You’ve probably seen it on every medical poster since you were a kid. 120/80. It’s the "golden number," right? For decades, we were told that if the monitor flashed those digits, you were basically the picture of cardiovascular health. You’d get a pat on the back from the nurse, a sticker if you were lucky, and you’d go about your day. But things have changed. If you’re asking if 120/80 blood pressure good for your specific body, the answer is a bit more nuanced than a simple "yes." Honestly, the medical community has shifted the goalposts recently, and it’s left a lot of people feeling unnecessarily anxious or, worse, overconfident.
The 120/80 Myth and the New "Normal"
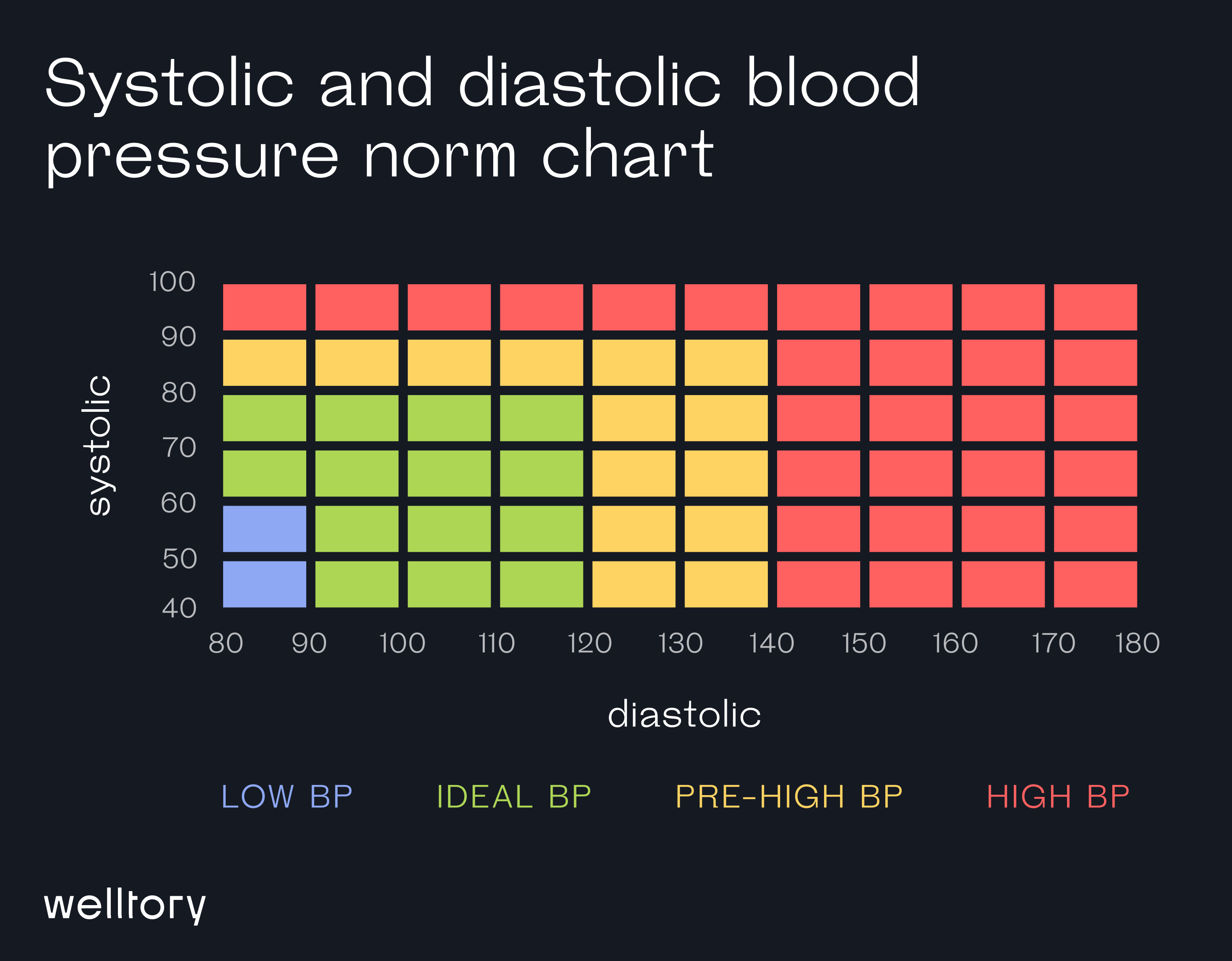
Here’s the deal. In 2017, the American Heart Association (AHA) and the American College of Cardiology (ACC) dropped a bit of a bombshell. They changed the definitions. Suddenly, that 120/80 reading—the one we all thought was perfect—wasn't "normal" anymore. It was reclassified as Elevated.
