You’ve probably seen it on every medical poster since the 1990s. That magic number. 120 over 80. It’s the gold standard, right? If you hit that bullseye, you’re basically Wolverine. But honestly, the reality of whether 120 80 blood pressure good is actually the "perfect" score has changed quite a bit in the last few years.
Medical guidelines aren't static. They breathe. They evolve as we get more data from massive longitudinal studies like the Framingham Heart Study or the SPRINT trial. If you walked into a clinic in 2010 with a reading of 135/85, your doctor might have given you a pat on the back and sent you home. Today? They’d likely be talking to you about "Stage 1 Hypertension" and lifestyle interventions. The goalposts moved.
Why we stopped calling 120/80 "normal"
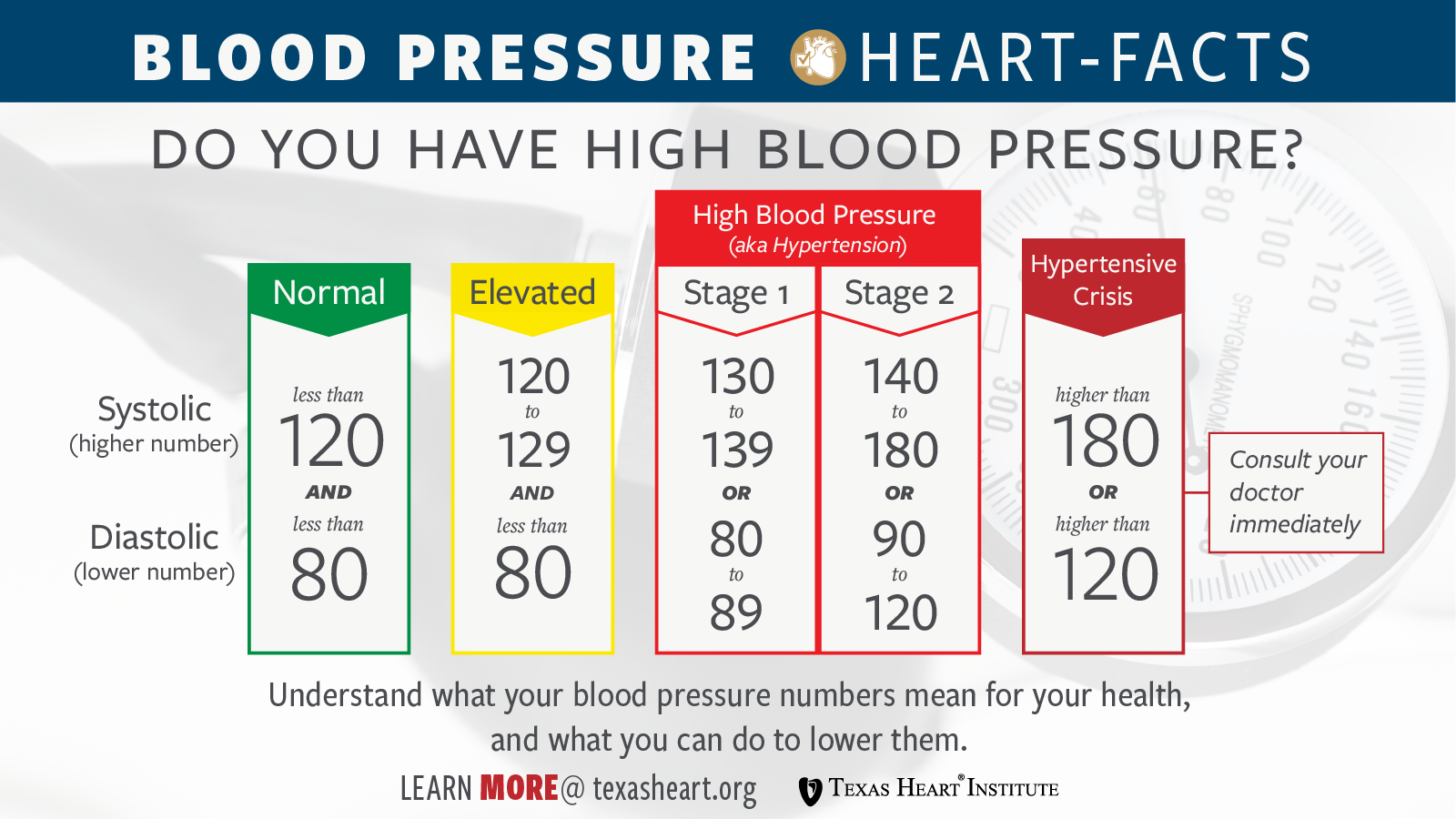
For a long time, the American Heart Association (AHA) and the American College of Cardiology (ACC) labeled 120/80 as the ceiling of normal. It was the safe zone. But then, in 2017, everything shifted. The guidelines were updated, and suddenly, 120/80 became the threshold for what is now called "Elevated" blood pressure.
