for the next 30 days: Resistance training three times a week to protect muscle mass, increasing fiber to help clear out excess "used" hormones, and prioritizing sleep hygiene even when it feels impossible. These aren't just "wellness" tips—they are physiological necessities when your internal chemistry is shifting.
Managing this phase is about advocacy. It’s about knowing your body well enough to say, "This isn't me," and having the resources to fix it.