Death is the only thing we all have in common, yet we’re terrible at talking about how it actually happens. When people start asking is assisted suicide legal in the United States, they usually aren't looking for a dry legal textbook. They're often facing a terrifying diagnosis—either for themselves or someone they love—and they want to know what their options are before things get unbearable.
The short answer? It depends entirely on which side of a state line you're standing on.
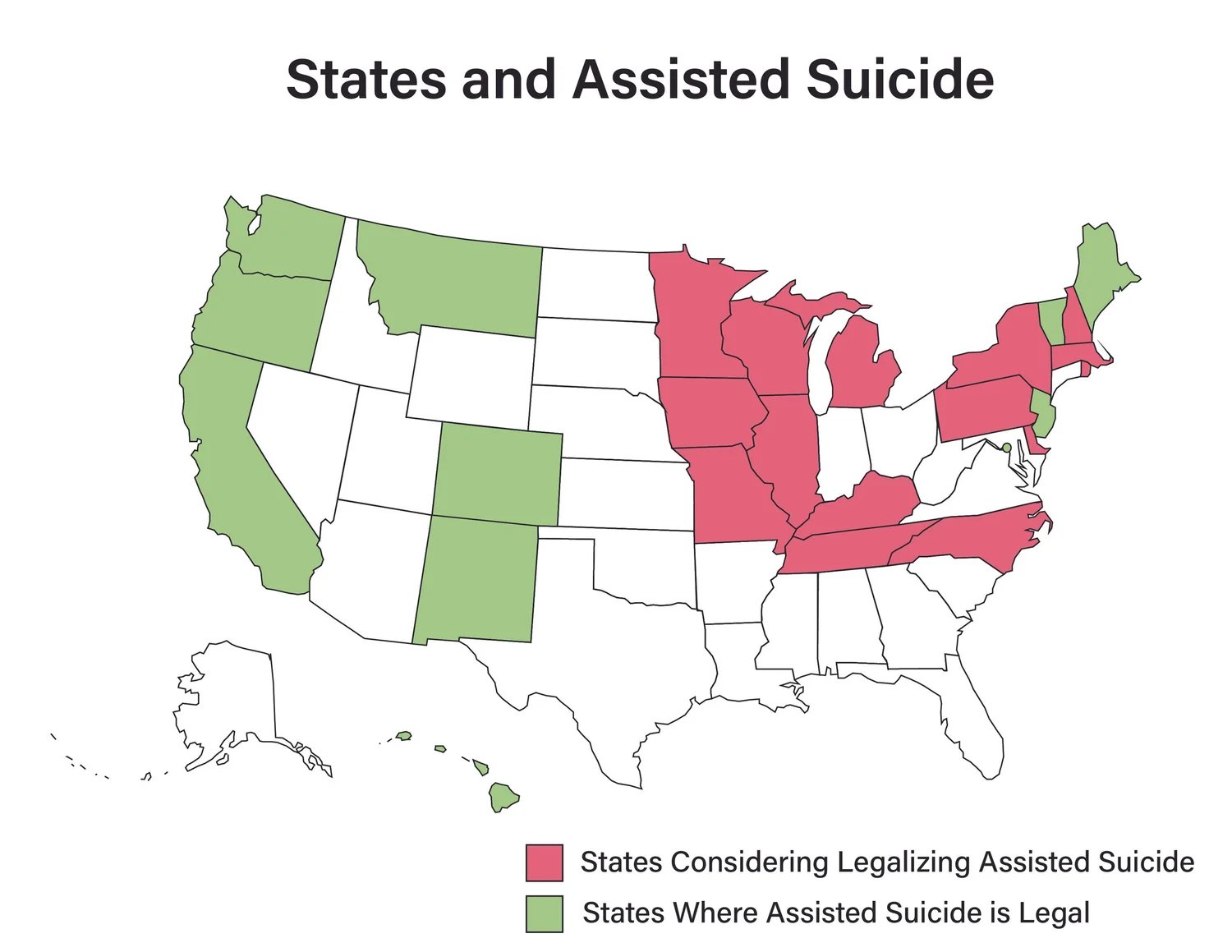
Right now, the map of the U.S. is a patchwork of "Death with Dignity" laws. Some states embrace it. Others will throw a doctor in prison for it. It’s complicated, emotional, and honestly, a bit of a bureaucratic nightmare for families in the middle of a crisis.
