You just took a nasty spill. Maybe it was a slip on a patch of ice, a collision during a pickup basketball game, or a literal run-in with an open cabinet door. Your head throbs. You’re seeing stars. Naturally, the first thing you wonder is whether you’ve just got a nasty bump or if something is actually broken inside. Understanding how to know if you have a skull fracture isn't always as straightforward as looking for a crack in a bone like you would with an arm or a leg.
Bones in the skull are tough. They’re designed to be a helmet for your brain, but they aren't invincible. Sometimes the skin doesn't even break, yet the bone underneath has given way. It’s scary because the skull isn't just one solid piece of rock; it's a complex puzzle of plates held together by sutures. When that puzzle gets disrupted, the stakes are incredibly high.
Honestly, the most dangerous thing about a skull fracture isn't always the bone itself. It’s what that broken bone might be doing to the gray matter underneath. You could be walking and talking one minute and in a life-threatening crisis the next.
The immediate red flags that demand an ER visit
Let’s get real. If you see clear fluid leaking from the nose or ears, stop reading this and call 911. That fluid is likely cerebrospinal fluid (CSF). It’s the stuff that cushions your brain. If it’s leaking out, it means the protective layers around your brain have been breached. This is a hallmark sign of a basilar skull fracture, which happens at the base of the cranium.
You might also notice something called "Battle’s sign." This is bruising that shows up behind the ear, over the mastoid process. It doesn't usually pop up the second you hit your head; it might take a few hours or even a day to darken. Similarly, "raccoon eyes"—bruising around both eyes without a direct hit to the face—is a massive indicator that the front of the skull base is compromised.
Pain is a given, but is it localized? If you can point to one specific spot where the pain is agonizing and feels "sharp" rather than a dull ache, that’s a clue. Sometimes you can actually feel a depression or a "soft spot" where the bone has been pushed inward. This is what doctors call a depressed skull fracture. It’s basically the "dent in the car door" of head injuries.
💡 You might also like: Can DayQuil Be Taken At Night: What Happens If You Skip NyQuil
Why a "clear" CT scan isn't always the end of the story
Doctors like Dr. Uzma Samadani, a prominent neurosurgeon, often emphasize that the brain injury is what matters most. You can have a fracture without a major brain bleed, and you can have a fatal brain bleed without a fracture. However, when you’re trying to figure out how to know if you have a skull fracture, you’re often looking at the mechanism of injury.
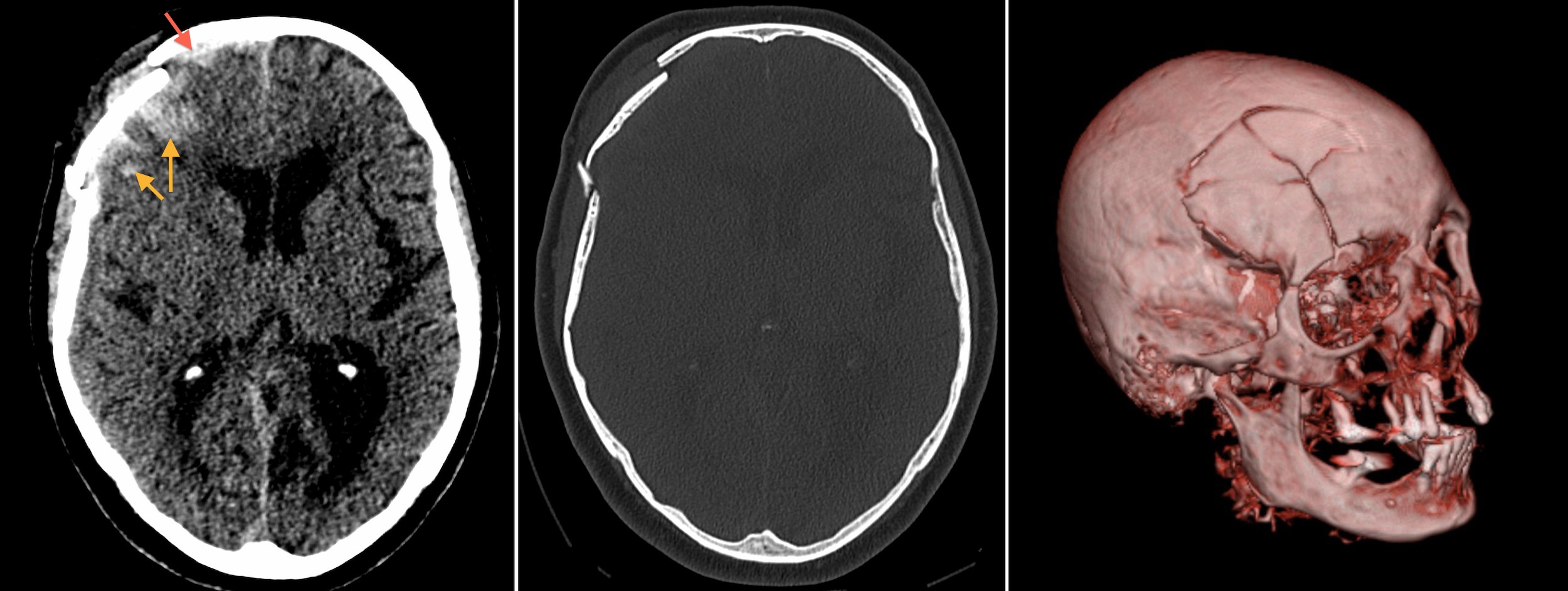
Was it a high-velocity impact? A fall from a height greater than five feet? These increase the statistical likelihood of a break. In a hospital setting, they’ll likely use a non-contrast CT scan. It’s the gold standard. X-rays are kinda old school for this; they miss a lot of the fine lines that a CT picks up easily.
