Finding something red or dark in the toilet bowl is enough to make anyone’s heart skip a beat. It’s scary. You’re sitting there, staring down, wondering if you should call a doctor or if it was just that beet salad you had for lunch. Honestly, most people panic immediately. But knowing how to tell if there is blood in your stool is about more than just seeing red. It’s about texture, timing, and sometimes even the smell.
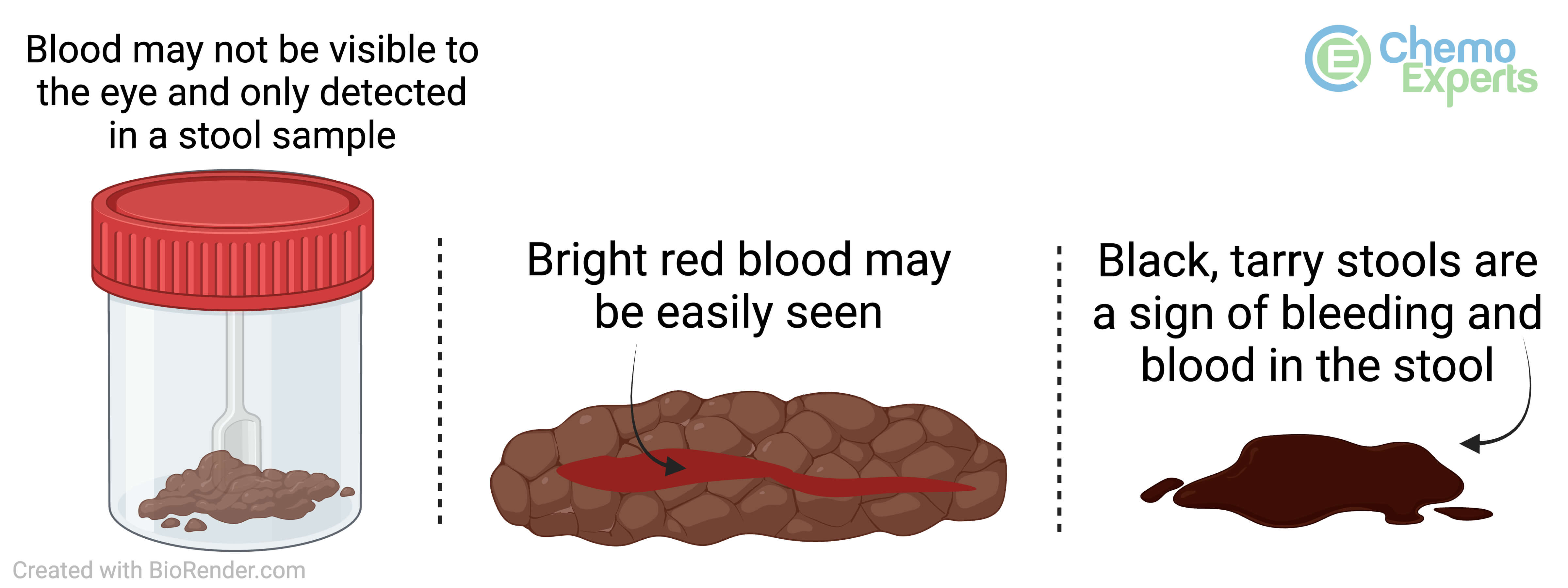
The reality is that "blood" doesn't always look like blood. Sometimes it’s a bright, alarming crimson that looks like a paper cut. Other times, it’s a thick, tarry black mess that you wouldn't even recognize as blood unless someone told you.
The Color Spectrum: It’s Not Always Red
Bright red blood is technically called hematochezia. If you see this, the "source" is usually somewhere low down in your digestive tract, like the rectum or the very end of the colon. Why? Because the blood hasn't had time to be digested. It’s fresh. It might be on the toilet paper, or it might be a few drops in the water.
Then there’s the dark stuff.
Doctors call this melena. It’s sticky. It’s black. It looks like used motor oil or coffee grounds. This is actually "old" blood that has been partially digested by stomach acid and enzymes. If your stool looks like this, the bleeding is likely happening much higher up—think stomach or esophagus. It’s a very different vibe than a hemorrhoid flare-up.
But wait. There is a third type that’s the most annoying of all: occult blood. You can't see it. It’s invisible to the naked eye. The only way you find out it’s there is through a fecal immunochemical test (FIT) or a guaiac-based test during a routine checkup. This is often why doctors find colon polyps before they ever turn into something worse.
The Great Pretenders: Foods That Look Like Blood
Before you spiral, think about what you ate. Seriously. Beets are the number one culprit. They can turn your stool—and even your urine—a deep, frightening magenta. It’s called beeturia.