Where Can You Actually Do This?
Let’s get the geography out of the way first. You can’t just walk into a clinic in any state and ask to end your life. That's not how this works. As of early 2026, medical aid in dying (MAID) is legal in several jurisdictions, including Oregon, Washington, California, Montana, Vermont, New Mexico, Hawaii, New Jersey, Maine, and the District of Columbia.
Oregon was the pioneer. They passed the Oregon Death with Dignity Act way back in 1994, though it didn't actually go into effect until 1997 because of a mountain of legal challenges. Since then, the "Oregon model" has basically become the blueprint for every other state that has followed suit.
In Montana, it’s a weird outlier. There is no specific statute or law passed by the legislature. Instead, a 2009 State Supreme Court ruling in Baxter v. Montana basically said that state law doesn't prohibit a doctor from honoring a terminally ill patient's request for life-ending medication. It’s a legal protection for doctors rather than a codified "right" for patients, which makes it feel a bit more precarious than the systems in place in places like Colorado or California.
The "Death with Dignity" vs. "Assisted Suicide" Debate
Language matters here. If you talk to a supporter, they will never use the word "suicide." They call it Medical Aid in Dying or MAID. Why? Because they argue that "suicide" implies a mental health crisis or a desire to die when you could otherwise live. These patients don't want to die; they are already dying.
Opponents, including many religious groups and some disability rights advocates, stick firmly to "assisted suicide." They worry that "normalizing" the practice creates a "slippery slope" where the elderly or disabled might feel pressured to end their lives to avoid being a "burden" to their families or the healthcare system.
✨ Don't miss: Fruits that are good to lose weight: What you’re actually missing
The Strict Rules Nobody Tells You About
People think you just get a prescription and that’s it. It is so much harder than that. To qualify under the laws in states like California or Maine, you have to jump through a series of very specific, very rigid hoops.
First, you have to be an adult. Sorry, no minors. You have to be a resident of the state (though this is changing, which I'll get into in a second). Most importantly, you must be terminally ill with a prognosis of six months or less to live. This has to be confirmed by two different doctors.
You also have to be "of sound mind." This is where it gets heartbreaking. If you have advanced Alzheimer’s or dementia, you're usually disqualified. By the time you might want the medication, you are no longer considered capable of making the decision. It's a cruel catch-22 that leaves many families in a lurch.
And you have to be able to self-administer the drug. The doctor can't inject you. Your spouse can't pour it down your throat. You have to be the one to swallow the liquid or push the plunger on a feeding tube. If you lose the physical ability to swallow before the paperwork clears, the option vanishes.
The Residency "Loophole" is Opening Up
For years, if you lived in a state where it was illegal, you were basically out of luck unless you were wealthy enough to move to Portland or Seattle and establish residency for months.
That’s shifting.
Vermont and Oregon have recently settled lawsuits that challenged the residency requirement. Basically, they’ve stopped enforcing the rule that you have to be a resident to use their laws. In theory, this means someone from Idaho could travel to Oregon to access the medication. But—and this is a huge "but"—many doctors are still terrified of the legal ramifications of helping out-of-state patients, especially with federal laws regarding controlled substances.
🔗 Read more: Resistance Bands Workout: Why Your Gym Memberships Are Feeling Extra Expensive Lately
What Actually Happens in the Room?
The process isn't like the movies. It’s not a quick "switch off."
