It happens at the worst times. Maybe you’re mid-meeting, or perhaps you're finally settling into bed after a long day, and suddenly, there it is—that sharp, stabbing pressure right under your ribs or deep in your abdomen. It’s paralyzing. You try to sit up straight, but it feels like there’s a literal balloon inflating inside your torso that shouldn't be there. Everyone has been there. Honestly, gas pain is one of those universal human experiences that we don't talk about enough because it’s "embarrassing," but when you're in the middle of a flare-up, you don't care about social norms. You just want to know how to help gas pain before you have to unbutton your pants in public.
Gas isn't just air. It’s a byproduct of your microbiome doing its job—or sometimes, doing it a little too enthusiastically. When your body breaks down carbohydrates in the large intestine, bacteria ferment that leftover fiber, starch, and sugar. The result? Hydrogen, methane, and carbon dioxide. Usually, this escapes naturally (we all do it, about 14 to 23 times a day, according to the Mayo Clinic). But when that gas gets trapped or moves too slowly through your digestive tract, the pressure builds. That’s when the "pain" part kicks in. It can even mimic a heart attack if the gas gets stuck in the upper curve of the colon near the chest. Scary, right? But usually, it’s just biology being loud.
Why your gut is acting like a chemistry experiment
Understanding the "why" is the first step toward the "how." You might think it’s just that spicy taco you had for lunch, but it’s often more complex. Swallowing air—aerophagia—is a massive culprit. You do this when you eat too fast, chew gum, or drink through a straw. It’s simple physics: what goes in must come out, and if it doesn't go out the top as a burp, it’s going on a long, uncomfortable journey through twenty-some feet of intestines.
Then there’s the food itself. We’ve all heard about beans, but cruciferous vegetables like broccoli, cabbage, and Brussels sprouts contain a complex sugar called raffinose. Humans lack the enzyme to break this down easily. So, it sits there. It ferments. Your bacteria have a party, and you pay the price in bloating. Some people also have genuine intolerances to lactose or fructose that they haven't quite pinned down yet. If you notice you're searching for how to help gas pain every time you have a latte or a big bowl of fruit, your body might be trying to tell you it lacks the specific tools to process those sugars.
The transit time trouble
Sometimes the issue isn't what you ate, but how fast things are moving. Constipation is a huge, often ignored factor in gas pain. If "the pipes" are backed up, the gas produced in your colon has nowhere to go. It gets trapped behind stool, stretching the intestinal walls and causing those sharp, cramping sensations. It’s a traffic jam. And just like a real traffic jam, the longer things sit there, the more frustrated (and gassy) the system becomes.
Moving the bubbles: Physical hacks for immediate relief
If you're hurting right now, you don't want a lecture on fiber. You want the pain gone. The fastest way to move trapped gas is often through gravity and movement. You have to physically help the bubbles navigate the twists and turns of your bowels.
🔗 Read more: X Ray on Hand: What Your Doctor is Actually Looking For
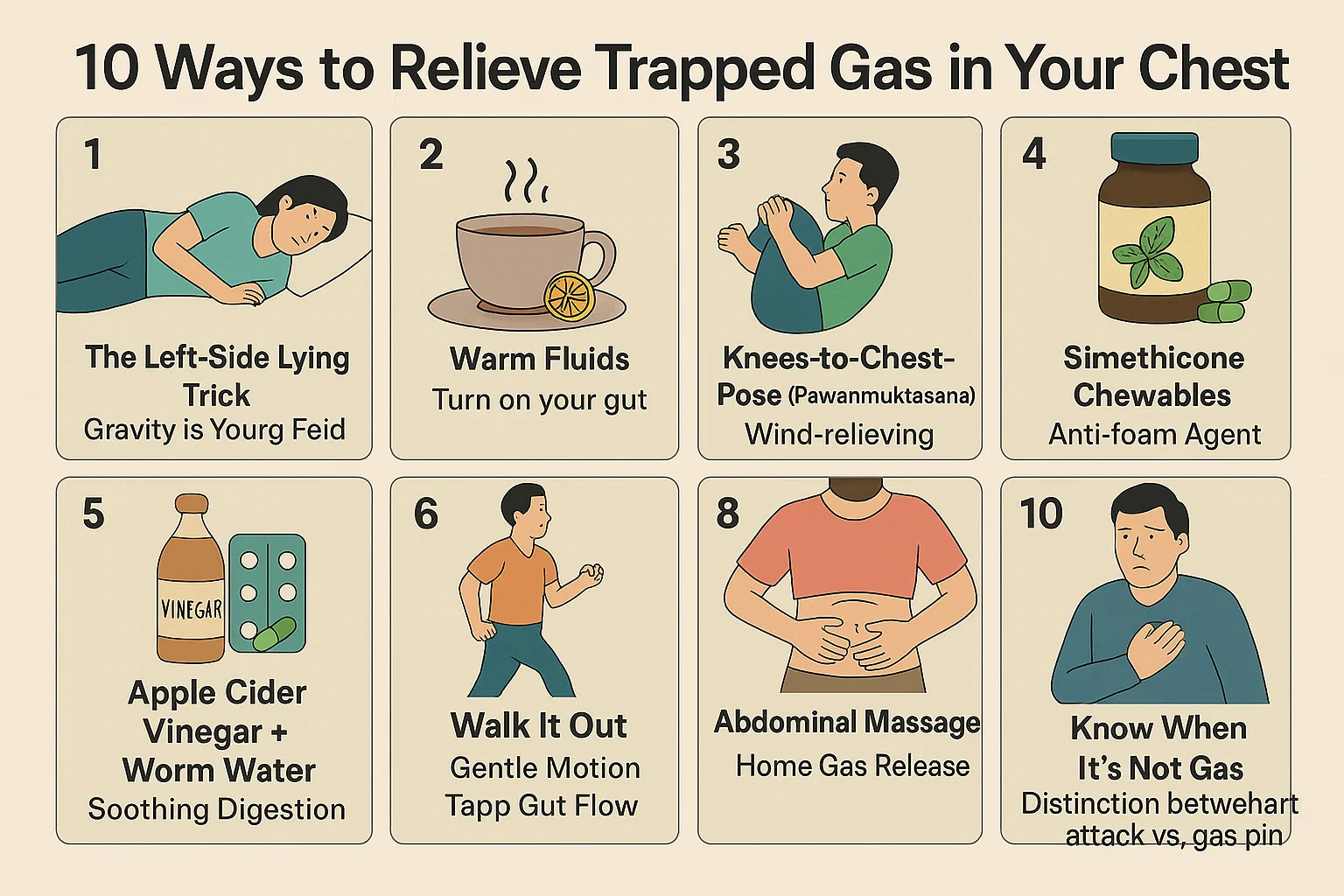
