We’ve all been there. You walk into the kitchen, stare at the fridge, and realize you have absolutely no clue why you’re standing there. Or maybe you spend ten minutes hunting for your glasses only to find them perched on your head.
It’s annoying. It feels like your brain is glitching. But for most of us, that’s just the tax we pay for living in a distracted, high-speed world.
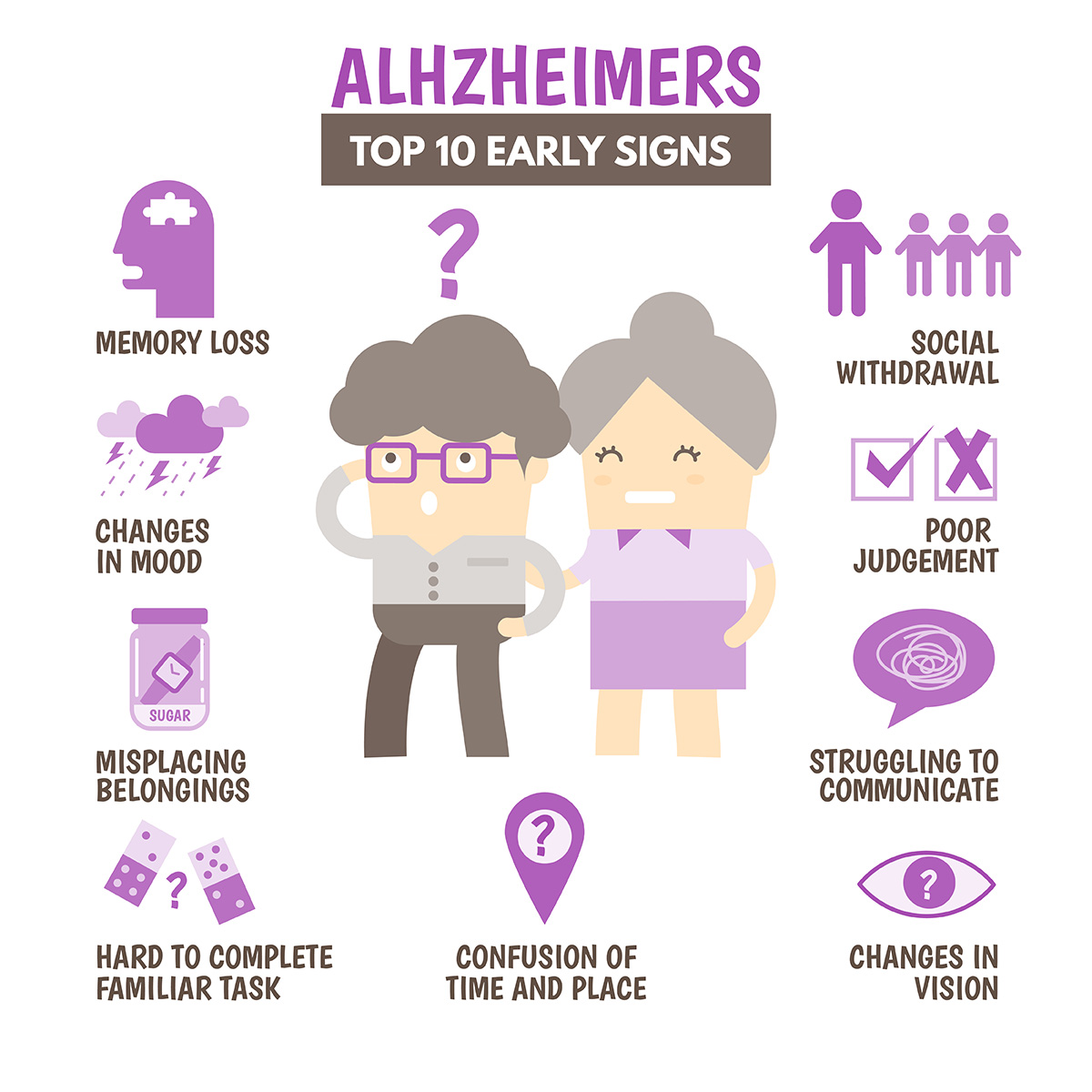
When we talk about what is a symptom of early stage alzheimer's disease, we aren't talking about a one-off brain fart. We are talking about a fundamental shift in how the brain processes the world. It’s subtle. It’s sneaky. Honestly, it’s often the people living with the person who notice it first, while the individual themselves might just feel a bit "off" or more tired than usual.
Alzheimer’s isn't an "old person's" light switch that just flips on one day. It’s a progressive neurodegenerative condition. According to the Alzheimer’s Association, more than 6 million Americans are living with this, and for many, the early signs were dismissed as "senior moments" for years before a diagnosis.
The Memory Loss That Actually Matters
Memory loss is the hallmark, sure. But not all memory loss is created equal.
If you forget where you parked at the mall, that’s normal. If you forget that you even drove to the mall, that’s a red flag. In the early stages of Alzheimer's, the brain’s ability to retain newly learned information is usually the first thing to crumble. This is because the hippocampus—the brain's "loading dock" for new memories—is often the first area to sustain damage from amyloid plaques and tau tangles.
You might find someone asking the same question three times in twenty minutes. Not because they weren't listening, but because the "save" button in their brain isn't working. They might start relying heavily on memory aids, like Post-it notes everywhere or digital reminders, for things they used to handle effortlessly.
