You’re sitting in that small, sterile exam room. The cuff squeezes your arm until it pulses, the Velcro rips, and the nurse mumbles "140 over 70." They might not even look up from the chart. But for you, those numbers feel like a giant question mark hanging in the air.
Is 140/70 high blood pressure?
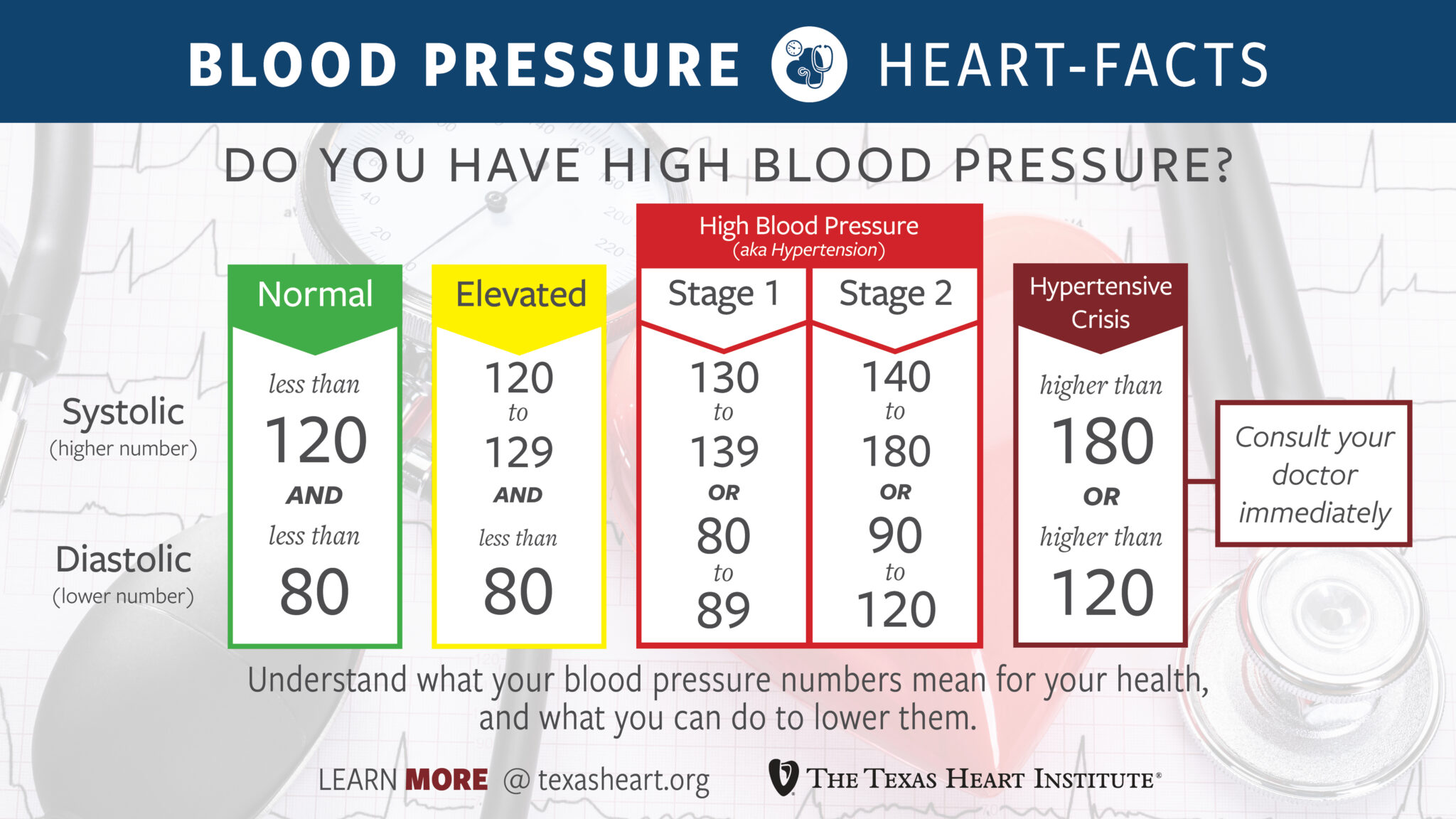
Well, it’s complicated. If you ask the American Heart Association (AHA), they’ll tell you that you’ve officially crossed the line into Hypertension Stage 2. That sounds scary. Honestly, it sounds like a diagnosis you’d want to avoid at all costs. But here’s the kicker: the top number (systolic) and the bottom number (diastolic) are telling two very different stories in this specific reading.
The Great Divide: Why 140/70 is "Isolated Systolic Hypertension"
Most people think of blood pressure as a single unit, like a score on a test. It’s not.
The top number, 140, represents the pressure in your arteries when your heart beats. The bottom number, 70, is the pressure when your heart rests between beats. When the top is high but the bottom is perfectly normal—which 70 absolutely is—doctors call this Isolated Systolic Hypertension (ISH).
