You’re sitting in a cramped exam room and your cardiologist turns the monitor toward you. On the screen, there's a grainy, flickering grayscale video of what looks like a series of lightning bolts or a river delta seen from a satellite. These are images of heart arteries, and honestly, to the untrained eye, they look like a chaotic mess of shadows. But for a specialist, this is the most important map they will ever read. It's the literal plumbing of your life force.
Most people think these pictures are just about finding "clogs." It's more complicated.
When we talk about visualizing the coronary system, we aren't just looking at one thing. We are looking at flow, wall thickness, and the terrifyingly specific way calcium deposits itself in the vessel lining. It’s the difference between a garden hose that’s kinked and one that’s slowly filling up with sand. One is an easy fix; the other is a ticking clock.
The Raw Reality of Coronary Angiography
The gold standard—the big kahuna of images of heart arteries—is the coronary angiogram. This isn't some passive "sit in a tube" experience. They actually thread a catheter through your wrist or groin, snake it up to the heart, and squirt iodine-based dye directly into the openings of the coronary arteries.
It’s invasive. It’s intense. But it's the only way to see "real-time" hemodynamics.
I remember talking to a technician at the Cleveland Clinic who described the process as "filming a high-speed chase through a tunnel that's constantly moving." Because the heart is beating, the arteries are whipping around like snakes. The software has to compensate for that motion just so the doctor can see if that 70% blockage is actually a 90% disaster waiting to happen.
Sometimes the dye reveals a "stenosis," which is just a fancy medical term for a narrowing. On the screen, it looks like someone pinched the straw. If that pinch is in the Left Main Coronary Artery—often nicknamed the "Widowmaker"—the vibe in the room changes instantly.
Why Static Photos Can Be Deceiving
A single snapshot doesn't tell the whole story. You could have an image that looks relatively "clean," but if the artery wall is "remodeling" outward, the plaque is hiding in the wall itself rather than the channel. This is what doctors call "positive remodeling." It’s sneaky. The channel looks wide, but the wall is fat with unstable, "soft" plaque that could rupture at any second.
This is why we’ve moved toward things like Intravascular Ultrasound (IVUS). Instead of looking from the outside in, they put a tiny ultrasound probe inside the artery. It’s like taking a GoPro through a sewer pipe. You see the layers. You see the different types of gunk.
👉 See also: The Stanford Prison Experiment Unlocking the Truth: What Most People Get Wrong
- Calcified plaque: Hard as a rock. It shows up bright white on an ultrasound or CT scan because the signal bounces right off it.
- Lipid-rich cores: These are the dangerous ones. They’re soft, mushy, and prone to "popping," which causes a sudden blood clot and a heart attack.
- Fibrotic tissue: Scarring. It's more stable than fat but still takes up space.
The Rise of the "Virtual" Heart Scan
Not everyone needs a tube in their arm. For many, the first time they see images of heart arteries is through a CCTA (Coronary Computed Tomography Angiography).
It's basically a super-powered X-ray.
The tech has jumped lightyears ahead in just the last few years. We used to get blurry images if the patient's heart rate was over 60 beats per minute. Now, with "multi-slice" scanners (we're talking 64, 128, or even 320 slices), the computer can reconstruct a 3D model of your heart in the time it takes you to hold your breath once.
It’s breathtaking, honestly. You can rotate the heart on a screen, strip away the muscle, and just look at the "tree" of arteries.
But there's a catch.
CT scans struggle with "blooming artifacts." If you have a lot of calcium, the bright white spots "bleed" in the image, making a small blockage look much bigger than it actually is. It’s like taking a photo of a lightbulb—the glow makes the bulb look huge. Doctors have to be careful not to over-diagnose based on a "bright" CT.
The Calcium Score: A Different Kind of Image
You might have heard of a "Calcium Score" or Agatston Score. This is a low-dose CT scan without dye. It doesn't show the blockages themselves; it just shows the "scabs" of old damage.
- Score of 0: You're basically in the clear for now.
