You’re sitting on the couch, maybe scrolling through your phone or watching a game, and something feels... off. It isn't a bolt of lightning. It isn't a cinematic moment where you clutch your chest and collapse onto the rug. Honestly, for most people, it's just a weird, nagging discomfort that makes you wonder if you ate something spicy for lunch. That's the danger. The biggest hurdle in learning how to tell if you are have a heart attack is unlearning everything Hollywood taught you about "the big one."
It’s often quiet.
Sometimes it’s just a dull ache.
According to the Centers for Disease Control and Prevention (CDC), someone in the United States has a heart attack every 40 seconds. That is a staggering frequency. Yet, a massive chunk of those people wait hours before calling 911 because they aren't "sure" if it’s serious enough to bother the paramedics. They don't want to be embarrassed. They think it's just acid reflux or a pulled muscle from the gym. But when heart muscle starts dying from a lack of oxygenated blood, ego and embarrassment are the last things you should worry about.
Why your chest might not actually "hurt"
We talk about chest pain like it’s a requirement. It isn’t.
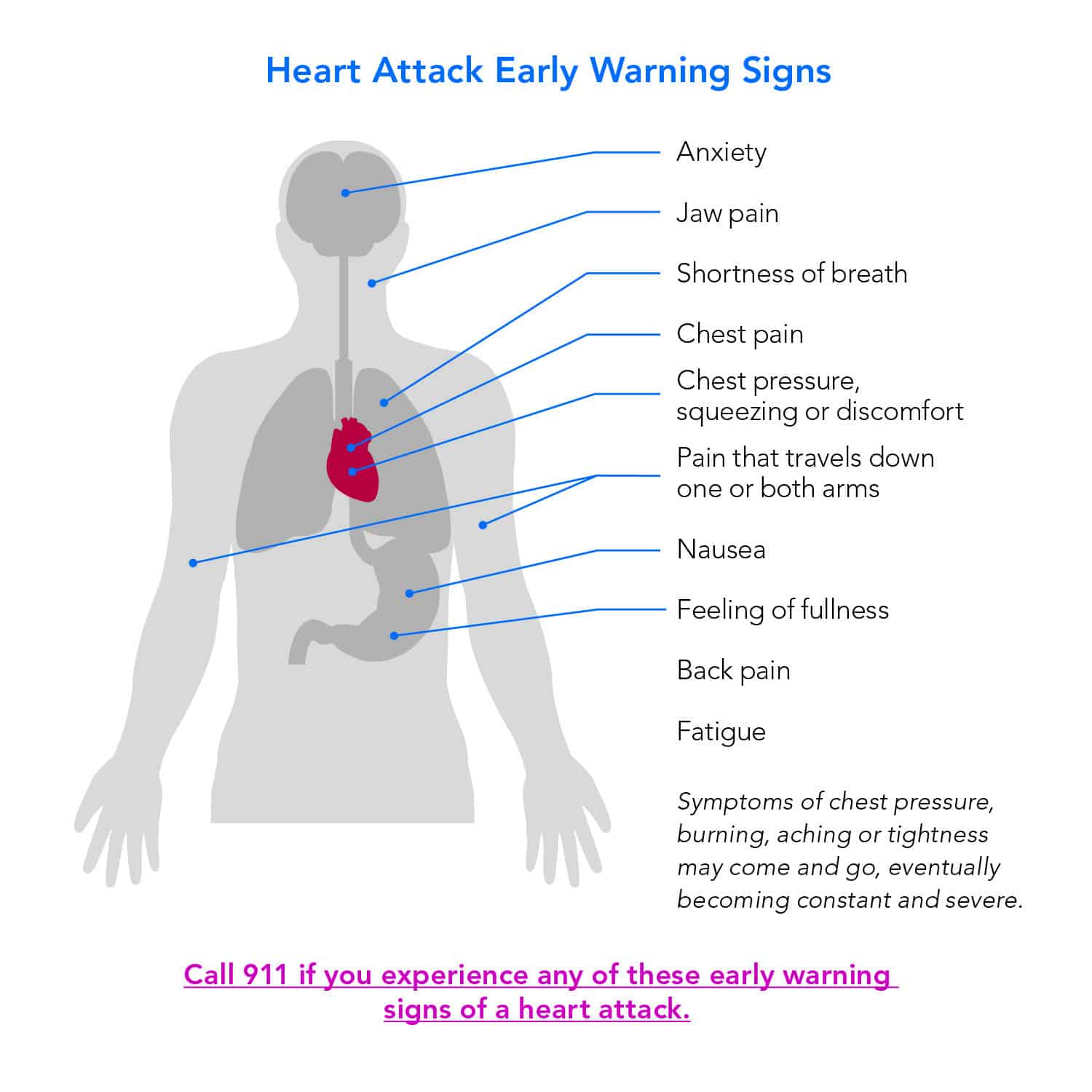
Medical professionals, including experts at the American Heart Association (AHA), often prefer the word "discomfort" over "pain." Why? Because patients frequently describe the sensation as pressure, squeezing, fullness, or a heavy weight sitting on their sternum. Imagine an elephant standing on your chest, or a belt being tightened around your ribcage. That is a classic presentation, but even that can be subtle.
