Living with a gut that feels like it’s constantly throwing a tantrum is exhausting. You know the drill. One day it’s bloating that makes your jeans feel two sizes too small, and the next, you’re scouting out every public restroom in a three-mile radius. Finding irritable bowel medications over counter shouldn't feel like a high-stakes chemistry experiment, but walk into any CVS or Walgreens and you’re met with a wall of brightly colored boxes promising "instant relief" and "total gut health." Honestly, most of it is noise.
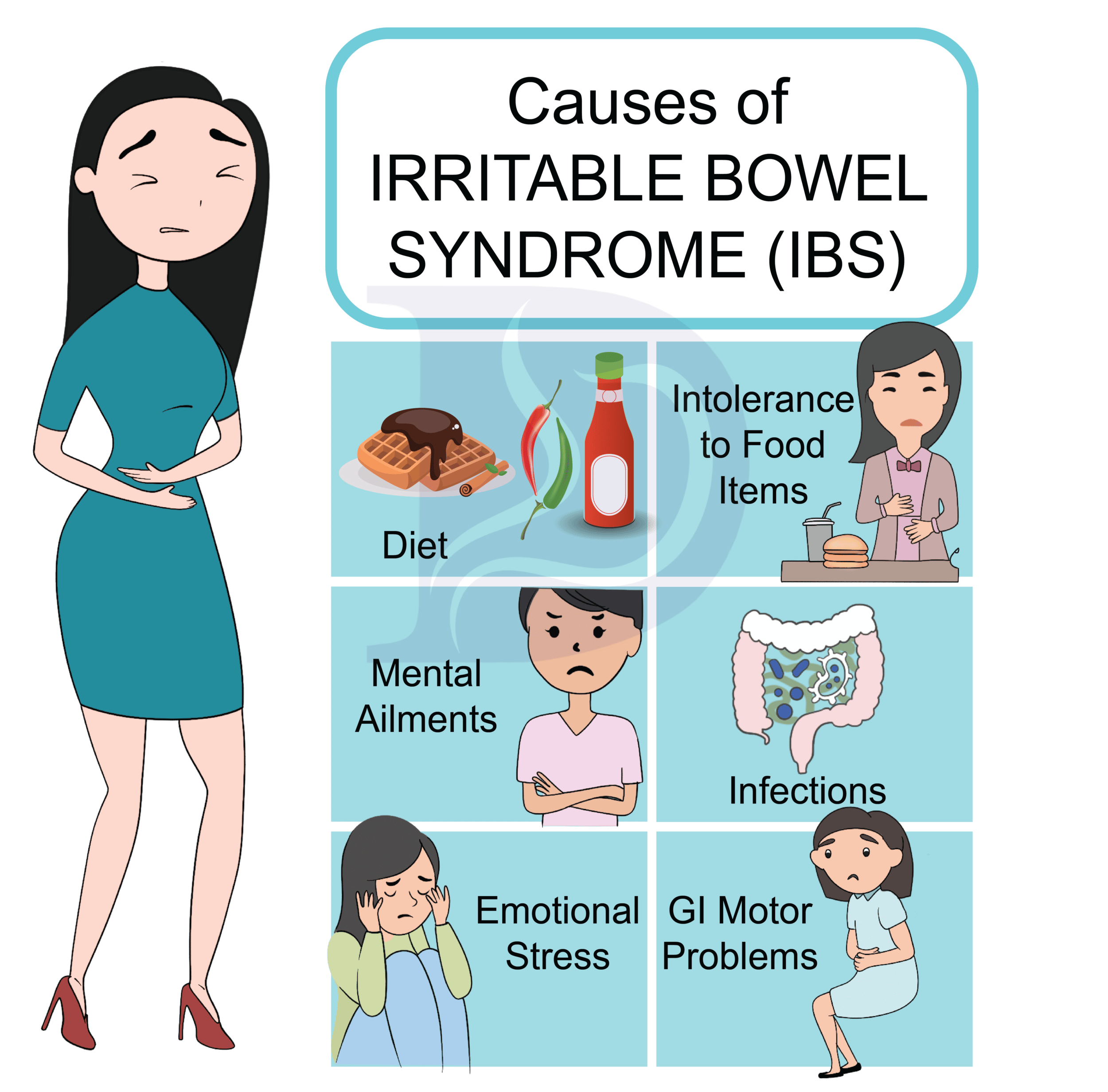
I’ve spent years looking into how people manage functional gastrointestinal disorders. The reality is that Irritable Bowel Syndrome (IBS) isn't a single disease. It’s a collection of symptoms, which means a "one size fits all" pill is basically a myth. Some people need to slow things down. Others need to get things moving. And some just need the cramping to stop so they can sit through a dinner party without breaking into a cold sweat.
