You just sat down, the cuff squeezed your arm, and the screen flashed: 113/83. Most people look at that top number, the 113, and breathe a sigh of relief because it’s comfortably under the "magic" 120 mark. But then there is that 83. It feels a little... off? Maybe a bit high compared to the first number? Honestly, it is.
Blood pressure is a weird, oscillating measurement of your life force. It isn't static. It’s a snapshot of a single second in time. When we talk about blood pressure 113 83, we are looking at a specific physiological puzzle that doesn't quite fit the "perfect" 120/80 mold.
The split personality of blood pressure 113 83
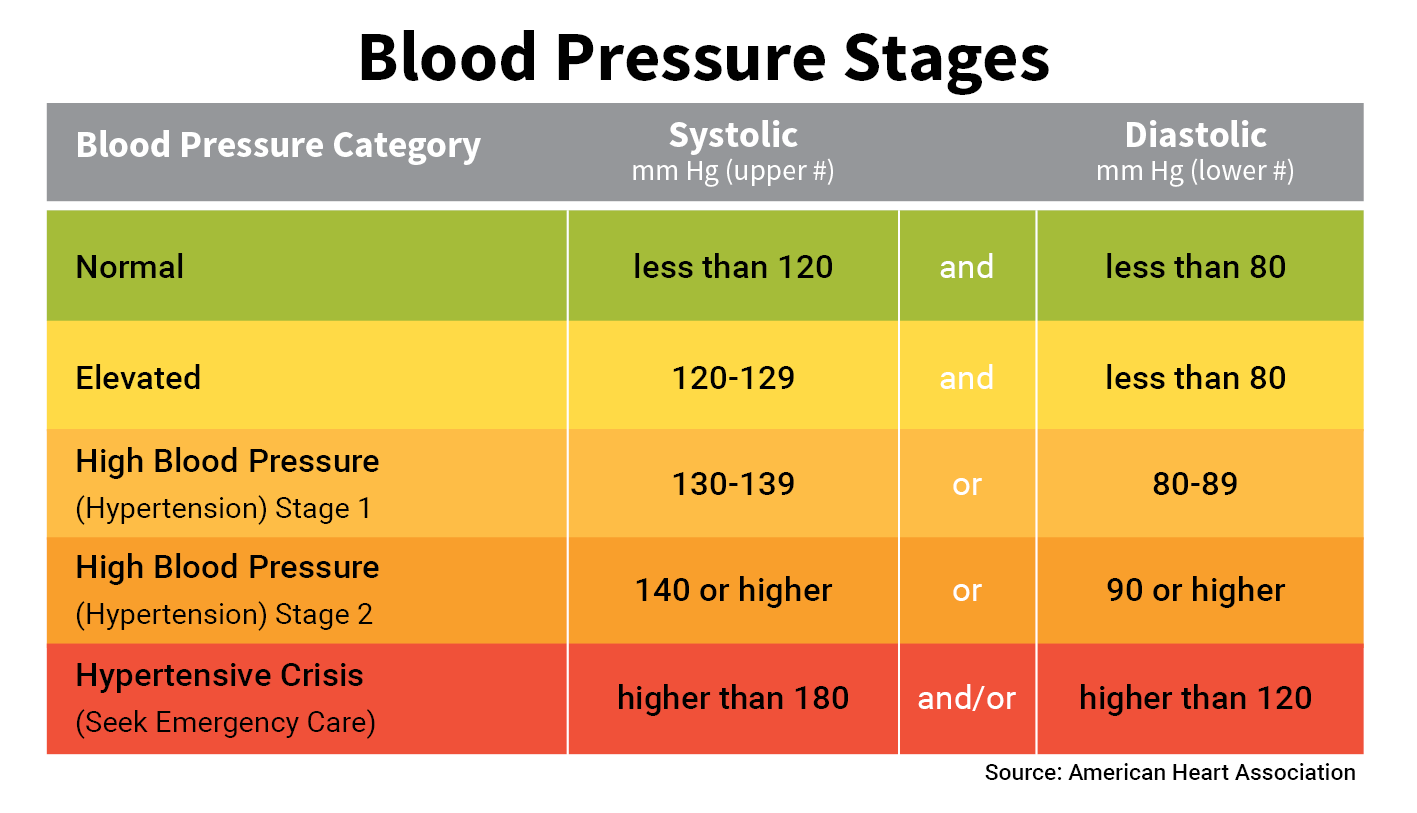
What are we actually looking at here? Your systolic pressure—the top number—is 113 mmHg. That is excellent. It means when your heart beats, the pressure against your artery walls is well within the "normal" range defined by the American Heart Association (AHA). You’re winning there. But the 83? That is your diastolic pressure. That is the pressure in your arteries when your heart is resting between beats.
