You’re sitting in a cold exam room, clutching a CD-ROM or staring at a grainy black-and-white screen while a doctor points at shadows. It’s a weird experience. Most people look at images of arthritis in the knee and see a Rorschach test of blobs and static. But those pixels are actually a roadmap of why your morning walk feels like grinding glass. Honestly, the biggest mistake people make is thinking that a "bad" picture always means a "bad" life. It doesn't.
Medical imaging has come a long way from the blurry plates of the 1950s. Today, we have high-resolution digital radiography, 3T MRI machines, and weight-bearing CT scans that show exactly how your joints behave under pressure. However, there is a massive disconnect between what the camera sees and what the patient feels. It’s a paradox. You can have a knee that looks like a "train wreck" on an X-ray but feels totally fine, or a knee that looks pristine while the owner is in constant agony.
Understanding what these images represent—and what they don't—is the first step in taking back control.
The Bone-on-Bone Myth and What X-rays Really Show
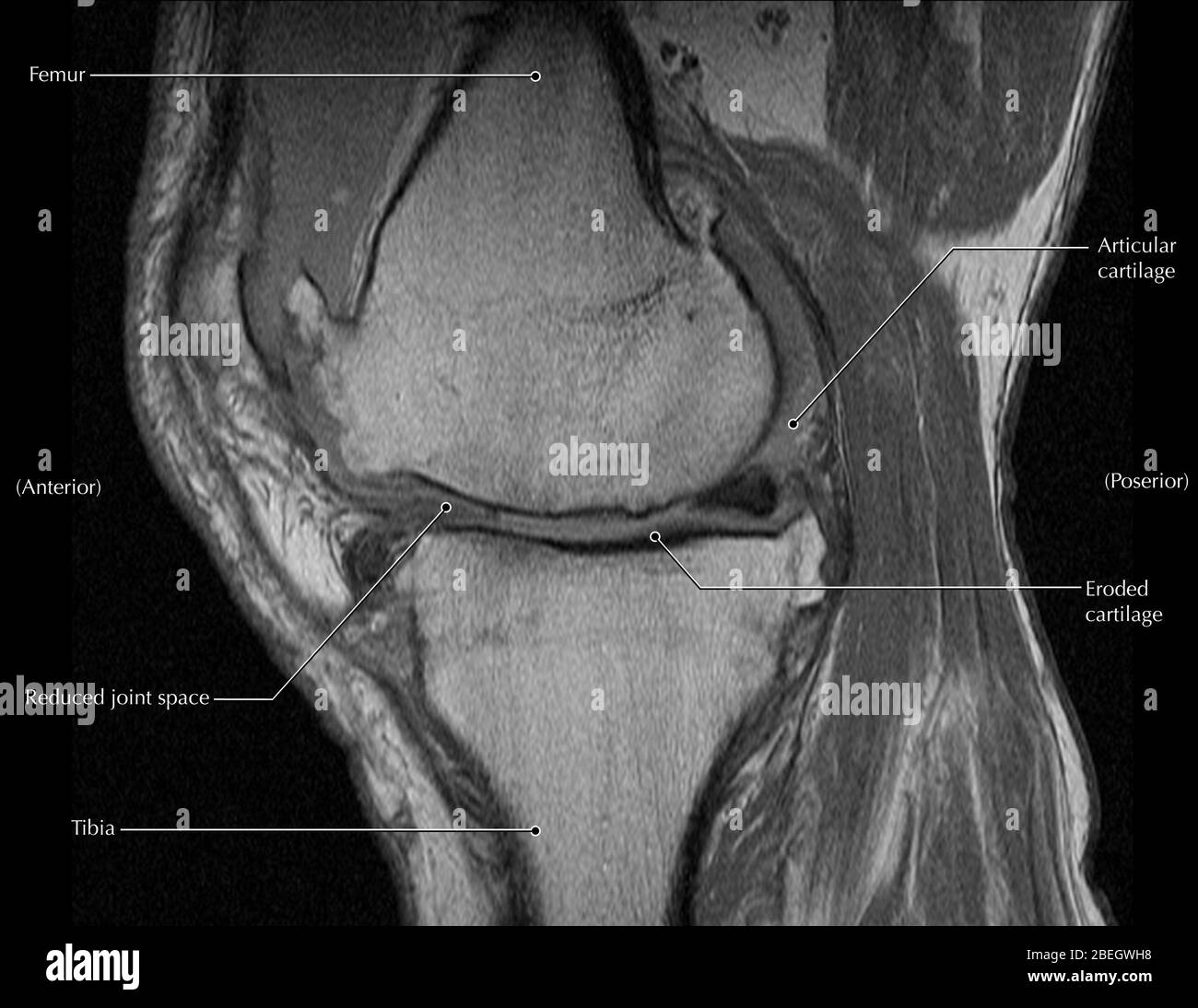
When people search for images of arthritis in the knee, they are usually looking for one thing: the gap. Or the lack of one. In a healthy knee, there’s a clear dark space between the femur (thigh bone) and the tibia (shin bone). That’s your cartilage. Well, technically, cartilage is invisible on an X-ray. The "space" you see is just the room the cartilage occupies.
Osteoarthritis (OA) is basically the thinning of that buffer.
As the cartilage wears down, the bones get closer. Doctors call this "joint space narrowing." When the gap vanishes, you get the dreaded "bone-on-bone" diagnosis. But here’s the thing: bone isn't just sitting there being passive. When it starts rubbing, it reacts. It gets angry. It builds reinforcements.