Wait. Seriously?
Yes. To be considered "Normal" now, your systolic (the top number) has to be less than 120, and your diastolic (the bottom number) has to be less than 80. So, if you’re sitting exactly at 120/80, you’re technically on the cusp. You’re in the yellow light zone. It’s not a crisis. You aren't going to keel over tomorrow. But it’s a signal that your arteries are starting to feel the pressure. It’s a bit like a check-engine light that flickers on. You can keep driving, but you probably want to figure out why it's blinking.
Why the change happened
Doctors didn't just decide to make everyone's lives harder for fun. The shift came after a massive study called the SPRINT trial (Systolic Blood Pressure Intervention Trial). This study looked at over 9,000 adults and found that when people aimed for a lower systolic target—closer to 120 rather than the old 140—the risk of heart attack, heart failure, and stroke dropped significantly. Like, 25% lower risk. That’s huge.
So, while 120/80 is "fine" in the grand scheme of things compared to someone rocking a 160/100, it’s no longer the gold standard. We want to be lower.
Understanding the Two Numbers (Without the Medical Jargon)
Think of your circulatory system as the plumbing in your house.
The top number, Systolic, is the pressure in your pipes when the pump (your heart) is actually pushing water through.
The bottom number, Diastolic, is the pressure in the pipes when the pump is resting between beats.
🔗 Read more: Can You Take Xanax With Alcohol? Why This Mix Is More Dangerous Than You Think
If your systolic is 120, your heart is working at a certain intensity to move blood. If it creeps up to 130 or 140, it’s like cranking the pressure in your home's pipes to the point where the joints start to leak. Eventually, things break. The problem is that your "pipes" are your arteries, and when they "leak" or "burst," it’s a stroke or an aneurysm.
Is 120/80 Blood Pressure Good for Everyone?
Age matters. A lot.
If you’re 22 and your blood pressure is 120/80, your doctor might tell you to cut back on the ramen noodles and start jogging. At that age, your arteries should be elastic and clear; hitting the "elevated" mark early can be a predictor of issues down the road.
However, if you’re 85? 120/80 might actually be too low for some people.
Older adults often deal with "stiff" arteries. If you force the blood pressure too low in an elderly person, they might get dizzy when they stand up—a condition called orthostatic hypotension. They fall. They break a hip. In that specific scenario, a doctor might be perfectly happy with a 130/80 or even slightly higher, because the risk of a fall is more immediate than the long-term risk of a slightly elevated pressure.
It’s all about context. You can’t look at the numbers in a vacuum.
The "White Coat" Factor
Have you ever noticed your heart racing the moment you walk into a doctor’s office? The smell of antiseptic, the cold stethoscope... it’s stressful. This is "White Coat Hypertension." Your blood pressure might spike to 140/90 in the office, but when you're at home on the couch watching Netflix, it’s a perfect 115/75.
This is why a single reading of 120/80 doesn’t tell the whole story. To really know if 120/80 blood pressure good for you, you need a trend. Doctors are moving toward "ambulatory blood pressure monitoring" or asking patients to keep a log at home.
💡 You might also like: Can You Drink Green Tea Empty Stomach: What Your Gut Actually Thinks
Basically, don't freak out over one high reading at the pharmacy kiosk after you just finished a double espresso. It doesn't count.
What Actually Causes That Number to Creep Up?
It's usually not one thing. It's a "death by a thousand cuts" situation.
- Sodium. We all know it. Salt holds onto water. More water in your blood means more volume. More volume means more pressure.