It feels a bit like a bait-and-switch.
If your top number (systolic) is exactly 120, you’re technically in the elevated category. To be "Normal," you actually need to be under 120 and under 80. Think 118/78. It sounds like a tiny distinction, a rounding error basically, but for your arteries, those few points of pressure matter over the span of decades.
The Systolic vs. Diastolic dance
Blood pressure is just a measure of force. The systolic (top) number is the pressure when your heart beats. The diastolic (bottom) is the pressure when it rests. Most doctors, including experts like Dr. Paul Whelton who chaired the 2017 Guideline Task Force, place more weight on the systolic number as we age. Why? Because it’s a better predictor of cardiovascular "events"—the polite medical term for strokes and heart attacks.
Stiff arteries. That’s the culprit. As we get older, our pipes get less flexible. When the heart pumps, those stiff pipes don't expand, so the pressure spikes.
Is 120 80 blood pressure good for everyone?
The short answer is: maybe.
Context is everything in medicine. If you are a 22-year-old athlete and your pressure is 120/80, your doctor might wonder why it isn't a bit lower, maybe 110/70. If you’re an 85-year-old grandmother, 120/80 is actually fantastic—it's arguably better than the "aggressive" targets some doctors used to push.
🔗 Read more: That Time a Doctor With Measles Treating Kids Sparked a Massive Health Crisis
There's this concept called "J-Curve" risk. It suggests that if you push blood pressure too low in elderly patients, you actually increase the risk of falls, fainting, and kidney issues. So, while 120 80 blood pressure good is the general vibe, your specific health history—like if you have diabetes or chronic kidney disease—changes the math.
The "White Coat" variable
We have to talk about the stress of the doctor's office. You’re sitting on that crinkly paper, it’s cold, you’re worried about your insurance, and a nurse wraps a Velcro cuff around your arm. Your pressure jumps. This is "White Coat Hypertension."
Research published in The Lancet has shown that home monitoring is often way more accurate than office readings. If you get 120/80 at the doctor, you might actually be 112/74 at your kitchen table. That’s why one single reading is basically useless. Doctors need a trend. They need a week of data.
The SPRINT Trial changed the game
If you want to know why the medical community got so aggressive about these numbers, look at the Systolic Blood Pressure Intervention Trial (SPRINT). It was a massive study funded by the National Institutes of Health.
They took over 9,000 people and split them into two groups.
Group A: Target under 140.
Group B: Target under 120.
The results were so dramatic they actually stopped the study early. The group with the 120 target had significantly lower rates of heart failure and death. This is the "smoking gun" that led the AHA to tighten the screws on what we consider "good." It turned out that aiming for 120 80 blood pressure good wasn't just a suggestion; it was a lifesaver.
Salt, Potassium, and the hidden chemistry
Most people think about salt. "Don't eat the fries," they say. And yeah, sodium makes you retain water, which increases blood volume and pressure. Simple physics.
But nobody talks about potassium.
💡 You might also like: Dr. Sharon Vila Wright: What You Should Know About the Houston OB-GYN
Potassium is the "anti-salt." It helps your blood vessels relax and helps your kidneys flush out the sodium. If you’re hitting 120/80 but your diet is 90% processed food, you’re likely missing the potassium cushion that protects your vascular walls. Avocados, bananas, spinach—they aren't just "health foods"; they are physiological pressure valves.
