You’re sitting in the pediatrician’s office, and they wrap that tiny, Velcro cuff around your baby’s arm or leg. It’s a bit of a struggle. The baby is squirming, maybe crying, and you’re wondering if the numbers even matter at this age. Honestly, most parents don't think about blood pressure until they see a nurse charting it. We focus on weight percentiles and head circumference, but an infant blood pressure chart is a different beast entirely. It isn’t like an adult reading where 120/80 is the "golden" number. In the world of neonates and infants, the "normal" range is a moving target that shifts almost daily in the first week of life.
It's complex.
If you look at a standard chart, you'll see percentiles based on age, sex, and height. For a newborn, a systolic reading (the top number) might be as low as 60 or 70. By the time they hit their first birthday, that same number would be cause for a closer look. Blood pressure is essentially the force of blood pushing against artery walls. In babies, those walls are incredibly compliant, and the heart is still figuring out its long-term rhythm.
Why an infant blood pressure chart is so confusing
If you try to Google a "normal" blood pressure for a six-month-old, you’re going to get a headache. Unlike adults, where we have clear cut-offs for hypertension, pediatric standards rely on the Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. This data—which is the gold standard—uses the 90th, 95th, and 99th percentiles.
Basically, a baby’s blood pressure is only "high" if it’s higher than 95% of other babies who are the exact same age, gender, and height.
Height matters more than you’d think. A taller baby naturally requires a slightly higher pressure to move blood through a larger frame. If your doctor uses an infant blood pressure chart that ignores height, they might be missing the full picture. Also, the "cuff size" is the biggest source of error. If the cuff is too small, the reading will be falsely high. If it's too big, it'll look dangerously low. It has to cover about 40% of the arm circumference. I’ve seen many "scary" readings turn out to be nothing more than a nurse using a toddler cuff on a three-month-old.
The first 24 hours are wild
In the NICU or the newborn nursery, everything is compressed. A baby born at 30 weeks gestation has a vastly different "normal" than a full-term baby. For those first few hours, doctors often use the "mean arterial pressure" (MAP) and compare it to the baby’s gestational age in weeks. If a baby is 28 weeks, we want the MAP to be at least 28. It’s a quick-and-dirty rule of thumb that neonatologists like Dr. Joseph Flynn, a leading expert in pediatric hypertension, have discussed in various clinical reviews.
As the baby stabilizes, the numbers climb. By day four, the kidneys are better at regulating fluid, and the heart is pumping more efficiently.
Reading the numbers: Systolic vs. Diastolic in babies
Let’s look at some rough ranges. Don't treat these as gospel because, again, percentiles are king.
📖 Related: How do you make homemade cough syrup without the store-bought chemicals
For a full-term newborn (1-3 days old), you might see:
- Systolic: 65 to 85 mmHg
- Diastolic: 35 to 55 mmHg
By the time they are 3 to 6 months old:
- Systolic: 70 to 90 mmHg
- Diastolic: 45 to 65 mmHg
And by 1 year:
- Systolic: 80 to 100 mmHg
- Diastolic: 55 to 70 mmHg
Notice the gap? It’s huge. A systolic of 85 is perfectly normal for a one-year-old but might be at the very top of the range for a two-day-old. This is why doctors don't usually worry about a single reading unless it's way out of bounds. They look for trends. If a baby is consistently hitting the 99th percentile across three different visits, that’s when the "hypertension" label starts being discussed.
What actually causes high blood pressure in infants?
In adults, high blood pressure is usually about lifestyle—salt, stress, lack of exercise. In infants? It’s almost always "secondary." That means something else is causing it. It’s not because the baby is "stressed."
Most of the time, it’s the kidneys.
Renal artery stenosis or structural issues with the kidneys account for the vast majority of infant hypertension cases. Another big one is Coarctation of the Aorta. This is a narrowing of the large blood vessel that leads from the heart. Doctors often check blood pressure in both the arm and the leg to screen for this. If the arm pressure is way higher than the leg pressure, it’s a massive red flag that the blood is getting "stuck" or restricted as it tries to reach the lower body.
