You’re staring at a red bump. It’s itchy, maybe a little sore, and your first instinct is to grab your phone and start scrolling through images of early stages of staph infection to see if your skin matches the horror stories. It’s a common panic. Most people assume a staph infection looks like a cinematic disaster from day one, but honestly, it usually starts out looking like absolutely nothing special. It looks like a bug bite. It looks like a pimple that won't quit.
Staph is sneaky. Staphylococcus aureus is a bacteria that lives on the skin of about 30% of the population without causing a single problem. It’s just hanging out. But the second there’s a micro-tear from a razor, a scratch from a cat, or a blister from new shoes, that bacteria moves in. Understanding the visual progression is less about finding a "perfect" match in a photo and more about recognizing how the skin is reacting to an invader.
The "Pimple" Phase: Spotting the early signs
When you search for images of early stages of staph infection, you’ll see a lot of small, red bumps. These are often mistaken for folliculitis—which is just an inflamed hair follicle—or a simple whitehead. At this point, the area is usually localized. It might be slightly raised. You might notice a tiny bit of pus at the center, looking like a yellowish dot.
Here is the thing: a normal pimple usually calms down. Staph doesn't.
If that "pimple" starts to feel firm or warm to the touch, the bacteria are multiplying. This is the stage where the infection is technically a boil, or a furuncle. Dr. Sandra Lee (widely known as Pimple Popper) often points out that you should never squeeze these. Why? Because the pressure can actually push the Staph bacteria deeper into your dermis or, worse, into your bloodstream. That is how a localized skin issue becomes a systemic medical emergency.
Is it a spider bite or staph?
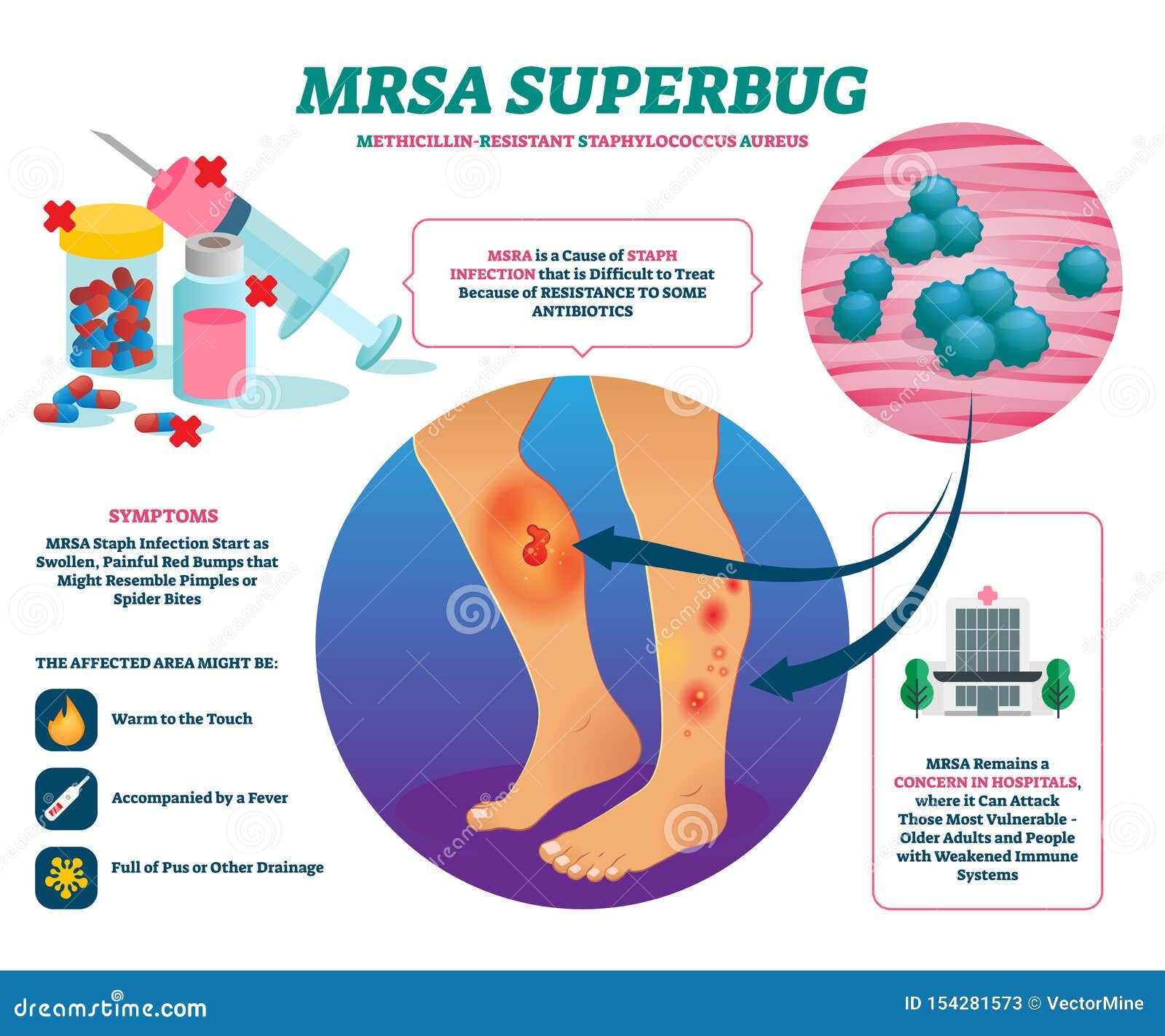
This is the big one. Almost everyone who walks into an urgent care with a "spider bite" actually has a staph infection, specifically MRSA (Methicillin-resistant Staphylococcus aureus). Real spider bites are actually quite rare compared to the frequency of staph. If you see a red, swollen lesion with a dark or necrotic (black) center, don’t go looking for a spider. Look for a doctor. The "bullseye" look is a classic early-stage visual for a staph-related abscess.