🔗 Read more: Why Raw Milk Is Bad: What Enthusiasts Often Ignore About The Science
It's Not Just About Forgetting Names
One of the most overlooked aspects of what is a symptom of early stage alzheimer's disease is a change in executive function. Basically, the "CEO" of the brain starts taking too many long lunches.
Think about a recipe. Making a complex lasagna requires timing, sequencing, and multitasking. You have to boil the noodles while browning the meat and shredding the cheese. An individual in the early stages might find these multi-step tasks suddenly overwhelming. They might get lost in the middle of a familiar hobby, like bridge or woodworking, because they can't remember the next logical step.
Numbers often become an early enemy. Balancing a checkbook or managing monthly bills—tasks that were once second nature—suddenly feel like advanced calculus. It isn't just a mistake here and there; it’s a total loss of the "map" for how to handle the process.
Confusion With Time and Place
Imagine waking up from a nap and for a split second, you don't know where you are. That happens to everyone. But for someone with early Alzheimer’s, that feeling doesn't always go away.
They might lose track of dates, seasons, and the passage of time. They may forget how they got to a certain place or why they are there. This isn't just being "absent-minded." It’s a genuine disconnect from the present moment. Experts at the Mayo Clinic note that this spatial disorientation is a key differentiator between normal aging and cognitive decline.
Sometimes it shows up in vision, too. This is weirdly common but rarely talked about. The brain might struggle to judge distance or determine color and contrast. This makes driving incredibly dangerous, even if the person’s reflexes are still okay. They might see a shadow on the floor and think it’s a hole, or struggle to realize how far away the car in front of them actually is.
💡 You might also like: Why Poetry About Bipolar Disorder Hits Different
The Subtle Shift in Conversation
Vocabulary starts to slip away. It’s called anomia.
We all have "tip-of-the-tongue" moments where we can't find a word. But a person with early-stage symptoms might stop in the middle of a sentence and have no idea how to continue. Or they might use the wrong name for things—calling a watch a "hand-clock" or a refrigerator a "cold box."
It’s exhausting to hold a conversation when your brain is constantly searching for missing pieces. Because of this, many people start to withdraw. They stop going to book club. They stop calling friends. It’s not that they’ve become antisocial; it’s that social interaction has become a Herculean effort that highlights their struggles.
Personality Changes Nobody Warns You About
This is often the hardest part for families. Alzheimer's can change a person's "vibe" before it takes their memories.
- Mood Swings: Someone who was always calm might become easily upset, anxious, or suspicious of family members.
- Loss of Initiative: A lifelong gardener might just sit and stare at the weeds for hours. This isn't laziness; it’s apathy caused by the brain losing the "spark" to initiate action.
- Poor Judgment: This is a big one. You might see a normally frugal person give away large sums of money to telemarketers or buy things they clearly don't need. They might also stop grooming themselves or pay less attention to hygiene.
Why Does This Happen?
Biologically, we’re looking at a protein problem. In a healthy brain, fragments of a protein called beta-amyloid are cleared away. In an Alzheimer’s brain, they clump together into plaques. These plaques sit between neurons and disrupt cell-to-cell signaling.
Then there’s tau. Normally, tau helps stabilize the internal transport system of neurons. In Alzheimer’s, it collapses into "tangles," which basically starves the brain cells of nutrients. When cells die, the brain shrinks. It’s a physical, structural change, not just a "mental" one.
📖 Related: Why Bloodletting & Miraculous Cures Still Haunt Modern Medicine
The "False Positives" to Watch Out For
Before you panic because you forgot your anniversary, remember that many things mimic Alzheimer’s.
B12 deficiency can cause massive brain fog. Dehydration is a huge culprit, especially in older adults. Depression can actually look exactly like dementia in a phenomenon called "pseudodementia." Even certain medications or urinary tract infections (UTIs) can cause sudden, sharp cognitive declines that look like Alzheimer's but are actually reversible.
This is why getting a professional workup is non-negotiable. A neurologist won't just give a memory test; they’ll do blood work and potentially an MRI or PET scan to see what’s actually happening under the hood.
Actionable Next Steps if You're Worried
If you or a loved one are ticking several of these boxes, don't wait for it to "get better." It doesn't. But early intervention changes the game.
- Start a "Symptom Log": Write down specific instances. "On Tuesday, Dad forgot how to get home from the grocery store he’s used for 20 years." Specificity helps doctors more than general "he’s getting forgetful" comments.
- Rule Out the Basics: Schedule a full physical. Check for UTIs, thyroid issues, and vitamin deficiencies. Sometimes the fix is a supplement or an antibiotic, not a life-altering diagnosis.
- Get a Cognitive Screening: Ask for a MoCA (Montreal Cognitive Assessment) or a MMSE (Mini-Mental State Exam). These are quick tests that can help determine if the memory issues are age-appropriate or clinically significant.
- Look into Clinical Trials: Sites like Antidote or the Alzheimer’s Association’s TrialMatch can connect you with research. Early-stage patients are often the best candidates for new treatments that aim to slow the progression of the disease.
- Audit the Environment: If there is a diagnosis, start simplifying. Remove trip hazards, use automatic bill pay, and label important drawers. Small changes now prevent big crises later.
The reality is that what is a symptom of early stage alzheimer's disease is a spectrum. No two people experience it the same way. One person might lose their sense of direction while their vocabulary remains perfect. Another might become a different person emotionally while still being able to do their taxes. Trust your gut. If something feels significantly different than it was two years ago, it’s worth a conversation with a professional.