- Score of 1-100: Mild buildup. Time to look at your diet.
- Score of 100-400: Moderate. You probably need a statin.
- Score of 400+: High risk. You need to see a specialist yesterday.
It's a blunt tool, but it's a powerful one because it’s objective. It doesn't care how "healthy" you feel. If the calcium is there, the disease is there.
✨ Don't miss: In the Veins of the Drowning: The Dark Reality of Saltwater vs Freshwater
Seeing the Unseen: Microvascular Disease
Here is the thing nobody talks about.
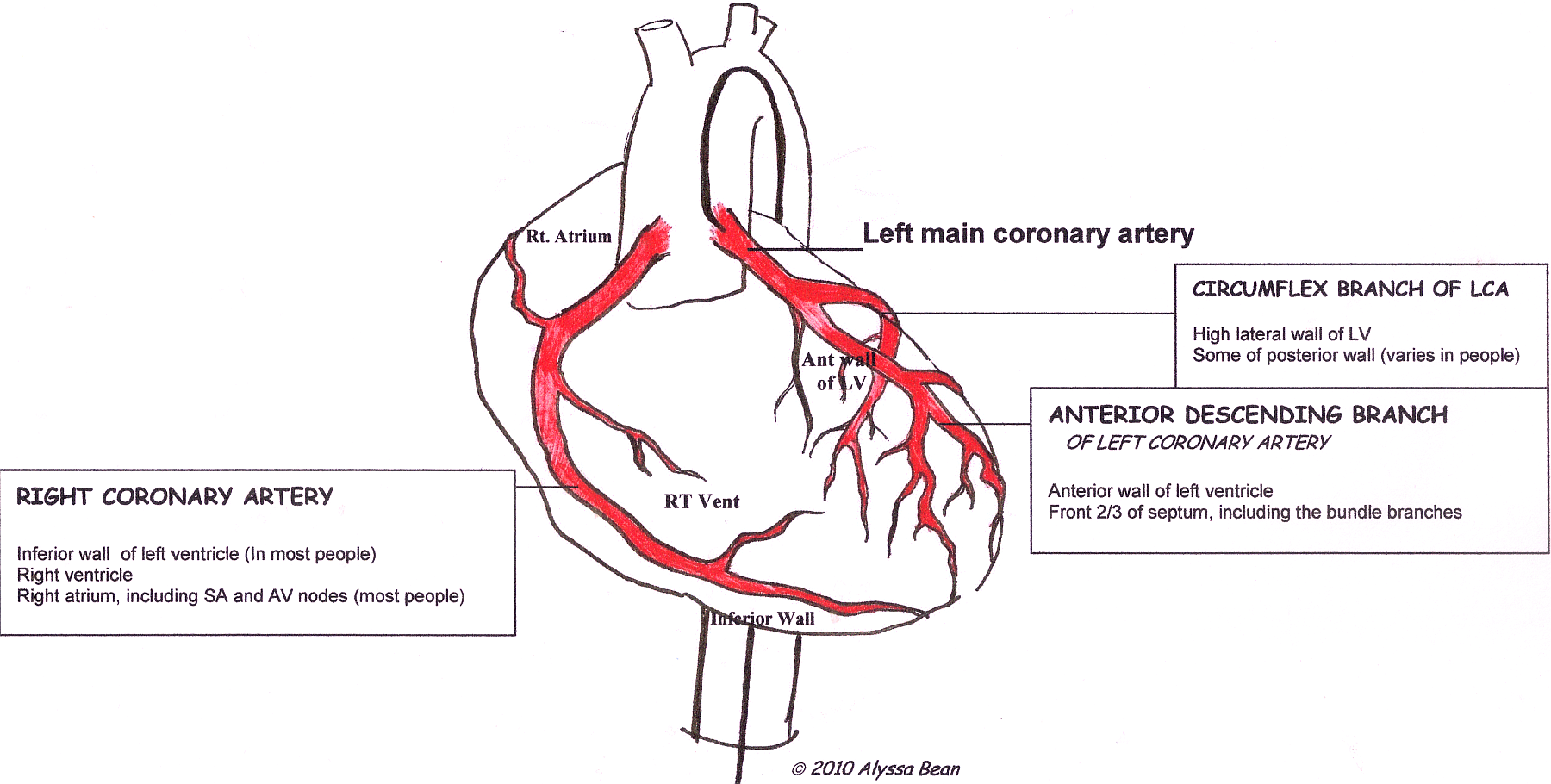
You can have "perfect" images of heart arteries on an angiogram and still have crushing chest pain. Why? Because those big arteries you see on the screen—the LAD, the Circumflex, the Right Coronary—are only the "highways."
