You just sat down in that crinkly paper-covered chair, the cuff tightened around your arm until it pulsed, and the screen flashed 130/75. Now what? Your doctor might mention "Stage 1 Hypertension," but honestly, that sounds way scarier than it usually is for most people.
It’s a weird middle ground.
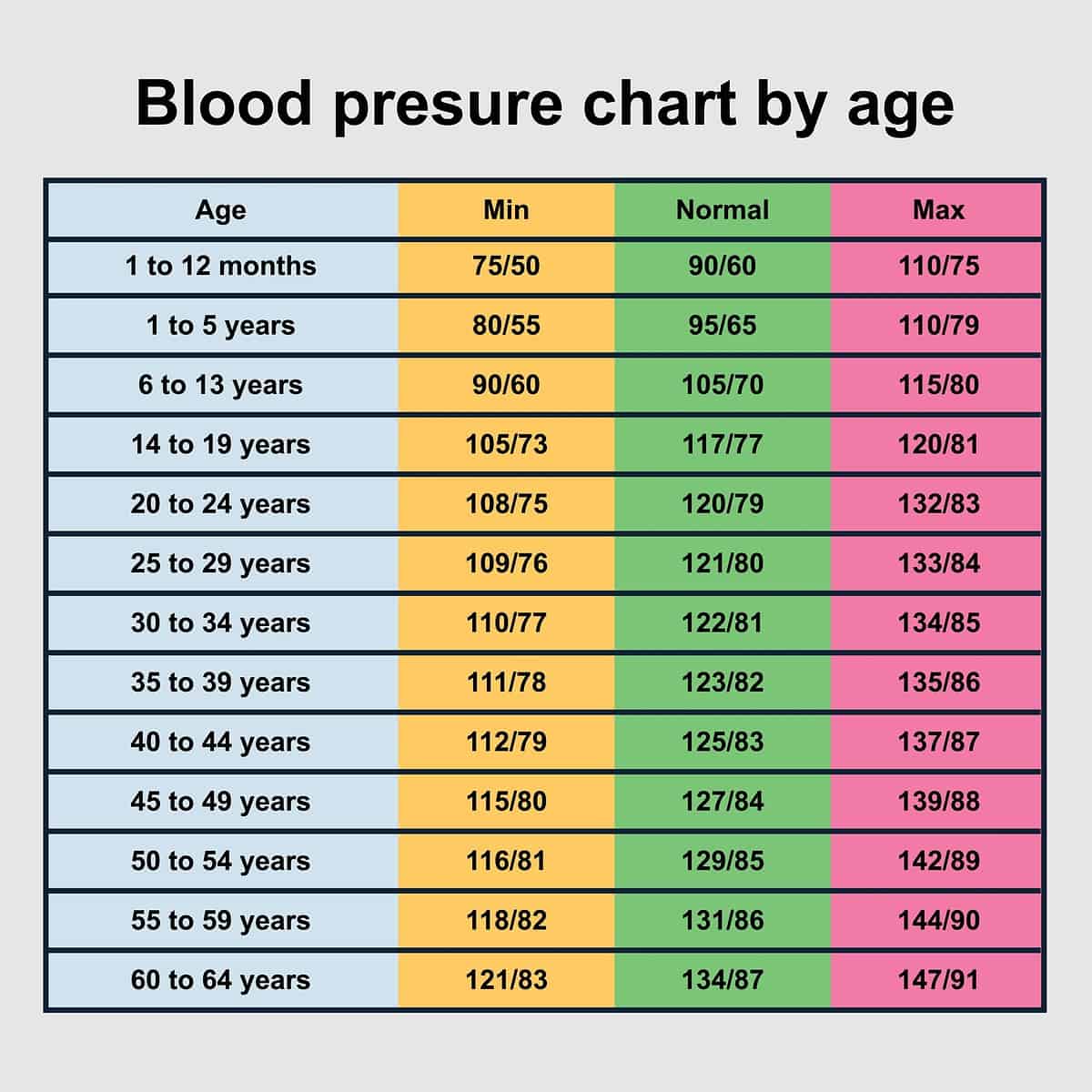
For decades, we were told that 140/90 was the "danger zone," but then the American Heart Association (AHA) and the American College of Cardiology shifted the goalposts back in 2017. Suddenly, millions of people woke up with a diagnosis they didn't have the night before. Having 130 over 75 blood pressure means you’re technically in the high category, even if you feel completely fine. But here’s the thing: that 75—the diastolic number—is actually pretty great. It’s the 130 that’s drawing the side-eye from the medical community.