📖 Related: Why PMS Food Cravings Are So Intense and What You Can Actually Do About Them
Other things that mess with your head:
- Red velvet cake (that dye is strong)
- Iron supplements (these make stool look black and greenish-black)
- Pepto-Bismol (bismuth subsalicylate reacts with sulfur in your saliva and gut to turn stool black)
- Blackberries or blueberries in large amounts
- Red gelatin or sports drinks
If you aren't sure, wait 24 to 48 hours. If the color clears up after you stop eating the red stuff, you're probably fine. If it stays? That’s when you pay attention.
How to Tell if There Is Blood in Your Stool Based on Symptoms
Blood rarely travels alone. Usually, it brings friends like pain, itching, or a change in your bathroom habits.
If you have bright red blood on the paper and it feels like you're passing shards of glass, it's almost certainly an anal fissure. These are tiny tears in the lining of the anus. They hurt like crazy, but they aren't usually a "code red" emergency. Then you have hemorrhoids. These are swollen veins. They might itch, or they might just bleed a little bit after you strain.
But what if there’s no pain?
Painless bleeding is actually something that deserves more scrutiny. While it can still be internal hemorrhoids, it is also a classic sign of polyps or even colorectal cancer. Don't assume that "no pain" means "no problem." In fact, according to organizations like the American Cancer Society, early-stage colon cancer is notoriously silent.
👉 See also: 100 percent power of will: Why Most People Fail to Find It
Texture Matters More Than You Think
Is the blood mixed into the stool, or is it just sitting on top?
When blood is mixed thoroughly into a bowel movement, it suggests the bleeding is happening further up in the colon. If it’s just a streak on the outside, it’s likely a local issue near the exit. Consistency is another big clue. If your stool is consistently thinner—like the width of a pencil—and you’re seeing blood, that’s a red flag. It suggests something might be obstructing the path.
When to Actually Worry
Let’s be real: any blood in the toilet is worth a conversation with a professional. But some situations require a "right now" doctor visit.
If you feel dizzy, lightheaded, or like you’re going to faint, that’s bad. It means you might be losing blood faster than you think. A racing heart or extreme paleness are also signs of anemia or acute blood loss.
Dr. Mark Pochapin, a well-known gastroenterologist, often emphasizes that people wait too long because they’re embarrassed. Don't be. These people look at colons for a living. They’ve seen it all. If you have a family history of colon cancer or IBD (like Crohn’s or Ulcerative Colitis), your threshold for calling the doctor should be basically zero.
The Difference Between IBD and IBS
People get these mixed up constantly. Irritable Bowel Syndrome (IBS) is a functional disorder; it causes cramps and bloating, but it does not cause bleeding. If you have been told you have IBS but you start seeing blood, something else is going on. Inflammatory Bowel Disease (IBD), on the other hand, involves actual sores and inflammation in the gut lining that bleed.
✨ Don't miss: Children’s Hospital London Ontario: What Every Parent Actually Needs to Know
Diagnostic Steps: What Happens Next?
If you go to the doctor, they won't just take your word for it. They’ll likely start with a digital rectal exam. Yes, it’s exactly what it sounds like. It’s quick, and it helps them check for immediate issues like hemorrhoids or masses.
From there, you might get a colonoscopy. This is the gold standard. They put you under, use a camera, and look at the entire length of the large intestine. It’s the only way to be 100% sure about how to tell if there is blood in your stool and, more importantly, why it is there.
There are also CT scans or capsules you can swallow that take pictures, but those are usually secondary options.
Actionable Steps to Take Right Now
If you noticed something suspicious today, do not just flush and forget.
- Check the "Input": Write down everything you ate in the last 24 hours. If it includes beets, red dye, or iron, breathe.
- Take a Photo: It feels weird. It feels gross. Do it anyway. Showing a photo to your doctor is a thousand times more helpful than trying to describe a shade of red.
- Monitor Your Energy: Are you more tired than usual? Short of breath? These are signs of slow, chronic blood loss.
- Check Your Meds: Are you taking a lot of NSAIDs like ibuprofen or aspirin? These can cause stomach ulcers that bleed.
- Schedule a FIT Test: If you’re over 45, or even younger with symptoms, ask your doctor for an at-home screening kit as a first step.
The most important thing is to stop Googling and start tracking. Keep a small log for three days. Note the color, the frequency, and any associated pain. If the bleeding persists for more than two days or happens more than once a month, make the appointment. Most causes are benign and easily treatable, but the peace of mind is worth the awkward conversation.