Other culprits include:
- Bronchopulmonary Dysplasia (BPD): Common in preemies who were on ventilators.
- Medications: Some steroids or even caffeine used in the NICU can bump the numbers.
- Umbilical Catheters: If a baby had a line in their belly button after birth, it can sometimes cause tiny clots that affect blood flow to the kidneys later on.
It’s scary to hear your baby has high blood pressure, but usually, it's a symptom of a fixable or manageable underlying condition rather than a lifelong "disease" like adult hypertension.
The "Fussy Baby" Factor
You can't get an accurate reading on a screaming baby. Period.
Kinda obvious, right? Yet, it happens all the time. A baby is hungry, wet, or just hates the cold stethoscope, and suddenly their systolic jumps to 110. The American Academy of Pediatrics (AAP) suggests that a baby should be quiet or asleep for at least five minutes before the measurement is taken. If the nurse takes it while the baby is kicking, the infant blood pressure chart becomes useless.
I’ve seen doctors wait until the baby is literally mid-nap or nursing to sneak the cuff on. That "resting state" is the only way to get a baseline that actually means something. If your baby’s reading was high during a meltdown, ask for a re-check when they’ve calmed down. Honestly, it's often just "white coat syndrome" but for the diaper crowd.
When should you actually worry?
If the blood pressure is truly elevated, you might notice things like:
- Unexplained irritability (more than just regular colic).
- Poor weight gain or "failure to thrive."
- Tachypnea (breathing too fast).
- Frequent nosebleeds (though this is much rarer in infants than older kids).
Most of the time, hypertension in babies is "silent." It's caught during routine screenings, which is why those measurements at the 6-month and 12-month checkups are actually pretty vital, even if they seem like a hassle.
How doctors use the chart to make decisions
When a doctor looks at an infant blood pressure chart, they aren't just looking at one dot. They are looking at the curve. If a baby starts at the 50th percentile and suddenly jumps to the 95th, that’s more concerning than a baby who has always been in the 90th percentile and is otherwise growing perfectly.
Medical professionals use specific software or complex printed tables that factor in:
- Gender: Boys and girls have slightly different vascular development rates.
- Age: Down to the week for newborns and the month for infants.
- Height Percentile: This is the big one. A "short" baby with a reading of 95 might be hypertensive, while a "tall" baby with the same reading is totally fine.
If the numbers are high, the next step isn't usually pills. It’s an ultrasound of the kidneys or an echocardiogram of the heart. They want to see the plumbing. They want to make sure the "pipes" are the right size and that the "pump" isn't working harder than it needs to.
Actionable Steps for Parents
If you are concerned about your baby's blood pressure or if a high reading was mentioned at your last visit, here is what you should actually do.
First, ask for the specific percentile, not just the raw numbers. Knowing your baby is in the "85th percentile" is much more helpful than knowing their systolic was "92." It gives you context.
Second, ensure the cuff size was documented. If the medical record doesn't specify which cuff was used, the reading is arguably invalid for a formal diagnosis. You want to see "Size 1" or "Infant Cuff" noted in the chart.