The Problem With the Term "IBS Medicine"
When you search for irritable bowel medications over counter, you’re often directed toward general digestive aids. But there is a massive difference between occasional heartburn and the chronic, recurring dysfunction of IBS. The FDA doesn’t actually approve many non-prescription drugs specifically for "IBS." Instead, we use medications designed for specific symptoms—diarrhea, constipation, or gas—to manage the syndrome.
It’s a bit of a patchwork quilt approach. You’re treating the smoke, not necessarily the fire. But when the smoke is keeping you home from work, you don't really care about the semantics; you just want to feel normal again.
Anti-Diarrheals: The "Stop" Button
If your IBS leans toward the "D" variety (diarrhea-predominant), your first instinct is probably to grab Loperamide. Most people know it as Imodium. It works by slowing down the rhythm of your digestion. Think of your gut as a conveyor belt; Loperamide basically turns the speed dial down so your body has more time to absorb water.
But here is where people mess up. If you take too much, you’ll swing wildly in the opposite direction and end up backed up for three days. It’s also not meant to be a daily vitamin. Gastroenterologists like Dr. Mark Pimentel, a leading researcher at Cedars-Sinai, often point out that while Loperamide helps with stool frequency, it does almost nothing for the abdominal pain or bloating that comes with IBS. It stops the bathroom trips, but it doesn't stop the hurt.
The Laxative Minefield
Then there’s the other side of the coin: IBS-C. If you’re dealing with constipation, the "irritable bowel medications over counter" options get overwhelming fast. You have stimulants like Bisacodyl (Dulcolax) and Senna. These are basically a physical kick to your intestines. They work, but they can cause some pretty nasty cramping.
🔗 Read more: Why Having Sex in Bed Naked Might Be the Best Health Hack You Aren't Using
A lot of experts now point toward Polyethylene Glycol 3350, or Miralax. It’s an osmotic laxative. Instead of irritating the nerves in your gut to force a movement, it just draws water into the colon to soften things up. It’s generally considered safer for long-term use because it doesn't cause that "dependency" feeling where your gut forgets how to work on its own. Still, it takes time. You aren't going to see results in twenty minutes. It’s a slow-burn solution.
Peppermint Oil: The Surprise Heavyweight
You might think "essential oils" sound like something your aunt tries to sell you through a Facebook group, but Peppermint Oil is actually one of the most well-researched irritable bowel medications over counter available.
Specifically, you’re looking for enteric-coated capsules. Brand names like IBgard have done a lot of the heavy lifting in clinical trials. The enteric coating is the "secret sauce" here. It ensures the capsule doesn't dissolve in your stomach—which would give you world-class heartburn—and instead opens up in the small intestine. Menthol, the active ingredient, acts as a natural calcium channel blocker. It relaxes the smooth muscle of the gut wall.
A 2019 meta-analysis published in BMC Complementary and Alternative Medicine looked at twelve different trials and found that peppermint oil was significantly superior to placebo for global IBS symptoms. It’s one of the few things you can buy without a script that actually tackles the pain, not just the bathroom habits.
Why Probiotics Are a Gamble
Let’s talk about the giant probiotic-shaped elephant in the room. Everyone tells you to take them. The marketing is relentless. But the truth? Most "gut health" supplements on the shelf at the grocery store are useless for IBS.
The strain matters. You can’t just swallow a random pill with "10 billion CFU" on the label and expect a miracle. Bifidobacterium infantis 35624 (found in Align) has some decent data behind it for reducing bloating and gas. Lactobacillus plantarum 299v is another one that specifically targets abdominal pain. But if you’re just grabbing a generic store brand, you’re probably just making your urine more expensive.
