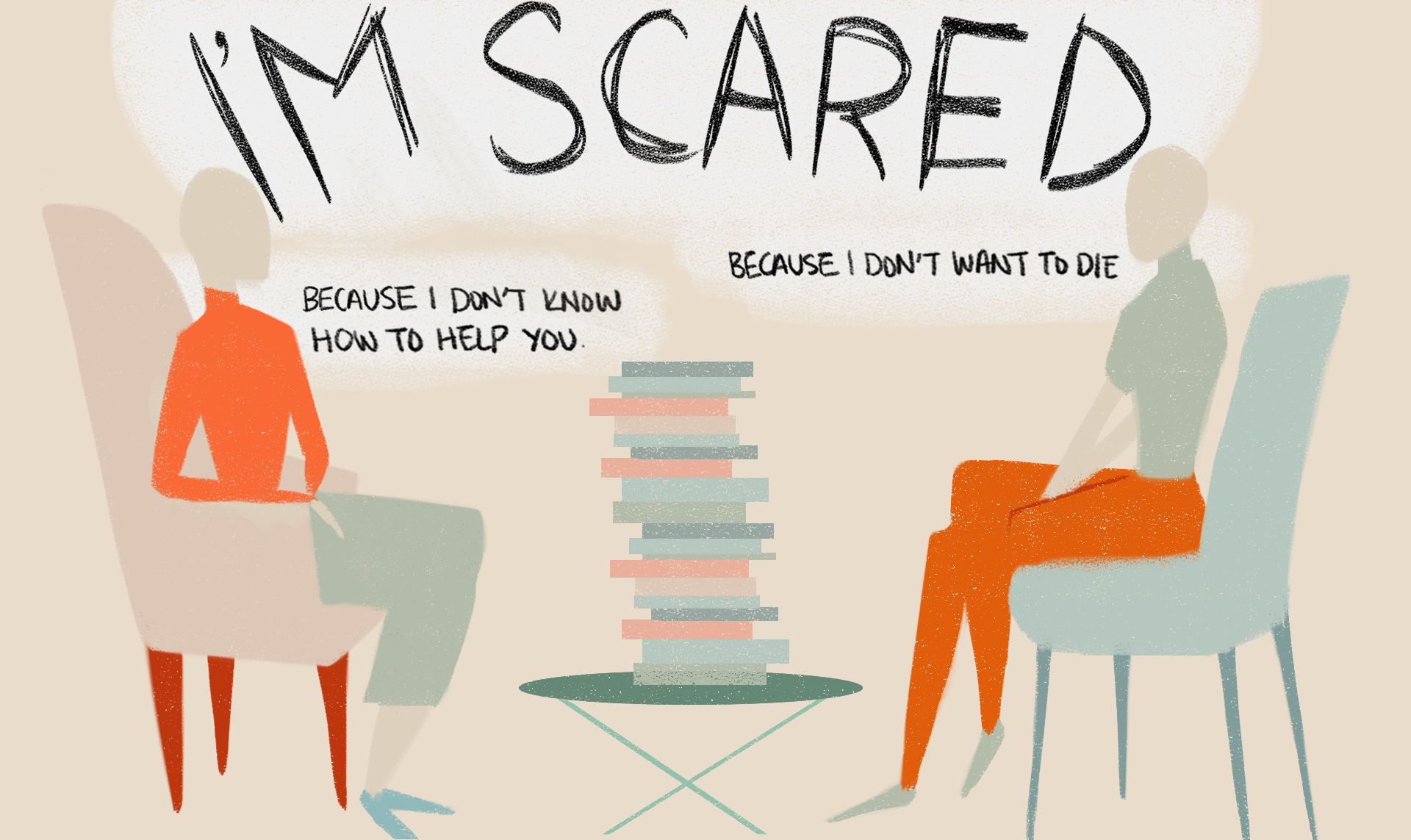
You're here because you're scared. Someone you care about—a friend, a brother, maybe a coworker—has said something that made your stomach drop. Or maybe they haven't said anything at all, but their silence feels heavy, like a physical weight in the room. You want to know how to help someone that is suicidal, but the internet is full of sterile, clinical advice that feels like reading a microwave manual.
It's terrifying.
The first thing you need to accept is that you aren't a magician. You can’t "fix" their brain chemistry or undo their trauma with a perfectly timed hug. But you can be a bridge. Most people who are struggling don't actually want to die; they just want the pain to stop. It’s a subtle but massive distinction. When you understand that, your role shifts from "lifeguard" to "anchor."
The Fear of "The Question"
Most of us were raised to believe that if you ask someone if they’re thinking about suicide, you’ll plant the idea in their head. That is a total myth. Experts like Dr. Thomas Joiner, who has spent decades studying the psychology of suicide, have found the opposite to be true. Asking the question directly—"Are you thinking about killing yourself?"—usually brings a sense of immense relief. It’s like popping a blister. The pressure finally has somewhere to go.
Don’t use metaphors. Don't ask if they’re "thinking of doing something silly" or "hurting themselves." Self-harm and suicide are different things. Be blunt. Be kind.
"I’ve noticed you’ve been saying some things that worry me. Are you thinking about ending your life?"
Saying the word "suicide" out loud shows them that you are strong enough to hear the answer. If you can’t say it, why should they feel safe enough to tell you?
Recognizing the "Quiet" Red Flags
We all know the classic signs. Giving away prized possessions. Writing a will. Saying goodbye. But the real indicators are often way more subtle and, honestly, kinda confusing.