You might feel it in the center of your chest. It might last for more than a few minutes, or—and this is the tricky part—it might go away and then come back. This "stuttering" pain is a huge red flag. If you feel fine one minute and then suddenly feel like your chest is in a vise ten minutes later, your body is trying to tell you that a coronary artery is struggling to stay open.
✨ Don't miss: High Protein in a Blood Test: What Most People Get Wrong
There’s also the "referred pain" factor. Your nerves are a complex highway system. Sometimes the brain gets confused about where a pain signal is coming from. This is why you might feel the ache in your jaw, your neck, or your back. Men often report pain radiating down the left arm, but don't ignore the right arm either. It can happen on both sides. If you have unexplained pain in your upper body that seems to coincide with a general feeling of unease, you need to take it seriously.
The gender gap in symptoms is real
Women are significantly more likely than men to experience "atypical" symptoms. This is a medical fact that has led to countless misdiagnoses over the decades. While chest pressure is still the most common symptom for everyone, women often report extreme fatigue that comes out of nowhere. We’re talking about the kind of exhaustion where you feel like you can't lift your arms to brush your hair.
- Nausea or vomiting that feels like food poisoning.
- Lightheadedness or a sudden dizzy spell.
- Shortness of breath without any physical exertion.
- Pain in the lower chest or upper abdomen.
Dr. Nieca Goldberg, a cardiologist and spokesperson for the AHA, has frequently noted that women might describe their heart attack as feeling like "pressure in the upper back" or even just "flu-like symptoms." If you’re a woman and you feel like you’ve been hit by a truck but your chest doesn't necessarily feel like it's exploding, don't dismiss it. The "silent" heart attack is much more common than people realize, particularly in those with diabetes or the elderly, where nerve damage (neuropathy) can actually blunt the sensation of pain entirely.
What's actually happening inside the artery?
To understand how to tell if you are have a heart attack, it helps to know what’s going on under the hood. Most heart attacks occur because of coronary artery disease. Over years, plaque—a sticky mix of fat, cholesterol, and other gunk—builds up on the inner walls of your arteries. This is atherosclerosis.
Usually, the heart attack doesn't happen because the artery "clogs up" slowly like a drain. Instead, a piece of that brittle plaque cracks or ruptures. Your body sees that rupture as an injury and sends platelets to "fix" it by forming a clot. That clot is the killer. It can block the blood flow instantly.
Once the blood stops flowing, the heart muscle cells downstream start to starve. They need oxygen. Without it, they begin to die within minutes. This is why cardiologists say "time is muscle." The longer you wait to get to an ER, the more permanent the damage to your heart's pumping chamber. If you get treated within the "golden hour," the chances of recovering with minimal damage are exponentially higher.
🔗 Read more: How to take out IUD: What your doctor might not tell you about the process
The "Sense of Impending Doom"
This sounds like something out of a gothic novel, but it is a genuine clinical symptom. Many patients who have survived a myocardial infarction (the medical term for a heart attack) report a sudden, overwhelming feeling that something is "very wrong" or that they are about to die.
It isn't just anxiety.
It's a physiological response to a systemic crisis. Your autonomic nervous system is firing on all cylinders. You might break out in a "cold sweat"—that clammy, drenching perspiration that has nothing to do with the room temperature. This is often accompanied by skin that looks pale or ashen. If you look in the mirror and you see a ghost staring back at you, and you’re sweating through your shirt while sitting still, call 911.
