You’re sitting in the doctor’s office, heart hammering against your ribs. The notification on your patient portal popped up an hour ago: "Abnormal." Specifically, it says you’re positive for high-risk Human Papillomavirus. It feels like a gut punch. You start mentally cataloging every partner you’ve had in the last decade, wondering who "gave" this to you or if your current partner has been unfaithful. Stop. Breathe. Honestly, there is a very real chance that your result isn't telling the whole story. The hpv false positive percentage is a figure that doesn't get nearly enough airtime in exam rooms, and it leads to a massive amount of unnecessary anxiety, expensive follow-up procedures, and strained relationships.
Testing isn't perfect. We want it to be, but biology is messy.
The reality is that "positive" doesn't always mean "infected," and it certainly doesn't mean "cancer." Most people don't realize that the highly sensitive molecular tests used today, like the Cobas or Onclarity assays, are designed to be "over-sensitive" on purpose. They’d rather tell ten healthy women they have HPV than miss one person who actually does. This bias toward caution is great for public health but can be a psychological nightmare for the individual patient.
The Math Behind the Panic: Understanding Your Risk
When we talk about the hpv false positive percentage, we have to look at clinical specificity. Most modern FDA-approved HPV tests have a clinical specificity of roughly 40% to 50% for predicting actual cervical intraepithelial neoplasia (CIN2+). That sounds shockingly low, doesn't it? It means that if you test positive, it doesn't automatically mean your cells are changing in a dangerous way.
Let's get into the weeds for a second. There is a difference between an "analytical" false positive and a "clinical" false positive. An analytical false positive is when the machine says the virus is there, but it literally isn't—maybe due to cross-reactivity with a different, harmless virus or some contamination in the lab. These are actually quite rare. The bigger issue is the clinical false positive. This is when the test correctly identifies the presence of HPV DNA or RNA, but that virus is just "passing through." It’s a transient infection that your immune system was going to clear anyway in six months. By labeling that as a "positive," the test is technically right about the virus but "wrong" about the threat to your health.
💡 You might also like: How to get rid of bloodshot eyes quickly without making the redness worse
Studies published in The Lancet Oncology have highlighted that while HPV DNA testing is superior to the old-school Pap smear for catching potential issues, the tradeoff is a surge in false positives. In younger populations, specifically those under 30, the rate of transient infections is so high that many countries don't even bother testing them for HPV because the "false positive" (clinically speaking) rate would be astronomical.
Why Your Body Might Be "Faking" a Positive
Cross-reactivity is a sneaky culprit. Sometimes, the probes used in the lab to find high-risk HPV types (like 16 or 18) accidentally latch onto low-risk types or even unrelated bacteria. If you have a particularly active case of bacterial vaginosis or even a heavy yeast infection during your swab, it can, in rare instances, interfere with the signal.
Then there’s the "latent" virus issue. Some experts, like Dr. Diane Harper, who was a lead researcher for the HPV vaccines, have pointed out that the virus can hide in basal cells at levels so low they don't cause disease. A super-sensitive test might pick up a few stray fragments of viral DNA. You aren't "sick." You aren't "contagious." But the computer spits out a "Positive" result anyway.
- The Age Factor: If you are 25, your chances of a "false" clinical positive are way higher than if you are 50.
- The Test Brand: Not all tests are created equal; some look for DNA, others look for mRNA (like the Aptima test), which tends to have a slightly better specificity because it only reacts when the virus is actually "active."
- Recent Activity: While doctors say it doesn't matter, some evidence suggests that recent intercourse or the use of certain vaginal products can occasionally mess with the sample quality, leading to inconclusive or "weak" positives that are often managed as full positives.
The Problem with "Better" Technology
We moved away from Pap smears as the primary screen because they missed too much. A Pap smear has a high "false negative" rate—it might miss up to 50% of precancerous lesions. So, the medical community pivoted to HPV DNA testing. It’s incredibly "sensitive." If the virus is there, even in a tiny amount, the test will find it.
But here is the kicker: high sensitivity usually means lower specificity.
