Forgetfulness is a bit of a running joke once you hit fifty. You walk into a room, stare at the wall, and realize you have absolutely no idea why you’re there. We laugh it off. We blame "senior moments" or a lack of coffee. But for some, that mental fog isn't just a byproduct of a busy life; it’s the quiet beginning of something much heavier. Understanding the symptoms of early alzheimer's isn't about fear-mongering. It’s about clarity.
Honestly, the line between normal aging and cognitive decline is thinner than people like to admit.
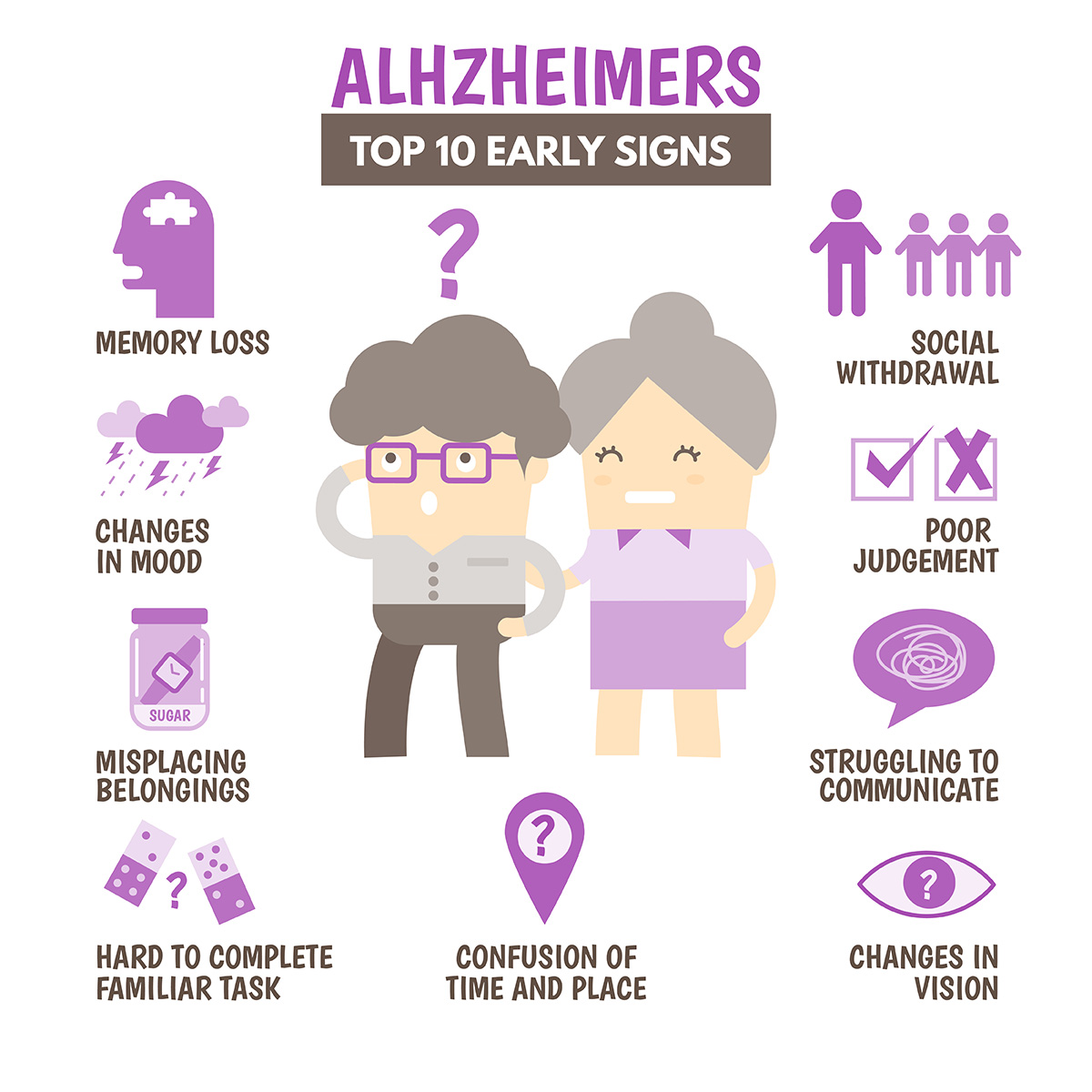
Doctors at the Mayo Clinic often point out that the biggest red flag isn't just forgetting a name—it's forgetting the context of the person entirely. If you forget where you put your keys, you’re human. If you find those keys in the freezer and have no memory of how they got there, that’s a different conversation. This distinction matters because early intervention actually does something these days. We aren't in the dark ages of neurology anymore.