There are miles and miles of tiny "surface streets" called the microvasculature. These vessels are too small to be seen on a standard scan.
Conditions like Microvascular Dysfunction (MVD) often affect women more than men. A woman might go to the ER with heart attack symptoms, get an angiogram, be told her "arteries are clear," and be sent home. It’s a tragedy of modern imaging.
To see this, we need specialized tests like Cardiac MRI or PET scans that measure "Myocardial Blood Flow" (MBF). Instead of looking at the pipes, we look at how the "lawn" (the heart muscle) gets watered. If the lawn is dying even though the main sprinkler pipe is open, we know the tiny sprinklers are clogged.
AI and the Future of Cardiac Imaging
We are currently entering the era of FFR-CT (Fractional Flow Reserve from CT).
In the old days, to know if a blockage was actually stopping blood flow, a doctor had to physically put a pressure-wire across the blockage during a procedure. Now, we use supercomputers.
Companies like HeartFlow take those 3D images of heart arteries and run complex fluid dynamics simulations on them. They can tell the doctor, "Hey, this blockage looks like 50%, but because of the way the blood swirls here, it's actually causing a significant drop in pressure."
🔗 Read more: Whooping Cough Symptoms: Why It’s Way More Than Just a Bad Cold
It’s "digital twin" technology. They build a digital version of your heart and "test" it before they ever touch you with a needle.
Understanding Your Results
When you finally get that report back, don't panic at every word. Radiology reports are written in a weird, defensive dialect of "med-speak."
If you see "tortuous vessels," it just means your arteries have some extra curves. Like a winding road. It's usually fine.
If you see "luminal narrowing," that's the one to pay attention to.
"Patent" is a great word. It means "open."
But remember, an image is just a moment in time. Plaque is dynamic. It’s a living part of your biology. It can be stabilized with medication, exercise, and aggressive cholesterol management.
Actionable Steps for Your Heart Health
If you are looking at or scheduled for images of heart arteries, here is exactly how to handle it:
- Ask for the "Why": If your doctor orders a CT, ask if they are looking for calcium or for actual blockages (angiography). They are different tests with different radiation levels.
- Request the Disk: You are legally entitled to your imaging data. Get the CD or the digital portal access. If you ever need a second opinion at a major center like Mayo Clinic or Johns Hopkins, having the actual images—not just the typed report—is vital.
- Context Matters: An image of a 50% blockage in a marathon runner means something very different than a 50% blockage in someone with uncontrolled diabetes and high blood pressure.
- Check the "Functional" Side: If your anatomy looks okay but you still have symptoms, push for a "functional" test like a Stress Echo or a PET scan. Don't let a "clean" picture gaslight you if you can't walk up a flight of stairs without chest pressure.
- Hydrate Before Dye: If you're getting an angiogram or CCTA, the contrast dye is hard on the kidneys. Drink plenty of water the day before and the day after to flush it out, unless your doctor has you on fluid restrictions.
The technology is getting better every day. We are moving away from grainy shadows and toward crystal-clear, 4D maps of the human engine. It's an incredible time for preventative medicine, but it only works if you understand what you're looking at. Stay curious, ask the hard questions, and don't treat those images as a final sentence—treat them as a tactical map for your recovery.