It’s actually the most common form of high blood pressure in adults over the age of 65.
Why does this happen? Think of your arteries like garden hoses. When you’re young, they’re stretchy and rubbery. As we age, they can get stiff. When the heart pumps blood into a stiff pipe, the pressure spikes (that's your 140). But because the "hose" isn't clogged or constantly constricted, the pressure drops back down to a healthy level when the heart rests (that's your 70).
🔗 Read more: Silicone Tape for Skin: Why It Actually Works for Scars (and When It Doesn't)
What the Guidelines Say vs. Real Life
In 2017, the goalposts moved. For decades, "high" started at 140/90. Then, the AHA and the American College of Cardiology dropped the hammer, declaring that anything over 130/80 is Stage 1 Hypertension.
Under these rules, 140/70 high blood pressure is definitely in the "we need to talk about this" category.
However, many European medical societies and some American physicians still look at 140/70 with a bit more nuance. They might see it as "borderline." If you’re 25 and hitting 140/70, your doctor is going to be much more concerned than if you’re 75. In older patients, trying to force that 140 down to 120 can sometimes drive the 70 down to 50, making the person feel dizzy, faint, or just plain miserable.
The Danger of the "Gap"
There is a term you should know: Pulse Pressure.
This is just the math between the two numbers. $140 - 70 = 70$.
A "normal" pulse pressure is usually around 40 or 50. When the gap widens—like it does with 140/70—it can be an indicator of arterial stiffness or even underlying issues like a leaky heart valve (aortic regurgitation) or an overactive thyroid.
💡 You might also like: Orgain Organic Plant Based Protein: What Most People Get Wrong
Research published in journals like The Lancet has suggested that a wide pulse pressure can actually be a better predictor of heart issues than the top number alone. It means your heart is working harder to push blood through a system that isn't as flexible as it used to be.
Does One Reading Even Count?
Don't panic over one 140/70 reading.
"White Coat Hypertension" is a very real thing. You’re stressed about traffic, you’re worried about the doctor’s bill, or maybe you just had a double espresso twenty minutes ago. All of these can kick your systolic pressure up by 10 or 20 points while your diastolic stays chill.
To really know if 140/70 high blood pressure is your "new normal," you need a log.
- Buy a validated home cuff (Omron is usually the gold standard).
- Sit quietly for five minutes before checking. No talking. No scrolling TikTok.
- Keep your feet flat on the floor.
- Take readings at the same time every day for a week.
If your average is 140/70, then it’s a trend. If it was just that one time at the clinic, you might just be reacting to the environment.
The Lifestyle Lever: Can You Fix This Without Meds?
The short answer is maybe.
📖 Related: National Breast Cancer Awareness Month and the Dates That Actually Matter
If you're hovering at 140/70, you're in the prime zone for lifestyle interventions. You aren't in a "hypertensive crisis" (which is usually 180/120), so you have time to experiment.
- Sodium is the silent killer. Most of us eat way more than the 1,500mg recommended for heart health. It's not the salt shaker on the table; it's the bread, the deli meat, and the "healthy" frozen dinners.
- Potassium is the secret weapon. Potassium helps your kidneys flush out sodium. Bananas are famous for it, but potatoes, spinach, and white beans actually have more.
- The 30-minute walk. You don't need to run a marathon. Brisk walking for 30 minutes most days can drop your systolic pressure by 5 to 8 points. That's the difference between 140/70 and a much healthier 132/70.
- Magnesium. Many people with stiff arteries are low in magnesium. It helps the smooth muscles in your blood vessels relax.
When to Bring in the Professionals
You shouldn't self-treat 140/70 if you have other "risk multipliers."
If you have diabetes, chronic kidney disease, or a history of smoking, 140/70 is treated much more aggressively. In these cases, your doctor isn't just looking at the number; they're looking at your total cardiovascular risk profile. They might prescribe a low-dose ACE inhibitor or a calcium channel blocker to protect your organs from that constant 140-point pounding.
Actionable Steps for 140/70
If you just saw 140/70 on a screen, here is your immediate game plan:
- Confirm the data. Don't trust a single reading. Use a home monitor for seven days, twice a day (morning and evening).
- Check your "Pulse Pressure." If your gap is consistently wider than 60 points (like 150/70), mention specifically to your doctor that you're concerned about arterial stiffness.
- Audit your minerals. Look at your salt intake for three days. Be honest. Most people find they are consuming 3,000mg or more.
- Ask for a "Basics" blood panel. Make sure your 140/70 isn't being caused by something else, like low potassium or a thyroid issue.
- Focus on the 140. Since your 70 is great, your goal is "systolic management." This usually responds best to aerobic exercise and sodium reduction.
Ultimately, 140/70 is a warning light on the dashboard. It’s not an engine failure, but it’s the car's way of telling you that the system is under more strain than it should be. Address it now, and you likely won't have to deal with the 160s or 170s down the road.