The Memory Myth and What Actually Happens
Everyone thinks Alzheimer’s is just "forgetting stuff." It’s not. It’s a breakdown of the brain's ability to process new data.
In the early stages, specifically what clinicians call Mild Cognitive Impairment (MCI) due to Alzheimer's, the brain's hippocampus starts to struggle. This is your "save button." When it fails, short-term memories never become long-term ones. You might remember the lyrics to a song from 1974 with perfect precision, yet struggle to recall what you ate for breakfast twenty minutes ago. It's frustrating. It's scary. And it’s incredibly subtle at first.
You might notice a loved one asking the same question three times in one conversation. They aren't trying to be difficult. Their brain literally didn't "write" the answer to the hard drive the first two times.
Why "Typical Aging" is a Bad Excuse
We tend to excuse away the symptoms of early alzheimer's because we want to be polite. Or because we're terrified.
- Normal aging: Forgetting which day it is but remembering it later.
- Early Alzheimer’s: Losing track of the season or the year entirely.
- Normal aging: Making a bad decision once in a while.
- Early Alzheimer’s: Consistently showing poor judgment, like giving away huge sums of money to telemarketers or wearing a heavy coat in a heatwave.
See the difference? It’s the consistency and the impact on daily life that shifts the diagnosis.
The "Executive Function" Collapse
Most people don't talk about the "planning" aspect. This is huge.
🔗 Read more: Creatine Explained: What Most People Get Wrong About the World's Most Popular Supplement
The frontal lobe handles your executive function. Think of it as the conductor of an orchestra. When Alzheimer's starts to creep in, the conductor leaves the podium. Suddenly, following a recipe—something you've done for thirty years—becomes a Herculean task. You miss steps. You get confused by the sequence. Managing a monthly budget or keeping track of bills starts to feel like solving a complex physics equation.
I’ve seen patients who were brilliant accountants suddenly struggle to calculate a 15% tip at a restaurant. It’s not that they forgot math. It’s that the brain can no longer hold multiple pieces of information at once to complete a multi-step task.
Vision and Spatial Awareness: The Symptoms Nobody Mentions
This is where it gets weird. Alzheimer’s isn't just a "memory disease." It’s a brain disease.
For some, the first symptoms of early alzheimer's show up in the visual cortex. This is often called Posterior Cortical Atrophy (PCA). You might have perfect 20/20 vision, but your brain can't interpret what your eyes see. Reading becomes difficult because the words seem to jump around. Judging distance becomes a nightmare.
Imagine reaching for a coffee cup and missing it by three inches. Or worse, struggling to drive because you can't tell how far away the car in front of you actually is. People often visit an eye doctor first, thinking they need new glasses, only to find out their eyes are fine—it’s the processing unit that's glitching.
Personality Flips and the Social "Filter"
Have you ever met someone who was always mild-mannered and suddenly started snapping at people? Or maybe someone who was a social butterfly but now refuses to leave the house?
Apathy is actually one of the most common early signs. It’s not depression, though it looks like it. It’s a loss of "get-up-and-go" caused by changes in the brain's reward system. A person might lose interest in hobbies, sports, or seeing grandchildren. They aren't sad, necessarily. They just... don't care.
Then there’s the loss of the social filter. The brain’s ability to inhibit inappropriate thoughts starts to erode. My friend’s father, a man who never uttered a swear word in his life, started using colorful language in the middle of Sunday brunch. It was shocking for the family. But biologically, it made sense. The "brakes" in his brain were failing.
💡 You might also like: Blackhead Removal Tools: What You’re Probably Doing Wrong and How to Fix It
The Science of "Self-Correction"
One fascinating thing experts look for is whether a person can "self-correct."
If you trip over a word—say you call a "watch" a "hand-clock"—and you immediately realize it and fix it, that’s usually just brain fog or fatigue. In the early stages of Alzheimer’s, that self-correction starts to vanish. A person might use the wrong word and have no idea they did it. Or they might stop in the middle of a sentence because they’ve completely lost the thread of what they were saying. We call this "aphasia." It’s basically the brain's dictionary getting its pages ripped out one by one.