🔗 Read more: Exercises to Get Big Boobs: What Actually Works and the Anatomy Most People Ignore
Take the "sudden calm" phenomenon. Sometimes, a person who has been deeply depressed for months suddenly seems... fine. They’re light, they’re making jokes, they’re finally sleeping. This can be the most dangerous moment. Why? Because they might have finally made the decision to go through with it. The struggle of deciding is over, and that brings a temporary, eerie peace.
Other signs are more chaotic:
- Increased alcohol or drug use (basically self-medicating the despair).
- Extreme irritability. They aren't sad; they're pissed off at everything.
- Sleeping all the time or not at all.
- Talking about being a "burden." This is huge. If someone says, "You’d be better off without me," they aren't fishing for compliments. They genuinely believe their existence is a net negative for the world.
The Power of "Wait"
In the mental health world, we talk about "means restriction." It sounds technical, but it’s basically about slowing things down. Suicidal crises are often surprisingly short-lived. If you can help someone get through the next ten minutes, the next hour, or the next night, the intensity of the urge often peaks and then ebbs.
If they have a firearm, get it out of the house. If they have a stash of pills, give them to a trusted third party. You aren't being "intrusive." You’re creating a gap between an impulse and an action.
Listening Without Trying to Win the Argument
When someone tells you they want to die, your instinct is to argue.
"But you have so much to live for!"
"Think about your kids!"
"It gets better, I promise!"
Stop. Just stop. When you do that, you’re essentially telling them their feelings are wrong. You’re trying to logic them out of an emotional state. It doesn't work. In fact, it often makes them feel more lonely because it proves you don’t understand how much they’re hurting.
Instead of arguing, validate.
💡 You might also like: Products With Red 40: What Most People Get Wrong
"That sounds incredibly heavy."
"I can't imagine how exhausted you must be."
"I'm so glad you told me."
You don't have to agree that life is hopeless. You just have to acknowledge that to them, right now, it feels that way. Listening is a profound act of service. Sometimes, just having one person sit in the dark with them is enough to keep them here.
Navigation: Who Do You Actually Call?
Knowing how to help someone that is suicidal means knowing the professional landscape. You are the first responder, but you aren't the hospital.
If there is an immediate threat—like they have a weapon in their hand or have already taken something—call emergency services or go to the nearest ER. If you're in the US or Canada, 988 is the go-to number for the Suicide & Crisis Lifeline. You can call it, or they can. You can even text it. It’s staffed 24/7 by people who actually know how to de-escalate these specific moments.
But let’s talk about the "middle ground." What if they aren't in immediate danger but they’re sliding down the mountain?
- Mobile Crisis Units: Many cities have these. They are teams of mental health professionals who come to the house so you don't have to involve the police, which can sometimes escalate stress.
- Safety Planning: This isn't a "contract" (those don't really work). It's a list. What are their triggers? What are their coping distractions (Netflix, walking the dog, playing Elden Ring)? Who are three people they can call?
- The "Warm Line": Unlike a hotline, a warm line is for people who just need to talk before it becomes a crisis. It’s a great preventative tool.
The Burden on You
Let’s be real for a second. This is traumatizing for you, too.
You cannot be someone’s only reason for living. That is an impossible, crushing weight that will eventually break you both. You have to involve other people. Whether it’s their family, a therapist, or a support group, you need a team.
📖 Related: Why Sometimes You Just Need a Hug: The Real Science of Physical Touch
There is a concept in psychology called "vicarious trauma." You might start feeling their symptoms. You might stop sleeping. You might feel guilty every time you're happy. Watch out for that. You are no use to them if you’re drowning right next to them.
Actionable Steps for Right Now
If you are sitting with someone right now, or you’re about to go see them, here is the protocol. Forget the fancy theories. Do this:
- Remove the means. Check for meds, blades, or weapons. If you can't remove them, move the person to a "safe" environment like your house or a coffee shop.
- The 988 Option. If the conversation gets too heavy for you to handle, call 988 together. Put it on speaker. Let the professional guide the talk.
- Don't leave them alone. If they are in an active crisis, stay. If you have to leave, make sure someone else takes your "shift."
- Follow up. The day after a big "talk" is often the loneliest. Send a text. "Hey, thinking of you. No need to reply, just wanted you to know I'm here."
- Help with the "life stuff." Depression makes laundry feel like climbing Everest. Don't ask "how can I help?" Just do something. Bring a meal. Fold the towels. Take the trash out. Reducing the "noise" of life gives them more energy to focus on staying alive.
Suicide is complex. It's often the result of "thwarted belongingness" and "perceived burdensomeness," terms coined by researchers to describe that lethal mix of feeling alone and feeling like a pain to others. By showing up, you tackle both. You prove they belong, and you prove they aren't a burden you can't handle.
The goal isn't to make them happy today. The goal is just to get to tomorrow. And then the tomorrow after that. One day at a time, until the fog starts to lift, even if just a little bit.
Immediate Resources:
- Crisis Text Line: Text HOME to 741741.
- The Trevor Project (for LGBTQ+ youth): Call 1-866-488-7386 or text START to 678-678.
- Veterans Crisis Line: Dial 988 then press 1.
Next Steps for You:
Enroll in a QPR (Question, Persuade, Refer) gatekeeper training session. It’s a short, often free course that functions like CPR for mental health. It gives you a scripted, proven way to handle these conversations so you don't have to rely on "gut instinct" when the stakes are this high. You can also look into Mental Health First Aid (MHFA) certification, which provides a more in-depth framework for supporting people through various stages of mental health challenges. Finally, make sure you have your own therapist or support system to process the emotional toll of being a caregiver.