- Potassium deficiency. This is the one people forget. Potassium helps your body flush out sodium and eases the tension in your blood vessel walls. If you aren't eating bananas, spinach, or potatoes, your blood pressure is likely higher than it needs to be.
- Sleep Apnea. If you snore or stop breathing at night, your brain panics. It releases stress hormones. Your blood pressure stays high all night when it should be dropping.
- The "Invisible" Stress. It’s not just work stress. It’s systemic inflammation. It’s lack of movement. It’s that second glass of wine.
Real-World Action: Moving from 120/80 to "Optimal"
If you’re staring at a 120/80 reading and want to get it down into the "Normal" range (under 120/80), you don't necessarily need meds. Most doctors won't even prescribe medication for "Elevated" blood pressure unless you have other major risk factors like diabetes or kidney disease.
Instead, they'll tell you to change your life. Which sounds exhausting, but it's actually pretty simple if you focus on the big wins.
The DASH Diet works (mostly)
The Dietary Approaches to Stop Hypertension (DASH) isn't a fad. It’s a clinically proven way to eat. It emphasizes fruits, veggies, and lean protein while nuking processed sugars and heavy salt. But honestly? Just eating more fiber and cutting out ultra-processed snacks does 80% of the work.
Movement is non-negotiable
You don't have to run a marathon. Just walk. Briskly. 30 minutes a day. It strengthens the heart muscle, making it a more efficient pump. An efficient pump doesn't have to work as hard, which lowers the pressure on the pipes.
📖 Related: Bragg Organic Raw Apple Cider Vinegar: Why That Cloudy Stuff in the Bottle Actually Matters
Magnesium: The unsung hero
Many people are chronically low on magnesium. This mineral helps muscles relax. Since your blood vessels are lined with smooth muscle, magnesium helps them "chill out." Taking a supplement (with a doctor's okay) or eating pumpkin seeds can sometimes nudge that 120 down to 115.
The Risks of Ignoring the "Elevated" Label
The danger of 120/80 is that you feel fine. High blood pressure is the "Silent Killer" for a reason. You don't feel the micro-tears in your arteries. You don't feel your kidneys slowly scarring from the constant pressure.
By the time you feel high blood pressure—headaches, blurred vision, chest pain—you’re usually in a hypertensive crisis. That’s why catching it at 120/80 is actually a gift. It’s your body giving you a head start.
When to Actually Worry
If that 120/80 starts climbing toward 130/80, you’ve officially entered Stage 1 Hypertension. This is where the conversation with your doctor gets more serious. If it hits 140/90, that’s Stage 2.
But here is a nuanced point: focus on the systolic (top number) more as you get older. For people over 50, the top number is a much better predictor of heart disease than the bottom number. If your reading is 135/75, don't be fooled by the "75" being good. That "135" is the one doing the damage.
Practical Next Steps for Your Health
Don't just take one reading and call it a day. If you want to take control of your cardiovascular health, follow this specific protocol for the next two weeks to see where you actually stand.
- Buy a validated home monitor. Look for one that goes on your upper arm, not the wrist. Wrist monitors are notoriously finicky and inaccurate if your arm isn't at the exact right level. Brands like Omron or Withings are usually solid bets.
- Measure correctly. Sit in a chair with your back supported. Keep your feet flat on the floor—no crossing your legs. Don't talk. Don't check your phone. Sit there for five minutes before you press the button.
- Log the data. Take two readings in the morning and two in the evening. Do this for a week.
- Look at the average. Ignore the highest and lowest numbers. The average of those middle readings is your "true" blood pressure.
- Audit your "hidden" salt. Check the labels on your bread, salad dressings, and canned soups. You’d be shocked how much sodium is in things that don't even taste salty.
- Increase your "Nitric Oxide" foods. Beets, arugula, and garlic help your body produce nitric oxide, which dilates blood vessels. It’s like widening the lanes on a highway to reduce traffic jams.
Ultimately, 120/80 is a wake-up call, not a death sentence. It’s the point where you decide if you’re going to let your health drift or if you’re going to steer the ship back toward the "Normal" zone. A few small tweaks to your salt intake and a daily walk are usually all it takes to push those numbers back into the safe territory. Take the data for what it is—a tool for longevity, not a reason for stress.