You’ve probably seen them on a grainy monitor in a hospital hallway or maybe while doom-scrolling through medical diagrams late at night. Images of arteries of the heart usually look like a tangled mess of red lightning bolts or a roadmap of a city you’ve never visited. It’s a bit overwhelming. But honestly, these visuals are the literal lifelines of your body.
They matter.
When a cardiologist stares at a screen, they aren't just looking for "clogs." They are looking at flow dynamics, vessel wall integrity, and the weird way your specific anatomy branches out. No two hearts are identical. Some people have a "right-dominant" system; others are "left-dominant." It’s basically the plumbing of your soul, and if the pipes get narrow, everything else starts to fail.
Why images of arteries of the heart look so different depending on the test
If you get an EKG, you aren't seeing the arteries. You're seeing the electricity. To actually see the vessels, doctors have to use some pretty heavy-duty tech.
The gold standard is the coronary angiogram. This isn't just a picture; it’s a live-action movie. Doctors thread a catheter up to the heart and inject a contrast dye. On the X-ray (fluoroscopy), the arteries suddenly pop into view as dark, flowing rivers against a ghostly white background. If there’s a blockage, the river narrows to a tiny thread. Doctors call this a "lesion." It looks like someone pinched a garden hose.
Then you have the CT Coronary Angiogram (CCTA). This is the one that produces those cool, 3D rotating models you see in health tech commercials. It’s non-invasive, which is great, but it’s essentially a massive data-crunching exercise. The computer takes hundreds of "slices" of your chest and stitches them together. It’s fantastic for seeing calcium buildup—those white crunchy bits that shouldn't be there.
The Left Main: The "Widowmaker" and other scary names
You’ve heard the term. It sounds terrifying. The Left Anterior Descending (LAD) artery is the one people usually mean when they talk about the Widowmaker.
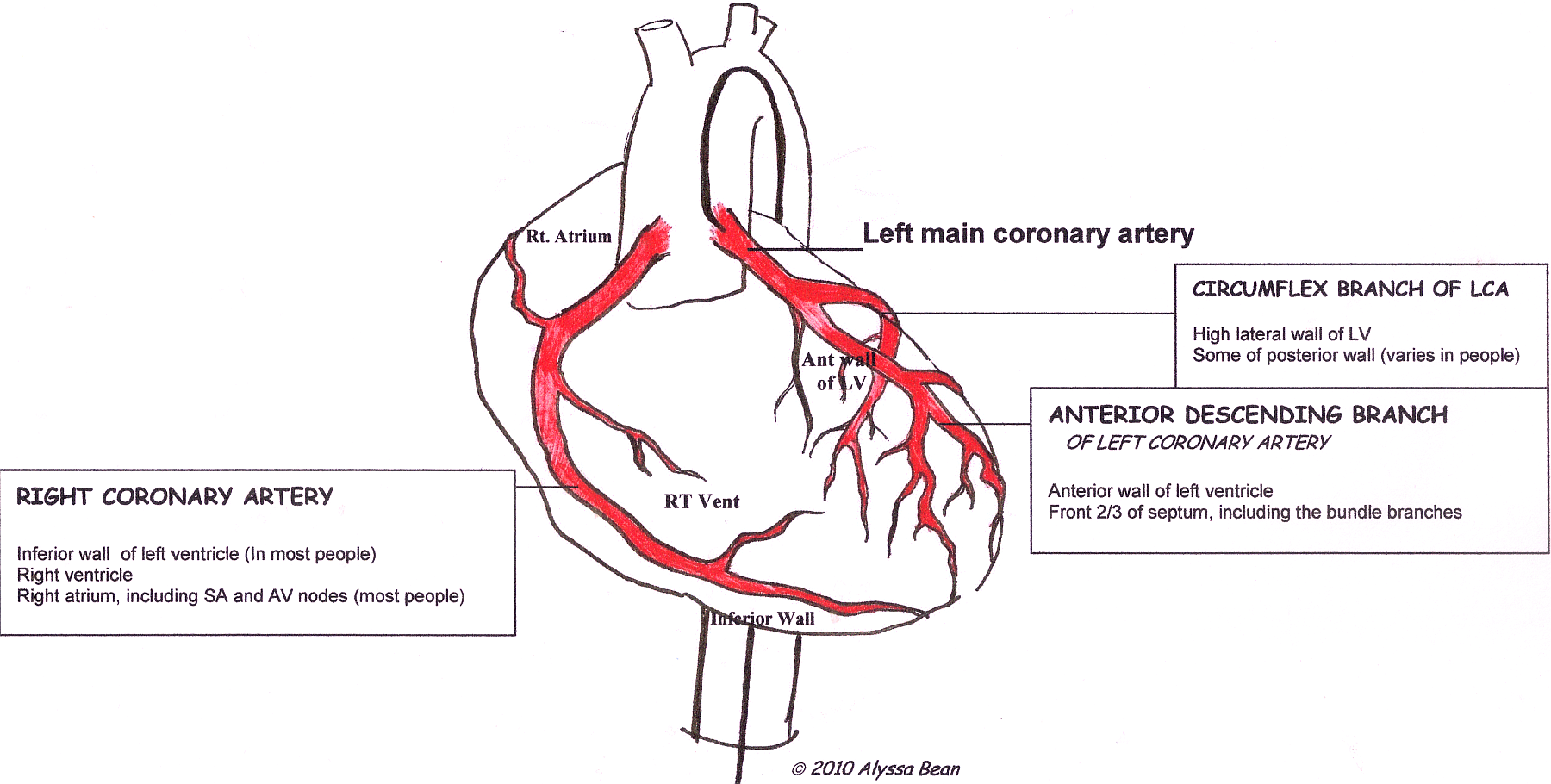
Why the drama? Because the LAD supplies about 50% of the blood to the heart’s left ventricle. If you look at images of arteries of the heart, the LAD is the big one running right down the front. If it shuts down, the pump stops.