What happens if you stay at 125/82?
You won't drop dead tomorrow. Hypertension is the "silent killer" because it takes years, even decades, to do its damage. Think of it like a slow leak in a pipe behind a wall.
At 125/82, your heart has to work slightly harder with every single beat. Over 100,000 beats a day, that adds up. The muscle of the left ventricle starts to thicken (hypertrophy). Thick muscle is less efficient. Eventually, the heart gets tired.
At the same time, that constant high-pressure stream is scarring the delicate lining of your arteries (the endothelium). These scars are where cholesterol gets stuck. That’s how you get plaques. That’s how you get blockages.
Real-world ways to nudge the needle
If you're sitting at 122/81 and want to get back into the "Normal" green zone without medication, you have more power than you think.
- The 2-pound rule: Studies show that for every kilogram (about 2.2 pounds) of weight lost, your systolic blood pressure can drop by about 1 mmHg. It’s a very direct correlation.
- The DASH Diet: This isn't a fad. It stands for Dietary Approaches to Stop Hypertension. It's heavy on fruits, veggies, and low-fat dairy. It has been shown to drop blood pressure as effectively as some medications.
- Sleep Apnea: This is the big one people miss. If you snore or stop breathing at night, your oxygen levels drop, your body panics, and it dumps adrenaline into your system. This spikes your blood pressure while you sleep. If you can't get your numbers down despite eating well and exercising, go get a sleep study. Seriously.
Alcohol and the "Rebound" effect
Sorry to be the bearer of bad news, but that nightly glass of wine might be the reason you're hovering at 128/84. While some studies once suggested moderate drinking was fine, newer genomic analyses (like those published in JAMA Network Open) suggest that any alcohol intake is associated with increased blood pressure risk.
It’s about the "rebound." When the alcohol wears off, your sympathetic nervous system kicks into high gear, raising your heart rate and tightening your vessels.
Why 120/80 is still a "Good" goal
Despite the new "Elevated" label, if you are consistently hitting 120/80, you are doing better than about half of the adult population in the United States. We are in the middle of a hypertension crisis.
📖 Related: Why Meditation for Emotional Numbness is Harder (and Better) Than You Think
Being at 120/80 means you are at the gateway. You’re at the point where lifestyle choices actually matter. Once you cross into 140/90 territory, the "inertia" of the disease makes it much harder to reverse without pills.
Does gender matter?
Absolutely. For years, we treated men and women the same when it came to blood pressure. Big mistake. Research from the Smidt Heart Institute at Cedars-Sinai suggests that women's blood pressure may actually start causing damage at lower thresholds than men's.
A "normal" reading for a woman might actually need to be lower than for a man to provide the same level of protection against heart disease. This is a developing field, but it highlights that 120 80 blood pressure good isn't a one-size-fits-all metric.
Actionable steps for your next check-up
Don't just take the number the nurse gives you and leave.
- Check both arms. There should be a minimal difference. If one arm is significantly higher, it could indicate a blockage in an artery.
- Sit still for 5 minutes before the cuff goes on. No talking. No checking your phone. If they take your pressure the second you sit down, it’s going to be high.
- Keep a log. Buy a validated home monitor (check validatebp.org to make sure it's a good one). Take your pressure at the same time every morning for a week.
- Ask about your "Global Risk." Blood pressure doesn't exist in a vacuum. A doctor should look at your BP alongside your cholesterol, your A1c (blood sugar), and your age to determine your 10-year risk of a heart attack.
The bottom line on 120/80
It’s a great target, but it’s not the finish line.
Think of 120/80 as a yellow light. It’s not a red light (danger), but it’s a sign to slow down and check your surroundings. If you’re there, you’re in a position of strength. You can maintain it through movement, better sleep, and maybe a few less salty snacks.
Health isn't a snapshot; it's a movie. Your blood pressure is just one of the main characters. Keep it in check, stay curious about your numbers, and don't be afraid to ask your doctor for the "why" behind the "what."
The best thing you can do right now? Go for a 15-minute walk. It’s the simplest, cheapest, and most effective way to start pushing that 120 down to a 115. Your arteries will thank you in twenty years.