You probably think lead poisoning is a relic of the Victorian era or something that only happens in extreme industrial accidents. It’s not. Honestly, lead is a "stealth" toxin. It doesn't usually announce itself with a fever or a bright red rash. Instead, it just sort of sits there, accumulating in your bones and teeth, mimicking other problems until things get serious.
The scary part? Most people who have it don’t look or feel "poisoned." Not at first.
If you’re wondering how to know if you have lead poisoning, you have to stop looking for a single "smoking gun" symptom. Lead is a systemic neurotoxin. It messes with your brain, your kidneys, and your blood. Because the symptoms are so vague—like fatigue or a bit of irritability—doctors often misdiagnose it as stress, anemia, or just "getting older." But if you live in a house built before 1978 or work in certain trades, that nagging brain fog might be more than just a lack of sleep.
The subtle ways lead shows up in adults
Adults usually get exposed through work or home renovations. It’s rarely one big dose. It’s a slow drip. You inhale some dust while sanding an old window frame. You drink water from a pipe joined with lead solder. Over time, the body mistakes lead for calcium. It stores it.
One of the first things people notice is a change in mood. You might feel "snappy" or unusually anxious. Mayo Clinic experts note that high lead levels in adults often manifest as high blood pressure and joint pain. It’s a dull ache. It’s that feeling of being "off" that you can't quite put your finger on.
But then there are the physical markers.
Abdominal pain is a big one. It’s often called "lead colic." This isn't your typical stomach flu; it's a deep, cramping pain that doesn't go away with an antacid. Some people also develop a "lead line"—a bluish-black line along the gums where they meet the teeth. It’s rare now, but it’s a classic sign of heavy exposure.
If your hands or feet start feeling tingly or weak, pay attention. Lead loves to attack the peripheral nerves. This can lead to something called "wrist drop," where you literally can't lift your hand at the wrist. That’s an extreme case, obviously, but the tingling (paresthesia) is a more common early warning.
✨ Don't miss: 2025 Radioactive Shrimp Recall: What Really Happened With Your Frozen Seafood
Why kids are the "canaries in the coal mine"
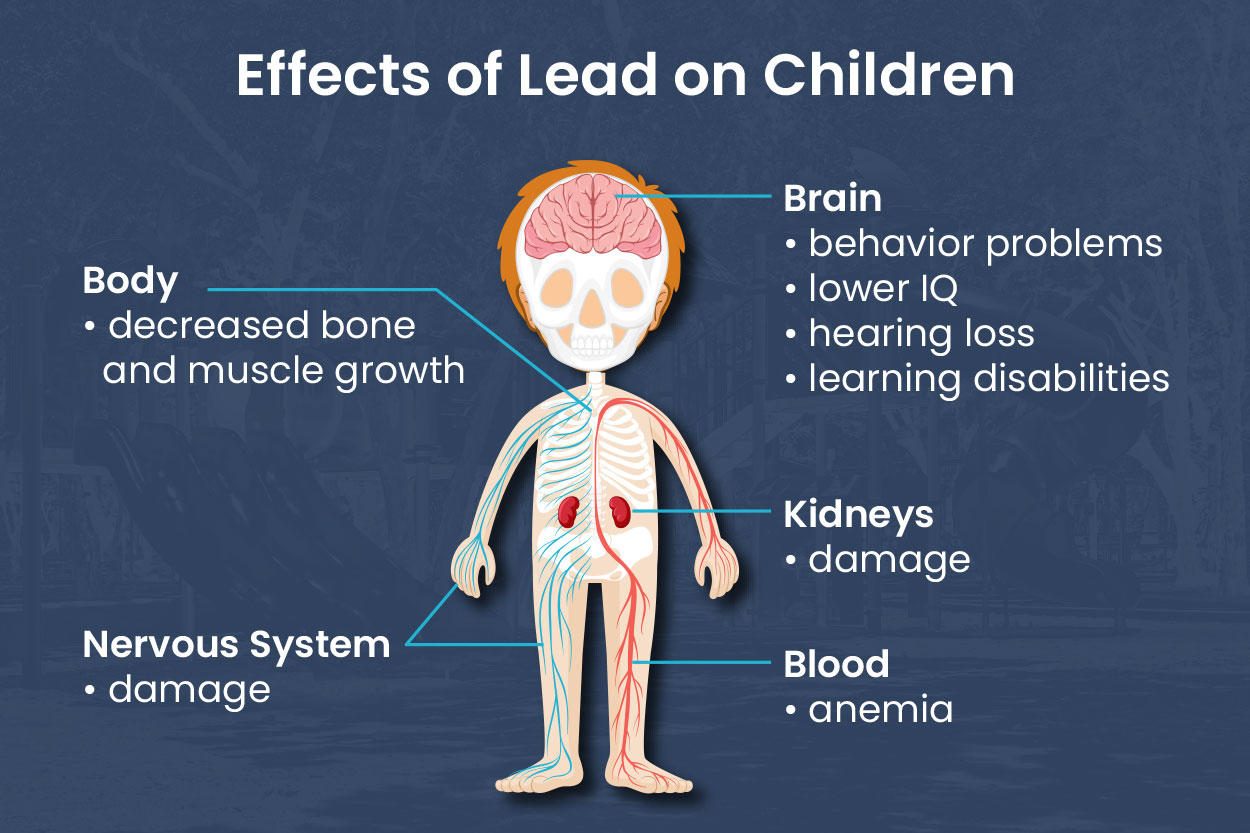
For children, the stakes are different. Their brains are still building connections. Even tiny amounts of lead can act like a monkey wrench in the machinery.