But here is the kicker: some linear fractures—which are basically just cracks—don't actually require surgery. They just need time. The body knits the bone back together. The real concern for the medical team is whether the bone fragments are pressing into the brain tissue or if a jagged edge has nicked an artery.
Different types of breaks you should know about
Not all fractures are created equal.
- Linear fractures: These are the most common. It’s a break in the bone, but the bone doesn't move. You might just think you have a bad headache. These often heal on their own, but they still require a professional eye to ensure no underlying hematoma is forming.
- Depressed fractures: This is the scary one. Part of the skull is sunken in toward the brain. If the "dent" is deeper than the thickness of the skull bone itself, surgeons usually have to go in and lift it back out to relieve pressure.
- Diastatic fractures: These happen along the suture lines—the places where the skull bones fused together during childhood. These are more common in infants and young children whose skulls haven't fully hardened yet.
- Basilar fractures: As mentioned, these occur at the base. They are tricky because you can't see them from the outside, and they often involve tears in the membranes surrounding the brain.
The "Talk and Die" Syndrome
It sounds like a horror movie title, but it’s a clinical reality. Epidural hematomas often follow a skull fracture, particularly if the break crosses the path of the middle meningeal artery.
📖 Related: Nuts Are Keto Friendly (Usually), But These 3 Mistakes Will Kick You Out Of Ketosis
The person gets hit. They might be unconscious for a second, but then they wake up. They feel "fine." They might even apologize for making a scene. This is the "lucid interval." Then, as the blood builds up inside the rigid container of the skull, pressure skyrockets. Within an hour or two, they lose consciousness again and can quickly slip into a coma.
If you or someone else hits their head hard enough to wonder how to know if you have a skull fracture, the worst thing you can do is go to sleep immediately without someone monitoring you. You need to check for pupil dilation. Are the pupils the same size? Do they shrink when you shine a light in them? If one is "blown" (huge and unresponsive), that is a neurosurgical emergency.
What about the "Goose Egg"?
We’ve all seen it. A kid bumps their head and a massive, terrifying lump grows within minutes. Paradoxically, a big external bump is often a good sign. It means the bleeding is happening outside the skull, under the scalp. The blood has somewhere to go.
It’s the injuries where there is no external swelling—but the person is acting "off"—that keep ER doctors up at night. Watch for behavioral changes. Is the person suddenly irritable? Are they slurring their words? Do they seem confused about where they are? If you ask them who the President is and they give you a name from 1994, things are bad.
Long-term symptoms to watch for
Maybe you didn't go to the hospital. Maybe you thought you'd just "tough it out." But now, three days later, you feel like garbage. Chronic headaches that don't respond to Tylenol or Advil are a major red flag.
👉 See also: That Time a Doctor With Measles Treating Kids Sparked a Massive Health Crisis
You might also experience:
- Tinnitus: A persistent ringing in the ears.
- Anosmia: Losing your sense of smell. This happens often with frontal fractures because the tiny nerves that control smell get sheared off.
- Vision changes: Blurred vision or double vision that doesn't go away.
- Nausea: Not just a "sour stomach," but projectile vomiting without any warning.
These symptoms suggest that the initial impact caused more than just a surface bruise. Even if the bone isn't shattered, the brain may have suffered a contusion (a bruise on the brain itself) or a concussion.
Immediate steps to take right now
If you suspect a fracture, do not apply direct pressure to the wound if you can feel the bone shifting. You don't want to push bone fragments deeper. Instead, wrap the head loosely with clean gauze to control bleeding. Keep the person's head and shoulders slightly elevated. This helps reduce the intracranial pressure.
Avoid taking aspirin. Most people reach for it for pain, but aspirin thins the blood. If there is a bleed inside the skull, aspirin will make it significantly worse. Stick to acetaminophen if you absolutely must take something, but honestly, if you’re in enough pain to need meds, you should be in a triage room.
Actionable Next Steps
- The Two-Hour Rule: If the person lost consciousness for even five seconds, they need a medical evaluation. No exceptions.
- Check the "Leak": Use a white tissue to dab any fluid from the nose or ears. If the fluid creates a clear ring around a central spot of blood (the "halo sign"), it is almost certainly CSF. This is a medical emergency.
- Monitor for 24 Hours: If you stay home, have someone wake you up every 2 to 3 hours. They should ask you a basic question to ensure you are coherent.
- Limit Stimulation: No screens, no loud music, and no bright lights. Even if it's "just" a concussion, your brain needs a metabolic "timeout" to heal.
- Document the Impact: If possible, remember what hit you. A flat surface (the floor) usually causes a linear fracture. A sharp object (the corner of a table) is more likely to cause a depressed fracture. This info helps the doctor tremendously.
Head injuries are deceptive. You can't see the damage, and the brain doesn't have pain receptors—the pain you feel comes from the scalp, the bone, and the membranes. When you're trying to figure out how to know if you have a skull fracture, err on the side of "overreacting." A missed fracture can lead to meningitis, permanent brain damage, or worse. Getting a scan might feel like a hassle, but it’s the only way to be 100% sure.