Differentiating from Panic Attacks and Heartburn
This is where it gets messy. A panic attack can feel almost identical to a heart attack. Both cause chest tightness, sweating, and a feeling of doom. However, a panic attack often peaks within about 10 minutes and then begins to subside. A heart attack usually persists or worsens.
Heartburn (GERD) is another common masquerader. Generally, heartburn is a burning sensation that moves upward from the stomach to the throat and is often triggered by lying down or eating. But here is the golden rule used by ER doctors: You cannot reliably tell the difference yourself. Even doctors need an EKG (electrocardiogram) and blood tests (looking for a protein called troponin) to be 100% sure.
Never try to "wait out" the pain to see if an antacid works. If you take a Tums and the pain doesn't vanish instantly, or if you have other symptoms like sweatiness or shortness of breath, the antacid test is a failure. Move. Fast.
💡 You might also like: How Much Sugar Are in Apples: What Most People Get Wrong
Immediate Actionable Steps
If you suspect you or someone near you is having a heart attack, the sequence of events matters immensely. Do not drive yourself to the hospital. If you black out behind the wheel, you’re a danger to yourself and everyone else on the road.
- Call 911 immediately. Paramedics can start treatment the second they arrive. They carry EKGs and can transmit the data to the hospital while in transit, so the cath lab is ready for you the moment the ambulance doors open.
- Chew an aspirin. Unless you are allergic or have been told by a doctor never to take it, chew a full-strength (325mg) aspirin or four baby aspirins. Chewing it gets it into your bloodstream faster than swallowing it whole. Aspirin helps thin the blood and can prevent the clot from getting larger.
- Sit down and stay calm. Stop all physical activity. Heart muscle under stress needs as little demand as possible.
- Unlock your front door. If you are alone, make sure the paramedics can get in without breaking the door down if you happen to lose consciousness before they arrive.
Risk Factors you can't ignore
While anyone can have a heart attack, certain factors mean you should have a much lower "trigger finger" for calling for help. If you have high blood pressure, high cholesterol, or a history of smoking, your risk is elevated. Diabetes is a massive one because, as mentioned, it can mask the pain.
Don't ignore family history. If your father or brother had a heart attack before age 55, or your mother or sister before 65, your genetic baseline is different. You might be fit, you might run marathons, but genetics can still play a hand in how your plaque is structured.
What happens at the hospital?
Once you arrive, the medical team will move fast. They’ll likely do a 12-lead EKG to look at the electrical activity of your heart. They are looking for specific patterns, like "ST-segment elevation," which indicates a major blockage.
They will also draw blood to check for Troponin. This protein is only released into the bloodstream when the heart muscle is damaged. If your Troponin levels are rising, it’s a confirmed heart attack. From there, you might go to the cardiac catheterization lab, where a doctor threads a thin tube through an artery in your wrist or groin up to your heart. They can inject dye to see the blockage and then use a tiny balloon to open it, often placing a metal mesh tube called a stent to keep it open.
It sounds intense, and it is, but it's routine for modern cardiac teams. The technology we have in 2026 is lightyears ahead of what was available even a decade ago.
Taking control of the aftermath
If you've identified the symptoms and gotten help, the journey doesn't end at the hospital exit. Survival is step one. Step two is preventing the next one.
- Cardiac Rehab: This is a supervised exercise and education program. It’s one of the most underutilized tools in recovery. People who attend cardiac rehab have significantly lower rates of a second heart attack.
- Medication Adherence: You’ll likely be put on statins, beta-blockers, or anti-platelet drugs like Plavix. These aren't "suggestions." They are the scaffolding that keeps your cardiovascular system from collapsing again.
- Dietary Shifts: It’s not about never eating a burger again. It’s about the Mediterranean approach—plenty of olive oil, nuts, fish, and greens.
Identifying how to tell if you are have a heart attack is ultimately about intuition and caution. If the feeling is "new," "different," or "scary," treat it as a medical emergency. It is far better to be sent home from the ER with a diagnosis of indigestion than to stay home with a heart attack and suffer permanent, life-altering damage. Trust your gut, even if your chest isn't screaming.