📖 Related: Dr. Sharon Vila Wright: What You Should Know About the Houston OB-GYN
Osteophytes and Sclerosis
Look closely at an advanced image of an arthritic knee. You’ll see little jagged "beaks" poking out from the edges of the joint. These are osteophytes, commonly known as bone spurs. Your body is trying to increase the surface area of the joint to redistribute the load. It’s a survival mechanism. You might also notice areas where the bone looks "whiter" or more dense than the rest. This is subchondral sclerosis. The bone is literally thickening itself because it’s taking too much impact. It’s like a callous on your hand, but inside your leg.
Why an MRI Sees the Stuff X-rays Miss
If an X-ray is a grainy polaroid, an MRI is a 4K documentary. While X-rays are great for looking at the "hard" stuff (bone), MRIs are the gold standard for "soft" tissues. This is where we see the meniscus, the ligaments, and the bone marrow itself.
Sometimes, images of arthritis in the knee taken via MRI reveal something called Bone Marrow Lesions (BMLs). These look like bright white clouds inside the bone. They represent swelling and micro-fractures. Research from the Journal of Orthopaedic Research suggests these lesions are actually a better predictor of pain than cartilage loss itself. If you have bone-on-bone images but no marrow edema, you might actually be asymptomatic. If you have those bright spots, you're likely hurting.
The Meniscus Factor
You also have the meniscus—two C-shaped pieces of tough, rubbery cartilage that act as shock absorbers. In arthritic images, the meniscus is often frayed or "extruded," meaning it’s been squeezed out of the joint like toothpaste. This changes the mechanics of everything. Once that shock absorber is out of place, the bone-on-bone progression accelerates. It’s a chain reaction.
Comparing Mild, Moderate, and Severe Stages
Visualizing the progression helps put your own diagnosis in context. It isn't a straight line for everyone, but there are distinct visual markers.
👉 See also: Why Meditation for Emotional Numbness is Harder (and Better) Than You Think
In Mild (Stage 1 or 2) images, the knee looks mostly normal. You might see a tiny, sharp point at the edge of the bone. Maybe a 10% loss of joint space. Most people at this stage think they just "overdid it" at the gym. They aren't looking for images yet.
By Moderate (Stage 3), the changes are undeniable. The joint space is visibly lopsided. Usually, the inner (medial) side of the knee collapses first, leading to a bow-legged appearance. You’ll see multiple bone spurs. The bone surface might look irregular instead of smooth and rounded.
Severe (Stage 4) is the "end-stage." The gap is gone. The bones are touching. There are large osteophytes that can actually limit how far you can straighten or bend your leg. At this point, the "image" of the knee often dictates the conversation about joint replacement surgery.
The Problem with "Scan-xiety"
We need to talk about the psychological impact of seeing your own imaging. There’s a documented phenomenon where patients who are told their X-rays look "terrible" actually start reporting higher levels of pain. It’s a "nocebo" effect.
Dr. David Hunter, a world-renowned osteoarthritis expert at the University of Sydney, often emphasizes that we treat the person, not the image. The image is a snapshot. It doesn't show your muscle strength, your inflammation levels on that specific day, or your neurological pain threshold.
✨ Don't miss: Images of Grief and Loss: Why We Look When It Hurts
Some of the most "arthritic-looking" knees belong to retired pro athletes who still hike ten miles a week. Why? Because they have massive quadriceps and hamstrings that act as external stabilizers, taking the pressure off the internal joint. The image shows the damage, but it doesn't show the compensation.
New Technology: The Future of Knee Imaging
We are moving past static pictures. Weight-bearing CT (WBCT) is a game-changer. Standard X-rays are often taken while you’re lying down or standing still. But we don't live our lives lying down. WBCT captures the joint while it's under the actual stress of your body weight, often revealing that the "space" seen on a normal X-ray actually disappears the moment you stand up.
There’s also "compositional MRI." This doesn't just look at the shape of the cartilage; it looks at the chemical makeup. It can detect the loss of proteoglycans (the molecules that hold water in the cartilage) years before the cartilage actually thins out. This is the "early warning system" we’ve been waiting for.
What to Look for in Your Own Report
When you get your radiology report back, don't just look for the word "arthritis." It’ll be there—almost everyone over 40 has some. Look for these specific terms:
- Tri-compartmental: This means the arthritis is in all three parts of the knee (inner, outer, and behind the kneecap).
- Chondromalacia: A fancy word for the softening of the cartilage.
- Subchondral cysts: Small fluid-filled holes in the bone just below the cartilage surface.
- Joint effusion: Swelling. This is the "water on the knee" that makes it feel tight.
Actionable Steps: Beyond the Image
So you’ve seen the images of arthritis in the knee and they aren't great. What now?
First, stop obsessing over the "bone-on-bone" phrase. It’s a scary term that often leads to unnecessary fear-avoidance behavior. If you stop moving because you’re afraid of "wearing it out," the muscles around the knee will atrophy. When the muscles weaken, the joint takes even more impact. It’s a death spiral for joint health.
- Strengthen the "Shock Absorbers": Focus on the glutes and quads. A strong leg can offload up to 30% of the pressure on the knee joint.
- Weight Management: Every pound you lose is four pounds of pressure off your knee during a single step. That is a massive multiplier.
- Low-Impact Movement: Cartilage doesn't have a blood supply. It gets its nutrients through "diffusion," which only happens when the joint is loaded and unloaded. Movement is literally medicine for the cartilage that’s left.
- Footwear Check: Sometimes a simple lateral wedge in your shoe can "open up" the side of the knee that looks collapsed on the X-ray. It’s called "offloading."
- Inflammation Control: Arthritis is as much an inflammatory disease as it is a mechanical one. Diet, sleep, and stress management change the chemistry of the fluid inside that joint, regardless of what the bone looks like.
The image is just one piece of the puzzle. It’s a baseline, not a destiny. Use the pictures to understand your anatomy, but let your function and your pain levels dictate your treatment. Most people can significantly improve their quality of life without ever "fixing" the image itself.