How do you know if a child has lead poisoning? You usually don't—not by looking at them.
The CDC recently lowered the blood lead reference value to 3.5 micrograms per deciliter, recognizing that no level of lead is safe for a child. Kids don't usually get the "colic" adults do. Instead, they lose milestones. A child who was speaking well might start struggling with words. They might become hyperactive or lose their appetite.
Research from the Environmental Protection Agency (EPA) highlights that lead exposure in childhood is linked to lower IQ scores and behavioral issues like ADHD. It’s frustrating because these symptoms overlap with so many other developmental hurdles. If a child is suddenly falling behind in school or seems perpetually lethargic, it’s worth asking when the house was last painted.
Common sources you might be overlooking
It’s not just paint chips. We’ve known about paint since the 70s. The real culprits today are often more obscure:
- Soil: Lead from old gasoline and exterior paint settles in the dirt. Kids play in it, then put their hands in their mouths.
- Glazed Pottery: That beautiful handcrafted bowl you bought on vacation? If it wasn't fired at a high enough temperature, the lead in the glaze can leach into your soup.
- Traditional Medicines: Some folk remedies like Greta or Azarcon (used for upset stomachs) contain high amounts of lead.
- Water: Even if the city water is clean, the "service line" connecting the main to your house might be lead.
- Hobbies: Stained glass work, target shooting (lead bullets), and fishing (lead weights) are huge contributors to adult exposure.
The only way to be sure: Testing
You cannot diagnose lead poisoning with a DIY kit from the hardware store. Those kits are for testing your walls, not your blood.
If you suspect exposure, you need a blood lead level (BLL) test. It’s a simple blood draw.
🔗 Read more: Barras de proteina sin azucar: Lo que las etiquetas no te dicen y cómo elegirlas de verdad
Physicians usually order a venous sample (from the arm) because it’s more accurate than a finger prick. A finger prick can sometimes give a "false positive" if there’s lead dust on the skin. If the test comes back elevated, the next step is figuring out where it's coming from.
Understanding the numbers
The results can be confusing.
For adults, a level under 5 µg/dL is considered "normal" for the general population, though OSHA (the Occupational Safety and Health Administration) has different, often criticized, standards for workers. If you're hitting 20 or 30 µg/dL, you're in the danger zone for long-term health issues. Once you hit 60 or 80 µg/dL, you’re looking at immediate medical intervention, possibly chelation therapy.
Chelation is a process where you take a medication that binds to the lead in your blood so you can pee it out. It sounds like a "quick fix," but it’s actually pretty hard on the body and is only used in severe cases. It doesn't "undo" the damage already done to the brain or kidneys; it just stops more damage from happening.
What to do if you suspect lead in your home
Don't panic and start scraping paint. That is the worst thing you can do.
Sanding or scraping lead paint creates fine dust that stays in the air for days. It's much easier to inhale dust than it is to eat a paint chip. If you think your home has lead, the first step is "lead-safe" cleaning. Use a wet mop and a HEPA-filter vacuum. Keep the dust down.
You can hire a certified lead inspector. They use an XRF (X-ray fluorescence) machine that can see through layers of new paint to find the lead underneath. It’s non-destructive and tells you exactly which walls are the problem.
💡 You might also like: Cleveland clinic abu dhabi photos: Why This Hospital Looks More Like a Museum
Nutrition also plays a weirdly important role.
The body absorbs lead more easily when you’re low on calcium, iron, and vitamin C. If your diet is solid, your body is slightly better at "rejecting" lead absorption. It’s not a shield, but it’s a layer of defense.
Actionable steps to take right now
If the symptoms resonate or you live in an old building, stop guessing.
First, call your doctor and specifically ask for a "blood lead level test." Don't just ask for "blood work"—lead isn't usually included in a standard CBC (Complete Blood Count).
Second, test your water. Many local utility companies offer free lead testing kits. You fill a bottle with the "first draw" of water in the morning and mail it back. If lead is present, you can often solve the problem with a high-quality water filter certified to NSF/ANSI Standard 53 for lead removal.
Third, evaluate your shoes. It sounds silly, but we track a massive amount of lead-contaminated soil into our homes. Implementing a "no-shoes" policy is one of the cheapest and most effective ways to lower lead dust levels in your living space.
Finally, if you work in construction, auto repair, or at a firing range, never wear your work clothes home. Change at the site if possible, or head straight to the laundry. You don't want to bring that dust to your couch or your kids.
Lead is a persistent problem, but it’s a manageable one once you stop treating it like a ghost and start treating it like the heavy metal it is. Knowledge is the difference between a permanent neurological hit and a simple lifestyle adjustment. Get the test, check the pipes, and keep the dust at bay.
Next Steps for Safety:
Check the EPA's "Lead-Safe" certified firm registry before hiring any contractors for home repairs. If you are pregnant or have young children, prioritize a venous blood test immediately if you reside in a pre-1978 home or have noticed any persistent developmental or neurological shifts. Ensure your household diet is rich in iron and calcium to provide a biological buffer against incidental lead absorption.