You just sat down in that crinkly paper-covered chair at the doctor's office. The cuff squeezes your arm tight, your heart thumps a little harder because—honestly—who doesn't get a bit of "white coat" anxiety? Then the nurse says it: "You're at 126 over 80."
It sounds okay, right? It’s not 140. It’s not 150. But it’s also not that "perfect" 120/80 we all grew up hearing about.
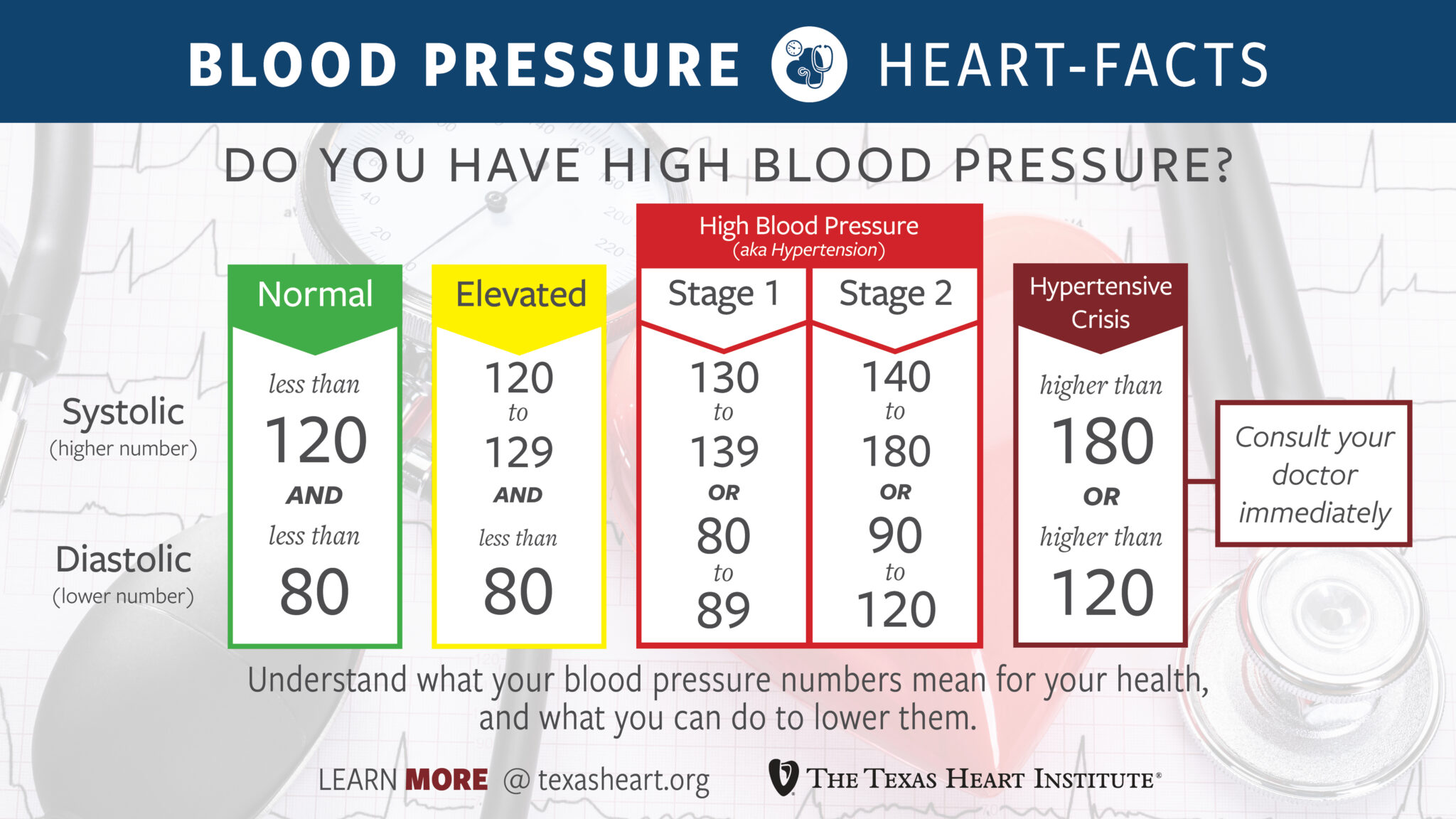
Here is the reality. Having 126 over 80 blood pressure puts you in a category that the American Heart Association (AHA) and the American College of Cardiology (ACC) now call "Elevated." It is a weird, middle-ground space. You aren't "sick," but your body is definitely trying to tell you something. It’s like the yellow light at a traffic intersection; you could probably make it through, but it might be time to start tapping the brakes.
Decoding the numbers: What is actually happening in your veins?
Blood pressure is basically just a measurement of how much force your blood is pushing against the walls of your arteries. Think of it like a garden hose. If the pressure is too high, the hose gets strained. Over years, that strain creates tiny tears in the lining of your vessels.
When we talk about 126 over 80 blood pressure, we are looking at two distinct stories. The top number, 126, is your systolic pressure. That is the force when your heart beats. The bottom number, 80, is the diastolic pressure. That is the pressure when your heart rests between beats.
Now, here is where it gets slightly confusing for people. Under the old rules from a decade ago, you were "normal" until you hit 140/90. But then a massive study called the SPRINT trial changed everything. Researchers found that people who kept their systolic pressure below 120 had significantly lower rates of heart attacks and strokes compared to those aiming for 140.
Because of that, the goalposts moved.