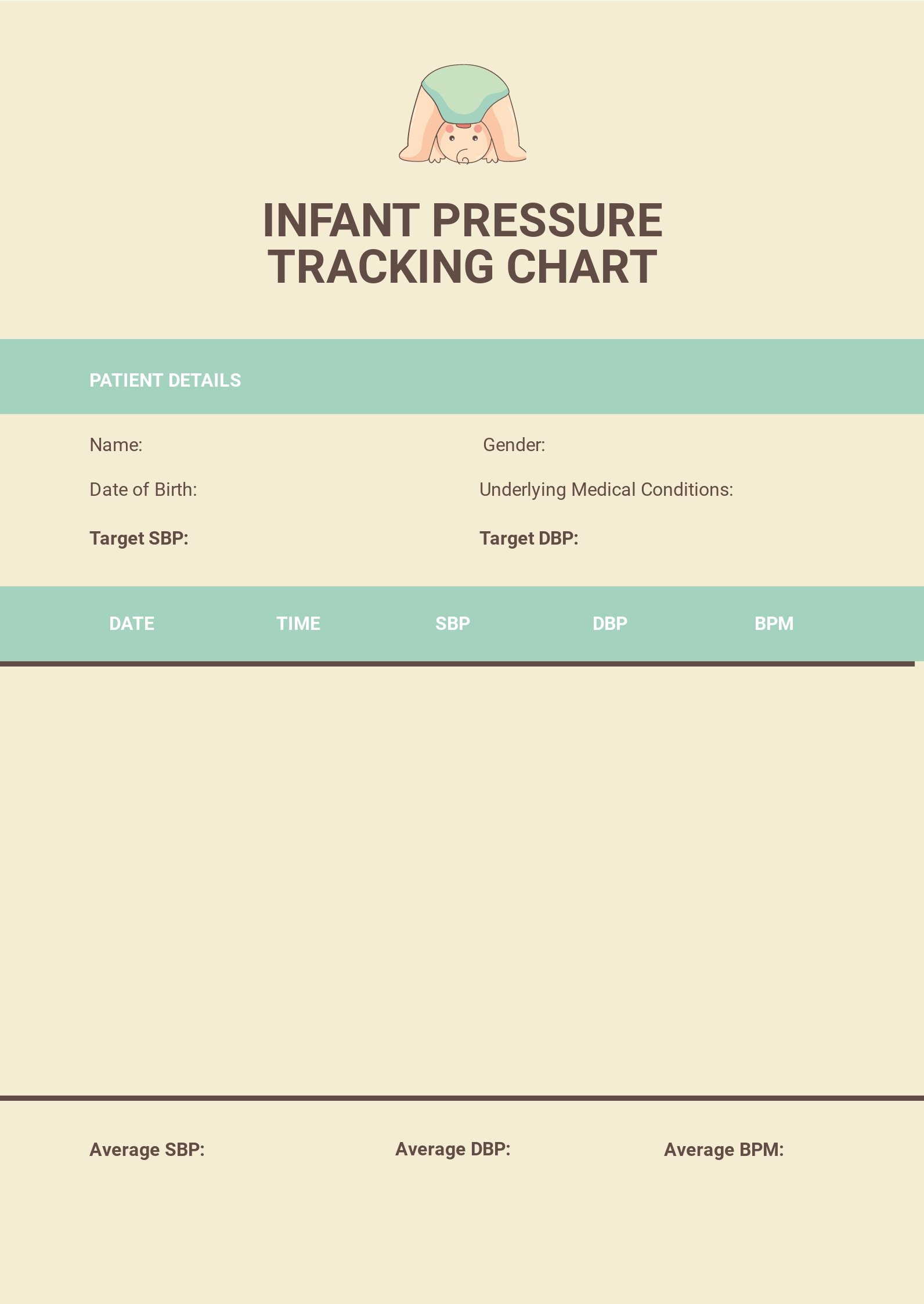
Third, keep a log if you are asked to do home monitoring. Use a high-quality pediatric-specific monitor; don't just use an adult one and hope for the best. Take the readings at the same time every day, preferably right after a feeding when the baby is in that "milk coma" state.
Lastly, check the pulses. You can do this at home. Feel your baby's femoral pulse (in the groin area) and compare it to the pulse in their wrist. They should feel equally strong and happen at the same time. If the groin pulse feels weak or delayed, mention it to your pediatrician immediately. It’s a simple at-home check that can provide a huge clue for the doctors.
Don't panic over one weird number. Babies are inconsistent. They are growing, their blood vessels are expanding, and their systems are calibrating. The infant blood pressure chart is a guide, not a final verdict. Trust the trends, watch the growth curves, and always advocate for a re-measure if the first one was taken while the baby was screaming their head off.