💡 You might also like: Why PMS Food Cravings Are So Intense and What You Can Actually Do About Them
Also, for some people—especially those with Small Intestinal Bacterial Overgrowth (SIBO)—probiotics can actually make things worse. They’re adding more fuel to an already crowded fire. If you try a probiotic and feel like a balloon about to pop after three days, stop. Your body is giving you a very clear signal.
Fiber: The Great Divider
Fiber is tricky. For years, the standard advice for anyone with a "finicky stomach" was to eat more bran. That was actually terrible advice for a lot of IBS sufferers. Insoluble fiber (the stuff in wheat bran and whole grains) is like rubbing sandpaper on an already inflamed gut.
If you’re looking at fiber-based irritable bowel medications over counter, you want Psyllium husk (like Metamucil). This is soluble fiber. It forms a gel. If you’re too loose, it soaks up water. If you’re too tight, it adds bulk and moisture to help things slide along. It’s a regulator.
Start small. Seriously. If you jump from zero fiber to a full dose of Psyllium, you will be miserable. Start with a teaspoon and work your way up over two weeks. Give your microbiome time to adjust to the new workload.
Managing the "Brain-Gut" Connection Without a Script
It sounds "woo-woo," but your brain and your gut are physically connected via the vagus nerve. This is why you get butterflies when you’re nervous. For many with IBS, the "nerves" in the gut are hypersensitive. They’re screaming at a volume of 10 when the actual problem is a 2.
While things like Simethicone (Gas-X) can help physically break up gas bubbles, they don't do anything for the "visceral hypersensitivity"—that feeling of being intensely aware of every gurgle in your abdomen.
📖 Related: 100 percent power of will: Why Most People Fail to Find It
Some people find relief using antihistamines, though this is "off-label" territory. There is emerging research suggesting that mast cells (part of your immune system) play a role in IBS irritation. While things like Benadryl aren't IBS meds, some people find certain antihistamines help calm the systemic "noise." However, you’ve gotta be careful with the drowsiness.
What to Avoid at the Pharmacy
When hunting for irritable bowel medications over counter, watch out for:
- Artificial Sweeteners: Many chewable tablets or "sugar-free" fibers use sorbitol or xylitol. These are FODMAPs. They ferment in your gut and cause massive bloating. You’re literally buying the thing that causes the problem.
- Excessive Stimulants: Avoid any "cleansing" teas. They usually contain high doses of Senna which can lead to "lazy bowel syndrome" if overused.
- Multi-Symptom Cold Meds: If you have IBS, be wary of medicines with high alcohol content or certain dyes that can irritate the gut lining.
When the Pharmacy Aisle Isn't Enough
There is a ceiling to what you can do on your own. If you’re seeing "red flag" symptoms, no amount of over-the-counter stuff is going to fix it. If you’re losing weight without trying, seeing blood, or waking up in the middle of the night because of pain, you need a doctor. Those aren't typical IBS markers; those are signs that something else, like IBD (Crohn’s or Colitis) or even celiac disease, might be the culprit.
Practical Steps for Relief
Don't buy five things at once. If you start a probiotic, a fiber supplement, and peppermint oil on the same day and you feel better, you won't know which one worked. If you feel worse, you won't know what to stop.
- Identify your "Type": Are you mostly C (constipated), D (diarrhea), or M (mixed)?
- Try Peppermint First: If pain and bloating are your main issues, enteric-coated peppermint oil is the most evidence-based starting point.
- The Psyllium Test: Introduce soluble fiber slowly. Use the powder you mix with water rather than the gummies, as the gummies often have sugar alcohols.
- Track the Triggers: Keep a simple note on your phone. What did you take, and what did you eat? Sometimes the "cure" is just avoiding that one specific garlic-heavy pasta sauce.
- Check the Inactive Ingredients: Read the fine print on the back of the bottle. If it has sorbitol, mannitol, or high fructose corn syrup, put it back on the shelf.
Managing IBS is more about strategy than just popping a pill. Over-the-counter options are great tools, but they work best when you understand exactly which "fire" you’re trying to put out. Use them targetedly, keep an eye on how your body reacts, and don't be afraid to change course if a supplement isn't pulling its weight after a couple of weeks.