Anything over 80 for that bottom number technically nudges you into the "Stage 1 Hypertension" category, regardless of how good that top number looks. It's a bit of a medical contradiction. You have one foot in the "ideal" zone and one foot in the "we should probably watch this" zone.
Why the diastolic number matters more than you think
We spent decades obsessing over the systolic number. Doctors used to say that as long as the top number was low, the bottom one didn't matter much for older adults. We were wrong. Recent data, including large-scale longitudinal studies published in the New England Journal of Medicine, suggests that both numbers independently predict cardiovascular risk.
If your diastolic is consistently 83, your heart is working slightly harder than it should even when it's supposed to be "off duty." Imagine a garden hose. If the water is always turned on just a little bit too high, even when you aren't spraying the lawn, the hose wears out faster. That is basically what is happening to your blood vessels.
Is 113/83 a sign of "Isolated Diastolic Hypertension"?
Isolated Diastolic Hypertension (IDH) is a specific condition where the systolic is normal but the diastolic is high. While blood pressure 113 83 isn't extreme IDH, it's the gateway.
You see this a lot in younger adults. Usually, people under 45 are more likely to have a higher diastolic number while their systolic stays low. It often stems from a high "total peripheral resistance." Basically, your smaller blood vessels are a bit more constricted than they ought to be. Why? It could be stress. It could be too much salt. It might just be your genetics playing a prank on you.
Dr. Paul Whelton, a lead author of the 2017 AHA/ACC guidelines, has pointed out that the shift to 80 as the cutoff for "normal" was intentional. It wasn't to put more people on meds. It was to wake people up. If you are sitting at 83, you aren't "sick," but you are on a trajectory.
💡 You might also like: Resistance Bands Workout: Why Your Gym Memberships Are Feeling Extra Expensive Lately
The "White Coat" factor and measurement errors
Let's get real for a second. Did you take this measurement at the doctor's office? If so, it might be fake news.
White Coat Hypertension is a real thing where your blood pressure spikes just because a person in a lab coat is staring at you. But there’s also "Masked Hypertension," where it's normal at the doctor but high at home. If you got a blood pressure 113 83 reading, you need to consider the context.
Did you:
- Talk while the machine was running? (Adds 10 points)
- Cross your legs? (Adds 5 points)
- Have a full bladder? (Adds 10-15 points)
- Drink coffee an hour before?
If you didn't sit in a chair with back support, feet flat on the floor, and arm at heart level for five minutes before hitting start, that 83 might actually be a 78. Or it could be an 88. Precision matters. One single reading of 113/83 is almost meaningless. It is the average over a week that tells the story of your heart.
The lifestyle culprits you're probably ignoring
Salt is the obvious villain. We all know it. But for the diastolic number, alcohol and sleep apnea are often the hidden triggers.
Alcohol is a weird one. It might relax you in the moment, but as your body processes it, your blood pressure often rebounds higher, especially the diastolic. If you had a couple of glasses of wine last night and measured 113/83 this morning, there's your answer.
Then there's sleep. If you snore or wake up feeling like a zombie, you might have sleep apnea. This causes repeated spikes in blood pressure throughout the night. Your body never truly gets that "diastolic dip" it needs. Over time, your baseline settles at a higher number, like 83, even when you're awake and calm.
When should you actually worry about 113/83?
Context is everything. If you are 25 years old, fit, and have no other health issues, a blood pressure 113 83 reading is mostly a "hey, keep an eye on this" moment. You probably just need to cut back on the processed snacks and maybe do a bit more cardio.