Is it Always Alzheimer's?
No.
And this is vital. A lot of things mimic the symptoms of early alzheimer's.
- Vitamin B12 Deficiency: Believe it or not, low B12 can cause memory loss and confusion that looks exactly like dementia. It’s often reversible with shots or supplements.
- Thyroid Issues: An underactive thyroid slows everything down, including your brain.
- Depression: "Pseudodementia" is a real thing. Severe depression can cause cognitive "slowness" that mimics early-stage Alzheimer's.
- UTIs in Seniors: This is a big one. An untreated urinary tract infection in an older adult can cause sudden, intense confusion and hallucinations.
This is why you don't self-diagnose via Google. You go to a neurologist. You get the blood work. You get the imaging.
The Role of Genetics vs. Lifestyle
"My grandmother had it, so I'm doomed, right?"
Not necessarily. While the APOE-ε4 gene can increase your risk, it isn't a guarantee. Most cases are "sporadic," meaning they happen due to a complex mix of age, environment, and lifestyle. According to the Lancet Commission on Dementia, nearly 40% of dementia cases could potentially be delayed or prevented by addressing risk factors like hearing loss, hypertension, and social isolation.
Yes, hearing loss. If your brain is constantly struggling to decode muffled sounds, it has less "power" left over for memory. It’s like running too many apps on an old phone. Eventually, the whole system crashes.
📖 Related: 2025 Radioactive Shrimp Recall: What Really Happened With Your Frozen Seafood
What to Do if You’re Worried
If you’re noticing these patterns in yourself or someone you love, stop waiting for it to "get better." It rarely just goes away.
First, start a log. Note the specific behaviors. Not just "Mom was confused," but "Mom forgot how to use the microwave on Tuesday." This data is gold for a doctor.
Second, get a "Mini-Mental State Exam" (MMSE) or a MoCA test. These are short, 10-minute screenings that check orientation, recall, and attention. They aren't perfect, but they’re a great baseline.
Third, look into new treatments. The FDA has recently approved drugs like Leqembi (lecanemab) and Kisunla (donanemab). These aren't "cures"—let’s be very clear about that—but they are the first medications that actually target the amyloid plaques in the brain to slow down the progression. They only work in the early stages. That’s why catching the symptoms of early alzheimer's early is so life-changing.
Actionable Steps for Cognitive Health
Don't just sit there and worry. Take control of the variables you can actually change.
- Fix your sleep. During deep sleep, your brain’s glymphatic system literally "washes" out toxins, including the beta-amyloid proteins linked to Alzheimer’s. If you have sleep apnea, treat it.
- Move your body. Exercise increases Brain-Derived Neurotrophic Factor (BDNF), which is basically Miracle-Gro for your brain cells. Even a 20-minute brisk walk changes your brain chemistry.
- Audit your social life. Isolation is toxic to the brain. Join a club, volunteer, or just call a friend. The complex interaction of conversation is a massive workout for your neurons.
- Manage vascular health. What's good for the heart is good for the brain. High blood pressure damages the tiny vessels in your brain, leading to "white matter disease," which accelerates cognitive decline.
- Get a professional baseline. If you’re over 65, ask for a cognitive screening during your annual Medicare wellness visit. It’s free, and it gives you a point of comparison for the future.
The goal isn't to live in fear of a diagnosis. It's to live with enough awareness that you can advocate for yourself or your family. We are entering an era where Alzheimer's might become a manageable chronic condition rather than a mysterious, unstoppable force. But that shift starts with recognizing the signs before they become impossible to ignore.
Next Steps for Action
- Schedule a physical: Ask specifically for a Vitamin B12 and thyroid panel to rule out reversible causes of brain fog.
- Download a cognitive app: Use something like the SAGE test (developed by Ohio State University) which can be taken at home to see if a formal doctor's visit is warranted.
- Update your hearing aids: If you or a loved one is struggling to hear, prioritize an audiology appointment immediately to reduce cognitive load.
- Review medications: Some "anticholinergic" drugs (like certain over-the-counter sleep aids or allergy meds) can actually worsen memory symptoms; ask a pharmacist to review your list.