You’re sitting on the couch, maybe scrolling through your phone, and you feel that familiar rhythmic thump in your chest. You check your Apple Watch or press two fingers against your wrist. The number flashes up: 75.
It’s a common number. Average, even. But is a heart rate 75 per minute actually where you want to be?
Most people are taught that anything between 60 and 100 beats per minute (bpm) is "normal." That’s a massive range. It’s like saying any temperature between 40 and 100 degrees is "weather." Technically true, but the lived experience is vastly different. While 75 bpm won't send you to the emergency room, modern cardiology suggests it’s a bit more nuanced than just staying under the 100-bpm speed limit.
The Myth of the 60-100 Range
We need to talk about why that "normal" range is so wide. It was established decades ago as a clinical baseline to identify extreme pathology—tachycardia (too fast) or bradycardia (too slow). It wasn't designed to define "optimal" health.
If your resting heart rate 75 per minute is your daily baseline, you're smack in the middle. You're safe. You’re fine. But "fine" is different from "thriving."
Research, including the landmark Framingham Heart Study, has hinted for years that resting heart rates on the higher end of the normal spectrum might correlate with different long-term outcomes than those on the lower end. Dr. Deepak Bhatt, a top cardiologist at Brigham and Women's Hospital, often notes that a rising resting heart rate over time can be a more significant "red flag" than the specific number itself.
Think of it this way. Your heart is a pump. If it pumps 75 times every minute instead of 60, that’s 15 extra beats per minute. Over an hour, that’s 900 extra beats. Over a year? About 7.8 million extra thumps. That’s a lot of extra work for a muscle that never gets a vacation.
Why Your Heart Rate 75 Per Minute Might Change
Context is everything. Honestly, your heart rate is a total gossip; it tells everyone exactly how your body is reacting to the world.
📖 Related: Does Ginger Ale Help With Upset Stomach? Why Your Soda Habit Might Be Making Things Worse
If you just finished a cup of coffee, 75 is actually pretty low. Caffeine blocks adenosine receptors, which usually keep things calm. If you’re dehydrated, your blood volume drops, making the heart beat faster to move the remaining fluid around. In that case, a heart rate 75 per minute might actually be your heart struggling a bit to keep up.
Then there’s the "White Coat Effect." Many people see 75 at the doctor’s office but 62 at home. Stress hormones like cortisol and adrenaline act like a foot on the gas pedal. If you're stressed at work, your sympathetic nervous system is likely keeping you at that 75 mark. It’s the "fight or flight" mode on a low simmer.
The Fitness Paradox
Athletes often brag about resting heart rates in the 40s or 50s. Why? Because their heart muscle is so strong it can move a huge volume of blood in a single, powerful squeeze (high stroke volume).
If you aren't an endurance athlete, having a heart rate 75 per minute is perfectly respectable. It means your heart is functioning efficiently enough that it doesn't need to race, but it’s likely not "athletically conditioned" in the cardiovascular sense. And that’s okay. Most of us aren't training for the Tour de France.
When 75 bpm Is a Sign of Something Else
We have to look at the outliers. Sometimes, a steady 75 isn't just a number; it's a symptom.
- Thyroid Function: An overactive thyroid (hyperthyroidism) can kick your metabolism into overdrive. Even a "normal" 75 could be a jump if you used to sit at 60.
- Anemia: If your blood doesn't have enough iron, it can't carry oxygen effectively. Your heart compensates by beating more often.
- Poor Sleep: Chronic sleep deprivation keeps your nervous system "up." You never truly drop into that deep, restorative bradycardia that happens during REM and deep sleep stages.
Digging Into the Data: Is Lower Always Better?
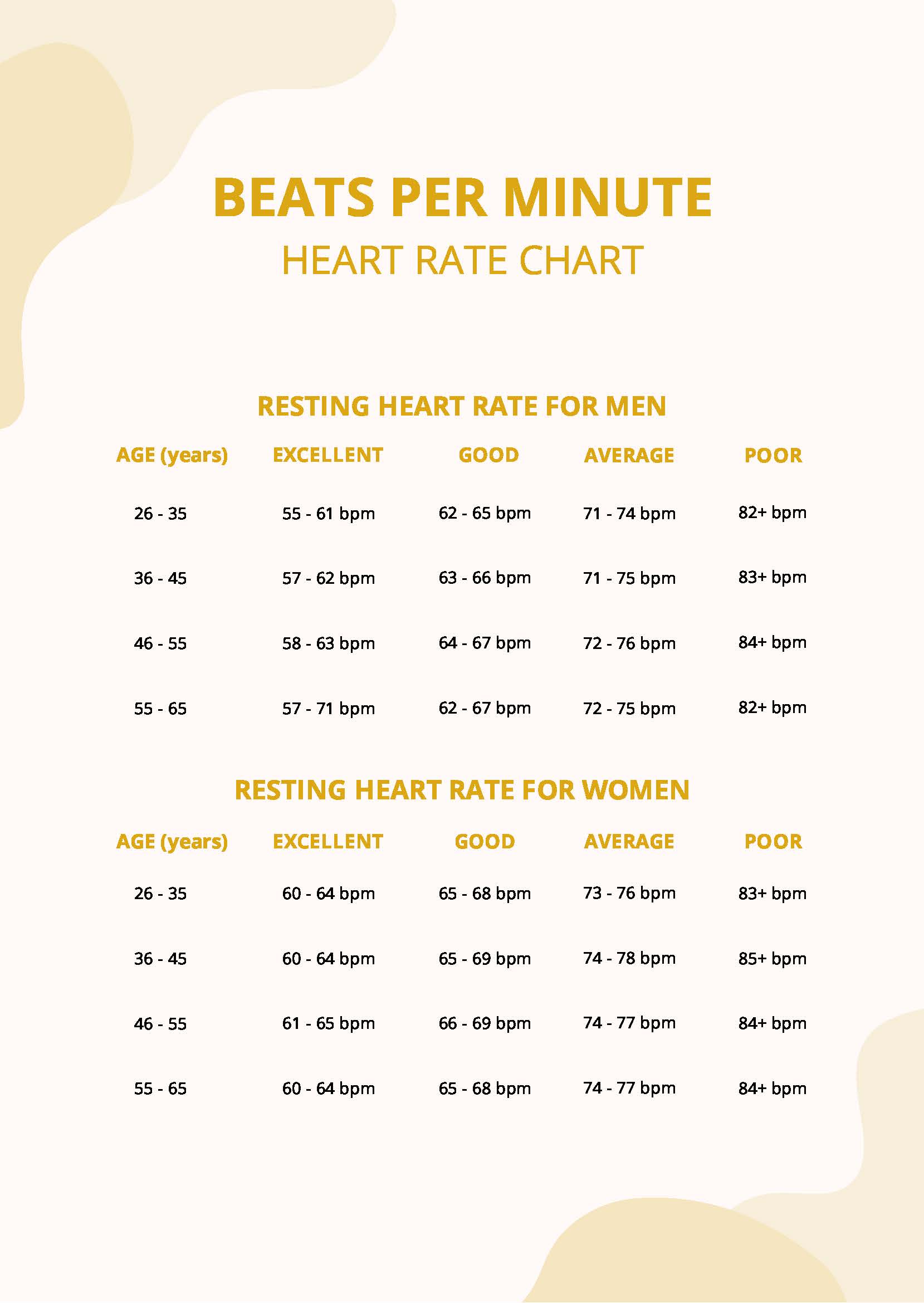