Usually, the patient is prescribed a high dose of barbiturates or a compound of several medications. It’s often a powder that has to be mixed into a small amount of juice or applesauce. Because the drugs taste incredibly bitter—borderline caustic—doctors often suggest eating a spoonful of sorbet or drinking a bit of schnapps right before and after to mask the flavor.
Once you take it, you usually fall into a deep sleep within minutes. Then a coma. Then, eventually, the heart stops. It can take 20 minutes; it can take four hours. It’s unpredictable.
One thing people rarely talk about is the cost. Medicare doesn't cover this because it's a federal program and assisted suicide is illegal at the federal level. Private insurance might cover it, but many don't. The drugs themselves have skyrocketed in price over the last decade, sometimes costing $3,000 to $5,000 for a single dose.
Why Doctors are Often the Biggest Hurdle
Even in a state where the answer to is assisted suicide legal in the United States is a resounding "yes," finding a doctor to help is a struggle.
Many hospital systems, especially those with religious affiliations (like Catholic hospital networks, which own a massive chunk of the U.S. healthcare market), strictly forbid their doctors from participating. A doctor might personally support your choice but be contractually prohibited from writing the script.
There's also the "conscientious objection" clause. No doctor is ever required to participate. Many find it fundamentally at odds with the Hippocratic Oath. Finding a "willing provider" often requires calling around to non-profits like Compassion & Choices just to find a lead.
💡 You might also like: Core Fitness Adjustable Dumbbell Weight Set: Why These Specific Weights Are Still Topping the Charts
The Moral and Social Friction
We can't ignore the pushback. Groups like Not Dead Yet argue that the healthcare system is already biased against people with disabilities. They fear that insurance companies might see "assisted death" as a cheaper alternative to expensive long-term care or complex surgeries.
Then there’s the "Slippery Slope" argument. Look at Canada. Their "MAID" laws have expanded significantly, and there are reports of people seeking assisted death because they are poor or homeless. That scares the hell out of people in the U.S. It’s why the American laws are so much stricter—proponents are terrified that if they let the rules loosen even a little, the whole thing will be struck down.
What You Should Actually Do Now
If you or a family member are considering this, don't wait. Time is your biggest enemy here because of the "mental capacity" requirements and the "six-month" rule.
First, talk to your current doctor. Ask them point-blank: "If I reached a point of terminal suffering, would you be willing to support me under the Death with Dignity Act?" Get a straight answer. If they say no, or if they're "unsure," you need to find a different doctor immediately.
Second, check your state’s specific timeline. Most states require two oral requests separated by a waiting period (usually 15 days, though some states like California have shortened this to 48 hours in "urgent" cases). Then you need a written request. If you wait until you're in the final days of life, you'll never make the deadline.
Third, document everything. Make sure your Advance Directive and Power of Attorney are updated. Even if you don't use MAID, having your wishes in writing is the only way to ensure you don't end up on a ventilator against your will.
The legal landscape is moving fast. In 2026, we’re seeing more states like New York and Maryland debating these bills. It’s no longer a fringe issue. It’s a mainstream medical conversation.
Practical Steps to Take:
- Visit Compassion & Choices or Death with Dignity National Center. These are the two biggest organizations that track state-by-state legality and can help you find doctors who participate.
- Verify your insurance. Call your provider and ask specifically about "medical aid in dying" coverage. Don't use the word suicide; use the legal medical term.
- Establish a backup plan. If your state doesn't allow it, look into "Voluntary Stopping of Eating and Drinking" (VSED). It's legal in all 50 states and doesn't require a doctor's prescription, though it requires intense hospice support.
- Talk to a palliative care specialist. They aren't the same as hospice. Palliative care focuses on pain management while you’re still seeking treatment, and they are usually the most honest about what the end-of-life process looks like.
Knowing whether is assisted suicide legal in the United States is just the first step. Navigating the actual system is the real marathon. Be proactive, be annoying with your questions, and don't let the paperwork outrun your health.