But it’s not the only player. You also have the Circumflex artery, which wraps around the side like a hug, and the Right Coronary Artery (RCA), which handles the bottom and back. When a doctor looks at these images, they’re checking the "lumen"—the open space inside the tube. Even a 50% narrowing might not cause symptoms while you're sitting on the couch, but try running for a bus, and your heart starts screaming for oxygen it can't get.
👉 See also: The Stanford Prison Experiment Unlocking the Truth: What Most People Get Wrong
The weird science of "Soft Plaque" vs. Calcium
Most people think of heart disease as a slow buildup of "gunk," like old pipes in a 1920s Victorian house. That’s partially true. But the images tell a more complex story.
There is calcified plaque, which shows up bright white on a CT scan. It’s hard. It’s stable. In a weird way, it’s the "safer" kind because it’s not likely to suddenly burst. Then there’s the "soft plaque" or non-calcified lipid pools. These are the real villains. On many standard images of arteries of the heart, soft plaque is almost invisible or looks like a faint shadow.
This is why some people pass a stress test and then have a heart attack a week later. The "vulnerable plaque" ruptures, a clot forms instantly, and the road is closed.
What an Intravascular Ultrasound (IVUS) reveals
Sometimes, looking from the outside isn't enough. Doctors actually have a tiny ultrasound camera they can put inside the artery.
It’s wild.
The IVUS gives a 360-degree view from the inside out. It looks like a cross-section of a tree trunk. You can see the layers of the artery wall: the intima, the media, and the adventitia. If there’s a "stent" in there—a little metal mesh tube—the IVUS shows if it’s actually pressed up against the walls or if it’s floating uselessly in the middle.
Understanding the "Tree" of your heart
Think of it like an upside-down tree.
The Aorta is the trunk. The coronary arteries are the first branches that sprout off, right at the base. It’s a bit selfish of the heart, really—it takes the best, most oxygenated blood for itself before sending the rest to your brain and toes.
✨ Don't miss: In the Veins of the Drowning: The Dark Reality of Saltwater vs Freshwater
- Left Main Coronary Artery: The short, thick starting point on the left side.
- LAD: The "front" branch.
- Circumflex: The "side/back" branch.
- RCA: The "right and bottom" branch.