There’s a bit of a debate in the medical community about the "longevity sweet spot." Some studies, like those published in the journal Open Heart, suggested that for middle-aged men, a resting heart rate of 75 or higher was associated with a higher risk of cardiovascular issues compared to those at 55 bpm.
But wait. Correlation isn't causation.
👉 See also: Horizon Treadmill 7.0 AT: What Most People Get Wrong
People with higher heart rates might also sit more, eat more processed foods, or deal with higher systemic inflammation. A heart rate 75 per minute isn't a death sentence—it's just a data point. It’s a "check engine" light that might just mean you need an oil change, not a new engine.
How to Actually Lower Your Resting Heart Rate
If you're looking at that 75 and thinking, "I'd rather see a 65," you can actually change it. It’s not a fixed setting like your height.
First, look at your magnesium levels. Most people are deficient. Magnesium helps the heart's electrical system stay stable. Without it, the "firing" mechanism can get a little twitchy.
Second, Zone 2 cardio. This is the magic pill. It’s exercise where you can still hold a conversation but you're definitely working. Think of a brisk walk where you're slightly out of breath. Doing this for 150 minutes a week strengthens the heart muscle, eventually lowering your heart rate 75 per minute down into the 60s.
Third, hydration. Seriously. Drink more water. When you're dehydrated, your blood is thicker. Thicker blood is harder to pump. It’s basic physics.
The Alcohol Factor
This is the one nobody likes to hear. Alcohol is a massive heart rate spike. Even one glass of wine can keep your resting heart rate elevated by 5-10 beats for several hours, often persisting through the night. If you’re checking your pulse the morning after a cocktail, that heart rate 75 per minute might actually be 10 beats higher than your true baseline.
Listening to the Rhythm, Not Just the Count
A number is just a number. What matters more is the "regularity."
✨ Don't miss: How to Treat Uneven Skin Tone Without Wasting a Fortune on TikTok Trends
Is your heart rate a steady thump-thump, thump-thump? Or does it feel like a jazz drummer having a mid-life crisis? If 75 bpm comes with palpitations, a feeling of "skipping" beats (PVCs), or lightheadedness, the 75 doesn't matter nearly as much as the arrhythmia.
If you feel "flip-flops" in your chest, that’s when you call the cardiologist. They’ll likely order an EKG or a Holter monitor to see what's happening behind the scenes.
Actionable Steps for Your Heart Health
Don't panic about 75. It's a solid, middle-of-the-road number. But if you want to optimize your cardiovascular health and potentially lower that number for better long-term efficiency, here is the blueprint.
Monitor your trends. Don't just look at a single snapshot. Use a wearable or a manual log to track your heart rate first thing in the morning, before you get out of bed. This is your true "Resting Heart Rate" (RHR). If it stays at a heart rate 75 per minute consistently, that’s your baseline. If it starts creeping up to 80 or 85 over a month, look at your stress or recovery levels.
Prioritize Vagal Tone. The vagus nerve is like the brake pedal for your heart. You can "train" it using deep belly breathing or cold exposure (like ending your shower with 30 seconds of cold water). This stimulates the parasympathetic nervous system, which naturally draws the heart rate down.
Focus on Mineral Balance. It's not just about salt; it's about the ratio of sodium to potassium and magnesium. Leafy greens, avocados, and nuts provide the electrolytes your heart needs to maintain a calm, efficient rhythm.
Assess your "hidden" stimulants. Check your supplements. Many pre-workouts, weight loss pills, or even some decongestants contain ingredients that artificially inflate your heart rate.
Basically, 75 is a "green light" for daily activity, but it’s a "yellow light" for long-term optimization. It means you’re doing okay, but there’s room to improve your heart's efficiency. Focus on the inputs—sleep, hydration, and steady movement— and the output will take care of itself.