Decoding 130 over 75 blood pressure: The gap between the numbers
To understand why this specific reading matters, you have to look at what those two numbers are actually doing. The top number, 130, is your systolic pressure. It measures the force your heart exerts on your artery walls every time it beats. Think of it like the water pressure in your home pipes when the faucet is wide open. At 130, the pressure is starting to push the limits of what’s considered "normal." It's like a warning light on your dashboard that isn't red yet, but it’s definitely glowing yellow.
Then there’s the 75.
This is your diastolic pressure, the force when your heart rests between beats. A 75 is squarely in the healthy range (which is typically anything under 80). So, when you have 130 over 75 blood pressure, you have what some might call "isolated systolic hypertension," or at least the very early stages of it. Your heart is pushing a bit hard, but your arteries are relaxing just fine in between. It’s a lopsided story.
Why does this happen? Usually, it's about the stiffness of the arteries. As we age, or if we eat a bit too much salt, or if stress is a constant companion, the large arteries lose some of their "stretch." When the heart pumps blood into these stiffer tubes, the pressure spikes higher (that’s your 130). But because the smaller vessels are still doing okay, the resting pressure stays low (that’s your 75).
Does this reading mean you're in danger?
Not necessarily today. But maybe down the road.
The reason doctors get worked up about 130/75 is because of the cumulative effect. It’s like a slow-motion wear and tear. Over years, that slightly higher pressure can irritate the lining of your blood vessels. This irritation leads to plaque buildup. We call that atherosclerosis. If you ignore a 130 systolic for ten years, you're much more likely to see it creep up to 140, 150, or higher.
💡 You might also like: What's a Good Resting Heart Rate? The Numbers Most People Get Wrong
The SPRINT trial (Systolic Blood Pressure Intervention Trial) is the big study everyone points to. It showed that for certain high-risk adults, bringing that top number down below 120 significantly reduced the risk of heart attacks and strokes. However—and this is a big however—not everyone in that study is you. If you’re 35, active, and have no other health issues, a 130/75 might just be a sign to cut back on the takeout. If you’re 65 with diabetes, it’s a much bigger deal.
Context is everything.
The "White Coat" factor and why one reading is a lie
If you saw 130/75 at the pharmacy kiosk or the doctor’s office, take a breath. It might not even be your real blood pressure.
"White coat hypertension" is incredibly common. You’re rushed, you’re worried about the appointment, you just drank a coffee, or maybe the nurse used a cuff that was too small for your arm. Any of these can bump your systolic number by 10 or 15 points. I've seen patients whose pressure drops significantly just by sitting quietly for five minutes without checking their phones.
To get a real sense of whether 130 over 75 blood pressure is your "true" baseline, you need a trend.
Doctors generally want to see a week's worth of readings taken at home. Take one in the morning and one in the evening. Keep your feet flat on the floor. Don’t talk. If those home readings are consistently 122/72, then your 130/75 at the clinic was just stress. But if you’re seeing 130/75 while sitting on your couch on a Saturday afternoon? Yeah, that’s your real number.
Salt, Potassium, and the hidden levers of pressure
If you want to move that 130 closer to 120, you have to talk about sodium. Most people think they’re "fine" with salt because they don’t use the shaker at the table.
Wrong.
📖 Related: What Really Happened When a Mom Gives Son Viagra: The Real Story and Medical Risks
About 70% of the sodium in the average diet comes from processed foods and restaurant meals. It's in the bread, the pasta sauce, and that "healthy" rotisserie chicken. Sodium holds onto water in your bloodstream. More water equals more volume. More volume equals higher pressure. It’s basic physics.
But here is the secret weapon: Potassium.
Potassium works like an off-switch for sodium. It helps your kidneys flush out the salt and eases the tension in your blood vessel walls. If you’re hovering at 130/75, adding more bananas, spinach, sweet potatoes, and avocados to your plate is often more effective than just "cutting out salt." You’re actively counteracting the pressure rather than just avoiding the trigger.