📖 Related: Core Fitness Adjustable Dumbbell Weight Set: Why These Specific Weights Are Still Topping the Charts
However, if you have diabetes, chronic kidney disease, or a family history of early strokes, that 83 is a bigger deal. The "sprint" trial—a massive study that changed how we look at BP—showed that getting numbers lower (closer to 120/80) significantly reduced the risk of heart failure and death in high-risk patients.
The salt sensitivity trap
Some people are "salt sensitive." It’s a genetic lottery. About half the people with high blood pressure are salt sensitive. For these folks, a single salty meal can keep their diastolic pressure elevated for a day or more.
If you want to test this, try a "low salt week." Aim for under 1,500mg of sodium a day. It's hard. It's basically impossible if you eat out. But if you do it and your 83 drops to a 77, you’ve found your culprit. You don't need a pill; you just need to stop the salt.
Potassium: The secret weapon
Everyone talks about cutting salt, but nobody talks about upping potassium. Potassium helps your body flush out sodium and eases the tension in your blood vessel walls.
Think of it as the antidote. Avocados, bananas, spinach, and sweet potatoes. If you're hitting blood pressure 113 83, increasing your potassium intake might be the fastest way to nudge that 83 back into the 70s without ever touching a prescription bottle.
Moving beyond the numbers
We get so caught up in the digits that we forget what blood pressure actually represents. It’s a measure of arterial health and autonomic nervous system balance.
If your reading is 113/83, your "Pulse Pressure" is 30 (113 minus 83). A pulse pressure of 30 to 40 is generally considered healthy. It suggests your arteries are still quite flexible. If that gap gets too narrow (like 110/95) or too wide (like 160/70), that is when cardiologists start getting really nervous.
So, in the grand scheme of things, 113/83 isn't a "red alert." It's more like a "yellow light." It’s your body's way of saying, "I'm doing okay, but I'm starting to feel the strain."
👉 See also: Why Doing Leg Lifts on a Pull Up Bar is Harder Than You Think
Actionable steps to manage 113/83
Don't panic. Seriously. Stressing about a blood pressure reading will literally make the reading worse. It’s a vicious cycle.
Instead, take a systematic approach to see if this is a fluke or a trend.
- Buy a validated home monitor. Look for one that is "clinically validated." Brands like Omron or Withings are usually solid. Avoid the wrist cuffs; they are notoriously finicky.
- The 7-7-7 Rule. Measure your blood pressure for 7 days. Twice in the morning, twice in the evening. Ignore the first day. Average the rest. If your average is still showing a diastolic above 80, it's time to talk to a professional.
- Magnesium supplementation. Many people are deficient in magnesium, which acts as a natural calcium channel blocker to relax blood vessels. Talk to your doctor, but a standard 200-400mg dose of Magnesium Glycinate can often shave a few points off that diastolic number.
- Zone 2 Cardio. You don't need to run a marathon. Just 30 minutes of brisk walking where you can still hold a conversation but feel slightly breathless. This strengthens the heart muscle, meaning it doesn't have to work as hard during that "diastolic" rest phase.
- Watch the NSAIDs. If you're popping Ibuprofen or Naproxen for back pain or headaches, stop. These drugs are notorious for raising blood pressure by causing the body to retain fluid and constricting blood vessels.
The final verdict
A reading of blood pressure 113 83 is a nudge. It’s not a diagnosis of a life-threatening illness, but it is an invitation to look at your habits.
You've got a great systolic number. You've got the foundation of a healthy heart. Now you just need to focus on the "rest" phase. Lower the resistance in your system, feed your body the right minerals, and give yourself a break.
Most of the time, that 83 is just a symptom of a modern, high-stress, high-sodium life. It's reversible. It's manageable. And now that you know what it means, it's something you can actually fix.
Check your equipment first. Ensure the cuff size is correct for your arm—a cuff that's too small will give you a falsely high reading every single time. If the cuff fits and the numbers stay in the 83-85 range, start with the potassium and the walking. You'll likely see that number dip back into the 70s within a month.
Next Steps for Monitoring:
- Log your readings for one week in a dedicated notebook or app to identify patterns.
- Schedule a consultation with a primary care physician if your average diastolic remains above 80 after two weeks of lifestyle adjustments.
- Review your current medications and supplements with a pharmacist to check for hidden blood pressure elevators.