If your top number is between 120 and 129, and your bottom number is less than 80, you are "Elevated." But wait—your bottom number is exactly 80. That technically bumps you into "Stage 1 Hypertension" territory according to current AHA guidelines.
Is that a reason to panic? No. Is it a reason to pay attention? Absolutely.
✨ Don't miss: The Truth Behind RFK Autism Destroys Families Claims and the Science of Neurodiversity
Why 126 over 80 blood pressure is a "sneaky" measurement
The 80 is the kicker here.
In the 2017 clinical practice guidelines, the threshold for Stage 1 Hypertension was lowered to 130/80. This means if either number is at or above that mark, you've crossed the line. Even though 126 is "Elevated," that 80 on the bottom puts you squarely in the first stage of high blood pressure.
It feels nitpicky. I get it. We are talking about a few points.
However, doctors like Dr. Paul Whelton, who chaired the 2017 guideline committee, argue that identifying these numbers early prevents the "cumulative damage" that leads to kidney failure or a late-night trip to the ER ten years from now. Blood pressure is famously a "silent killer" because you usually can't feel 126/80. You don't get a headache. You don't feel dizzy. You just feel... normal.
Meanwhile, your arteries are starting to stiffen. This process is called atherosclerosis. High pressure causes the smooth inner lining of the artery to roughen, which makes it easier for plaque (cholesterol) to get stuck there.
Context is everything
One single reading of 126 over 80 blood pressure does not mean you have a chronic condition.
Your blood pressure is as moody as a teenager. It changes when you talk. It changes when you hold your breath. It definitely changes if you just drank a double espresso or if you're annoyed at the guy who took your parking spot.
To get a real diagnosis, you need a trend. Most doctors want to see a week's worth of readings taken at home, ideally in the morning and evening. You have to sit still for five minutes first. No scrolling on your phone. No talking. Feet flat on the floor. If your average over seven days is still sitting at 126/80, then it's a pattern.
🔗 Read more: Medicine Ball Set With Rack: What Your Home Gym Is Actually Missing
Factors that might be nudging your numbers up:
- The Salt Trap: Most of us eat way more sodium than we realize—not from the salt shaker, but from bread, deli meats, and canned soups.
- Sleep Apnea: If you snore or wake up tired, your nighttime oxygen drops might be spiking your daytime pressure.
- Potassium Deficiency: Most people focus on cutting salt, but they forget to add potassium (found in beans, spinach, and potatoes), which helps the body flush out sodium.
- Stress: Chronic cortisol elevation is a direct line to higher diastolic numbers.
Does 126/80 require medication?
Probably not.
For the vast majority of people with 126 over 80 blood pressure, the first line of defense is lifestyle modification, not a pill bottle. Unless you have other major risk factors like diabetes or existing kidney disease, a doctor is going to tell you to change your habits for three to six months before even mentioning a prescription.
This is actually good news. It means you have agency. You have control.
But "lifestyle change" is a vague, annoying term. Let’s get specific.
The DASH diet (Dietary Approaches to Stop Hypertension) is the gold standard here. It’s not a "diet" in the weight-loss sense, though you might lose weight. It’s a focus on magnesium, calcium, and potassium. In some studies, the DASH diet lowered systolic pressure by up to 11 points. That would take you from 126/80 down to 115/80—safely back in the green zone.
The exercise paradox
You might think that because your blood pressure is "Stage 1," you should take it easy.
Actually, the opposite is true.
When you exercise, your blood pressure spikes temporarily. That’s normal. That’s good. It’s like a workout for your blood vessels. Over time, regular cardio makes your heart stronger. A stronger heart can pump more blood with less effort. If your heart works less to pump, the force on your arteries decreases, and your blood pressure drops.
💡 You might also like: Trump Says Don't Take Tylenol: Why This Medical Advice Is Stirring Controversy
You don't need to run a marathon. Brisk walking for 30 minutes, five days a week, is often enough to see a 5-to-8 point drop in that top number.
Actionable steps to manage 126 over 80 blood pressure
If you just saw this number on a monitor, don't spiral. Start here:
1. Validate the reading.
Buy a validated home blood pressure cuff (look for the "Validated Device" seal). Take your pressure at the same time every morning for a week. Keep a log. If the numbers stay in the 126/80 range, take that log to your doctor.
2. The 2,300mg Rule.
Check your nutrition labels. Most "healthy" frozen meals have 800mg of sodium. If you can keep your total daily intake under 2,300mg—or even better, 1,500mg—you will likely see a shift in your numbers within 14 days.
3. Watch the "Hidden" Spikers.
Decongestants (like Sudafed), NSAIDs (like Ibuprofen), and even some herbal supplements can raise blood pressure. If you're taking these daily for aches or allergies, they might be the reason you're hitting 126/80.
4. Breathwork.
It sounds "woo-woo," but it is science. Deep, slow breathing (6 breaths per minute) for just 5 minutes a day can stimulate the vagus nerve and lower your heart rate and blood pressure almost instantly. It’s a temporary fix that, when done daily, helps reset your nervous system.
5. Alcohol and Caffeine.
If you're a heavy coffee drinker or enjoy a couple of glasses of wine every night, try cutting back for two weeks. Alcohol, in particular, is a major contributor to elevated diastolic (bottom number) pressure.
The bottom line? 126 over 80 blood pressure is a wake-up call, not an emergency. It is the body's way of saying the current status quo isn't working perfectly. By making small, tectonic shifts in how you eat and move now, you avoid the much harder conversations about chronic disease later. Listen to the yellow light. It’s there for a reason.