Lifestyle tweaks that actually move the needle
You don't need to become a marathon runner to fix a 130/75 reading. In fact, most experts, including those from the Harvard Medical School, suggest that "lifestyle modifications" should be the first line of defense at this stage, long before pills enter the conversation.
- The 30-minute rule: You don't need a gym. A brisk walk—where you can still talk but would struggle to sing—for 30 minutes a day can drop your systolic pressure by 5 to 8 points. That’s the difference between "Stage 1" and "Normal."
- The sleep connection: Sleep apnea is a massive, often undiagnosed cause of high blood pressure. If you snore or wake up feeling like a zombie, your 130/75 might be happening because your heart is struggling for oxygen all night.
- Alcohol's double-edged sword: A glass of wine might feel relaxing, but more than one or two drinks starts to constrict blood vessels and raise heart rates. If you're a daily drinker, even a week-long break can show up on the blood pressure monitor.
Is medication necessary? Usually, for 130 over 75 blood pressure, the answer is no—unless you have other "comorbidities." That’s doctor-speak for other problems like chronic kidney disease, a previous heart attack, or a high "ASCVD risk score" (a calculation of your 10-year risk of a heart event). If your risk is low, most physicians will give you three to six months to change your diet and exercise habits before even mentioning a prescription.
Understanding the "Pulse Pressure" nuance
There is a technical term called "Pulse Pressure," which is just the difference between your top and bottom numbers. In this case, 130 minus 75 equals 55.
A "normal" pulse pressure is around 40. When that gap starts to widen (getting closer to 60 or higher), it suggests that your arteries are becoming less elastic. While a 55 isn't a crisis, it is a nudge. It’s your body telling you that the plumbing is starting to stiffen up.
Interestingly, some people find that their pressure hits 130/75 because of specific triggers like ibuprofen or other NSAIDs. If you’re taking Advil every day for back pain, that could easily be the culprit. These meds tell your kidneys to hold onto fluid, which jacks up the pressure. Switching to acetaminophen (Tylenol) can sometimes "cure" Stage 1 hypertension overnight.
👉 See also: Understanding BD Veritor Covid Test Results: What the Lines Actually Mean
Why you should care about the 75
Let’s give some credit to that 75.
Having a diastolic pressure of 75 is actually a very good sign. It means that when your heart is at rest, the pressure in your system drops to a very safe level. This gives your coronary arteries—the ones that supply the heart muscle itself—plenty of time to fill with blood. High diastolic pressure (over 80 or 90) is often harder on the heart muscle over time than a slightly elevated systolic. So, if you’re going to have an "elevated" reading, 130/75 is a lot "better" than 125/85.
Actionable steps to manage 130/75 starting today
Don't panic, but don't ignore it either. A 130/75 is an opportunity to fix things while they're still easy to fix.
First, buy a reliable home monitor. Look for one that is "clinically validated," usually marked with a Dabl or BIHS seal. Omron is a standard brand, but there are others. Stop relying on the machine at the grocery store; they are notoriously uncalibrated and the cuffs are often beat up.
Second, track your "added" sugars. We talk a lot about salt, but recent studies suggest that highly processed sugars (like high-fructose corn syrup) might be just as bad for blood pressure. Sugar increases insulin, which activates the sympathetic nervous system and raises heart rate and pressure.
Third, check your magnesium. Many of us are deficient. Magnesium helps blood vessels relax (vasodilation). You can get it from pumpkin seeds, almonds, or a supplement (though check with your doctor first if you have kidney issues).
Finally, give it time. Blood pressure doesn't change in a day. If you start exercising and eating better, it can take 4 to 6 weeks to see those numbers consistently drop.
Next Steps for You:
- Monitor for one week: Take your pressure every morning after using the bathroom but before eating. Write it down.
- Calculate your 10-year risk: Search for the "ASCVD Risk Estimator" online. Plug in your numbers. If your risk is under 10%, you have plenty of time to use lifestyle changes.
- The "One Less" Rule: Identify one high-sodium or high-sugar item you consume daily (like soda, deli meat, or canned soup) and swap it for a whole-food alternative.
- Discuss with your doctor: Take your log of home readings to your next physical. This data is ten times more valuable to them than the single reading they take in the office.