When you see these in an image, you're looking for "tortuosity." That’s a fancy word for twisty. Some people have very straight arteries; others have vessels that loop-the-loop. High blood pressure often makes these vessels more tortuous over time, like a hose that’s being pushed with too much water pressure and starts to kink.
Limitations of the pictures
We love technology, but it’s not perfect.
Images of arteries of the heart can sometimes be misleading. For example, "artifact" is a huge problem. If a patient breathes or moves during a CT scan, the image might show a "step-off" that looks like a blockage but is actually just a blurry photo.
Also, there is Microvascular Disease. This is huge, especially for women. The big arteries—the ones we can see on an angiogram—might look perfectly clean. Smooth as silk. But the tiny, microscopic vessels branching off them are constricted or damaged. These don't show up on standard images. You could have "clear" arteries and still have significant chest pain (angina) because the "irrigation system" for the heart muscle is failing at the microscopic level.
Digital reconstructions and the future of heart imaging
We’re moving toward Fractional Flow Reserve (FFR-CT).
Basically, instead of just looking at a picture and guessing how bad a blockage is, supercomputers calculate the actual fluid dynamics. They simulate blood flow through the 3D model of your heart. It tells the doctor: "Hey, this narrowing looks scary, but the pressure on the other side is actually fine. Leave it alone." This prevents unnecessary stents and surgeries.
It turns a static image into a functional map.
How to read your own report (sorta)
If you’re looking at your own medical images or the radiologist’s report, look for these keywords:
🔗 Read more: Whooping Cough Symptoms: Why It’s Way More Than Just a Bad Cold
- Stenosis: This means narrowing. 70% stenosis is usually the threshold where doctors start considering an intervention like a stent.
- Bifurcation: Where one artery splits into two. These are high-stress areas where plaque loves to hide.
- Collateral Circulation: This is actually cool. If a main artery closes slowly over years, your heart might grow its own "detour" tiny vessels to bypass the clog. It’s the body’s natural bypass surgery.
- Patent: This is a good word! It means "open." If your stent is "patent," it’s doing its job.
What you should actually do with this information
Seeing images of arteries of the heart shouldn't just be a biology lesson. It should be a wake-up call or a relief.
If you have a family history of heart issues, don't wait for a "grabber" chest pain to get checked. Ask about a Calcium Score scan. It’s a low-dose CT that takes about 10 minutes and doesn't require needles or dyes. It gives you a number.
- Score 0: Great.
- Score 1-100: Mild buildup.
- Score 400+: You need to talk to a cardiologist yesterday.
It is the single most predictive "image" you can get for future heart risk.
Also, keep an eye on your "numbers" beyond the images. Blood pressure and LDL cholesterol are the two things that physically damage the lining of those arteries (the endothelium). Once that lining is nicked, plaque starts to stick. It’s like a pothole on a highway—once it starts, it only gets bigger as cars (cholesterol) hit it.
Next Steps for Your Heart Health:
- Get a Calcium Score: If you’re over 40 and have risk factors, this is the most actionable "image" you can get. It’s often not covered by insurance (costs about $100-$150), but it provides more clarity than a basic cholesterol test.
- Review your "Lumen" health: If you already have images, ask your doctor specifically about "soft plaque" vs. "calcified plaque." The strategy for treating them can differ.
- Check the Microvasculature: If you have chest pain but "clear" big arteries, ask about a stress MRI or a PET scan, which can look at blood flow through the smaller vessels that standard angiograms miss.
- Monitor the Endothelium: Use a home blood pressure cuff. Constant high pressure acts like sandpaper on the inside of your arteries, creating the very damage that shows up on these images years later.
The goal isn't just to have pretty pictures of your heart; it's to make sure those "rivers" keep flowing without obstruction. Stay proactive. The best time to worry about your heart's plumbing is before the leak starts.
Don't ignore the dull ache or the "indigestion" that only happens when you walk up stairs. Your heart doesn't have many ways to talk to you, and usually, it's just trying to tell you that the picture inside isn't looking so great.
References for further reading:
- Journal of the American College of Cardiology (JACC) on CCTA advancements.
- Cleveland Clinic’s Guide to Coronary Artery Anatomy.
- The Lancet: Comparisons of FFR-CT vs. Invasive Angiography.