📖 Related: Blackhead Removal Tools: What You’re Probably Doing Wrong and How to Fix It
Cellulitis: The redness that moves
Sometimes staph doesn't stay in a little bump. It spreads out. This is called cellulitis. If you’re looking at images of early stages of staph infection that show flat, red, and swollen skin rather than a distinct lump, you’re likely looking at this. It feels like the skin is tight. It might look "pitted," almost like the skin of an orange.
Doctors often use a sharpie to trace the border of the redness. If the red area expands past that line in a few hours, the infection is winning the race.
Early cellulitis is subtle. It might just look like a mild sunburn on one leg. But if it’s only on one side of your body—say, your left calf is red but your right is fine—that’s a massive red flag. Symmetrical redness is often an allergy or circulation issue; asymmetrical redness is usually an infection.
Impetigo and the "Honey-Crust" look
In kids, and sometimes athletes, staph manifests as impetigo. This looks very different from the boils we discussed. The early stages often feature small blisters that pop easily. Once they pop, they leave behind a very specific visual: a honey-colored crust.
It’s gross. It’s also incredibly contagious.
👉 See also: 2025 Radioactive Shrimp Recall: What Really Happened With Your Frozen Seafood
If you see these yellowish, crusty patches around the nose or mouth, you’re looking at a classic staph or strep presentation. It doesn't usually hurt much, but it itches like crazy. Scratching it is the fastest way to move the bacteria to other parts of the body or to other people. This is why wrestling mats and gym equipment are notorious breeding grounds.
The heat test and other non-visual cues
You can't rely solely on your eyes. Your sense of touch is just as important when evaluating images of early stages of staph infection against your own skin.
- The Temperature Check: Take the back of your hand and touch the red area. Then touch the same spot on the opposite side of your body. Is the red spot significantly hotter? Heat is a byproduct of your white blood cells fighting a war.
- The Pain Scale: Does it hurt more than it looks like it should? Staph infections often have a "deep" ache that feels disproportionate to the size of the bump.
- The Fluid Factor: Is it draining? Clear fluid is usually okay. Cloudy, yellow, or foul-smelling pus is a sign that the staph population is booming.
Why MRSA changed the game
We have to talk about MRSA because it’s the version of staph that keeps doctors up at night. Visually, it can look identical to a "normal" staph infection. You cannot tell the difference just by looking at a photo.
The difference is in the resistance. Standard staph responds to basic antibiotics like cephalexin. MRSA laughs at them. If you are looking at your infection and it seems to be getting worse despite using an over-the-counter antibiotic cream like Neosporin, stop. Staph is increasingly resistant to the triple-antibiotic ointments we keep in our medicine cabinets.
When to stop Googling and go to the ER
Visuals only take you so far. There is a point where the "early stage" ends and the "danger zone" begins. If you see red streaks radiating away from the initial bump, that is a sign of lymphangitis. Basically, the infection is traveling through your lymphatic system.
✨ Don't miss: Barras de proteina sin azucar: Lo que las etiquetas no te dicen y cómo elegirlas de verdad
That is not a "wait and see" situation. That is an "ER right now" situation.
The same goes for systemic symptoms. If you have a red bump and you also feel like you have the flu—chills, fever, body aches—the bacteria may have entered your blood. This can lead to sepsis, endocarditis (infection of the heart valves), or osteomyelitis (bone infection).
Practical steps for managing a suspected staph spot
If your skin looks like some of the milder images of early stages of staph infection, you need a plan that doesn't involve "popping" it.
- Clean and Cover: Wash the area gently with Hibiclens (chlorhexidine) or a simple fragrance-free soap. Cover it with a clean bandage. This keeps you from touching it and prevents the bacteria from hitching a ride on your fingers.
- Warm Compresses: Use a clean washcloth soaked in warm water. Apply it for 10 minutes several times a day. This can help the infection "come to a head" naturally without the trauma of squeezing.
- No Sharing: Don't share towels, razors, or gym gear. If it is staph, it's looking for its next host.
- Monitor the Border: Take a pen and draw a circle around the redness. This is the most objective way to tell if it's spreading. If the redness marches past that ink line, call your primary care physician or head to urgent care.
The reality of staph is that early detection makes treatment boring—usually just a round of oral antibiotics. Late detection makes treatment a hospital stay with an IV drip. If your "pimple" is throbbing, hot, and spreading, trust your gut over a Google image search. Most staph infections are easily cured if you catch them while they still look like a minor annoyance. If you have a fever or the pain is keeping you awake, skip the home remedies and get a professional opinion immediately. High-risk individuals, such as those with diabetes or weakened immune systems, should never wait for "clearer" symptoms to emerge. Early intervention is the only way to prevent a localized skin issue from becoming a life-altering event.