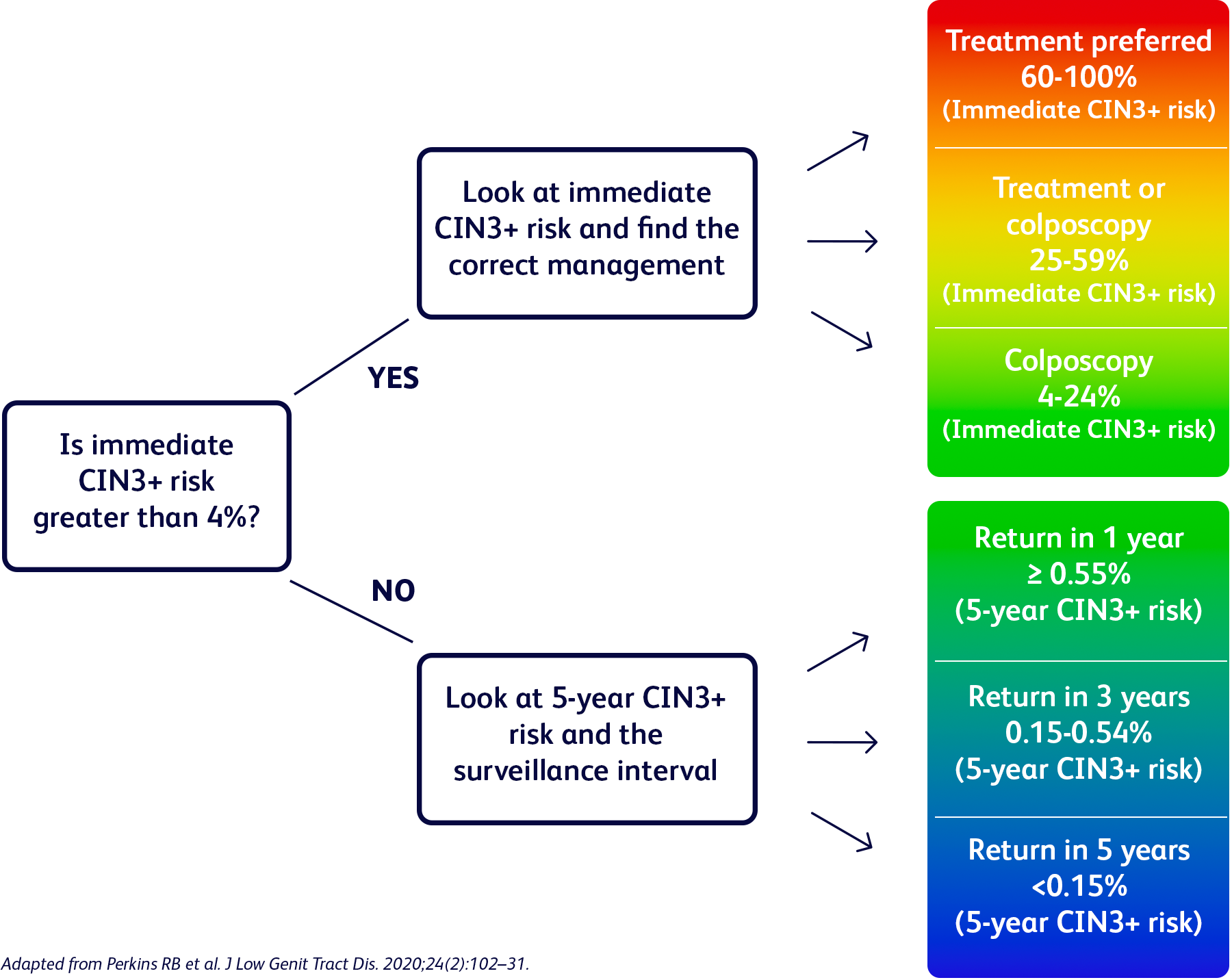
Imagine a smoke detector that is so sensitive it goes off every time you boil a pot of water. It’s doing its job—it's detecting "particles" in the air—but it's not a fire. A positive HPV test is often just the steam from the pasta water, yet we treat it like a three-alarm fire. This leads to the "over-treatment" pipeline. You get a positive result, then you’re scheduled for a colposcopy (where they look at your cervix with a microscope), and maybe even a biopsy. For many, the biopsy comes back as "normal" or "inflammation." That is the hpv false positive percentage in action. You just spent $800 and a week of sleepless nights for a result that didn't matter.
Navigating the "Abnormal" Result Without Losing Your Mind
So, what do you actually do? First, check which test was used. If it was an mRNA test, the result is slightly more likely to be clinically relevant than a standard DNA test. mRNA looks for the production of E6/E7 oncogenes—basically, it's checking if the virus is actually trying to turn your cells into monsters or if it's just napping.
Ask your doctor about the "Cycle Threshold" or the signal strength if available. While most labs just give a binary "Yes/No," some clinicians can see how "strong" the positive was. A weak positive is much more likely to be a fluke or a dying infection than a strong one.
Also, look at your Pap co-test. If the HPV is positive but the Pap is "NILM" (Negative for Intraepithelial Lesion or Malignancy), your immediate risk is actually very low. Most guidelines recommend just waiting a year and re-testing. That year is crucial. It gives your body time to do what it does best: clear the virus. About 90% of HPV infections are cleared by the immune system within two years. If you test positive today and negative in twelve months, that first test was—for all intents and purposes—a clinical false positive.
Moving Forward: Actionable Steps
Don't let a single lab report ruin your month. If you've received a positive result and you're worried about the hpv false positive percentage, take these specific steps:
Request a Co-test or Triage: If you only had an HPV test, ask for a reflex Pap smear. If the cells look fine, the HPV result is less urgent.
Wait and See is a Valid Strategy: For a first-time positive HPV result with a normal Pap, the standard of care is often a 12-month follow-up. Do not pressure your doctor into a biopsy immediately unless there are other risk factors. Give your immune system a chance to prove the test "wrong."
Check for "High-Risk" Typing: Not all HPV is the same. Ensure the lab specified if it is Type 16 or 18. If it's "Other High Risk," the chance of it being a transient, non-threatening infection is much higher.
Optimize Your Immune System: Stop smoking. Seriously. Smoking is the number one co-factor that prevents your body from clearing HPV. If you want that "false positive" to disappear by next year, put down the cigarettes. Take a quality folate supplement, as some studies suggest B9 deficiency is linked to persistent HPV.
Contextualize the Partner Talk: If you’re in a long-term relationship, a "new" positive HPV test does not mean someone cheated. The virus can remain subclinical (invisible) for decades. A positive test today could be from a partner you had in 2008.
The medical system is designed to catch the worst-case scenario, which is great for saving lives but terrible for your stress levels. Treat a positive HPV test as a yellow light, not a red one. It’s a signal to stay vigilant and follow up, but more often than not, it’s just a biological glitch in a system that errs on the side of caution.
Keep your follow-up appointments, but don't start writing your will. The odds are heavily in your favor that your body is already handling it.