One of the most effective methods is the "Child’s Pose" from yoga. You kneel on the floor, sit back on your heels, and fold forward, resting your forehead on the ground. This position compresses the abdomen and helps relax the pelvic muscles, which can encourage gas to move toward the exit. Another one is the "Wind-Relieving Pose" (Pavanamuktasana)—the name literally tells you what it does. You lie on your back and pull your knees to your chest. It’s not glamorous. It’s not "aesthetic." But it works because it puts targeted pressure on the ascending and descending colon.
Walking it off
Don't just sit there. If you can manage it, get up and walk. Gentle movement stimulates peristalsis, which is the wave-like muscle contractions that move food and gas through your system. A ten-minute stroll around the block can do more for gas pain than almost any over-the-counter pill because it uses gravity to your advantage.
- Try a heating pad. Heat relaxes the muscles in the gut, which can stop the spasms that make gas feel so painful.
- Self-massage. Start at the lower right side of your belly, move up to the ribs, across to the left, and then down. This follows the path of the large intestine.
- Drink something warm. Peppermint tea is a classic for a reason; the menthol has an antispasmodic effect on the smooth muscle of the digestive tract.
What the science says about supplements and meds
When movement isn't enough, people usually reach for the medicine cabinet. There are a few heavy hitters here, but they work in very different ways. Simethicone (found in Gas-X or Mylanta) is the most common. It’s actually a "surfactant." Basically, it takes all those tiny, painful gas bubbles and merges them into bigger bubbles that are much easier to pass. It doesn't "delete" the gas; it just makes it more manageable.
Then you have digestive enzymes. If you know you're about to eat a bowl of lentil soup, taking something like Beano (which contains alpha-galactosidase) can prevent the gas from forming in the first place by helping you break down those tricky sugars. However, these are preventative. If you’re already in pain, Beano won’t do much. You’re already past that stage.
The probiotic debate
Probiotics are a bit of a gray area. While they can help rebalance a gut microbiome that’s producing too much gas, some people find that starting a new probiotic actually increases gas for the first week or two. Your gut is an ecosystem. When you drop a bunch of new "good" bacteria into it, there’s going to be some initial tension. If you're looking for how to help gas pain in the long term, a specific strain like Bifidobacterium infantis has shown some promise in clinical trials for reducing bloating in IBS patients.
💡 You might also like: Does Ginger Ale Help With Upset Stomach? Why Your Soda Habit Might Be Making Things Worse
When gas pain isn't just gas
We need to be honest: sometimes that "gas" isn't gas. It’s important to know the "red flags" because self-treating a more serious condition can be dangerous. If your gas pain is accompanied by a fever, persistent vomiting, bloody stools, or unintended weight loss, stop googling and call a doctor.
Appendicitis often starts as a vague pain around the belly button that feels like it could be gas before it migrates to the lower right side. Gallstones can cause intense pressure in the upper right abdomen that people often mistake for indigestion. Even ovarian cysts or endometriosis can mimic the feeling of trapped gas in the lower pelvis. If you’ve tried moving, heat, and simethicone and the pain is still 10/10 after a few hours, it's time for a professional opinion.
The stress connection
Your brain and your gut are constantly talking. It's called the gut-brain axis. When you're stressed, your body's "fight or flight" system kicks in, which slows down digestion. Food sits longer. It ferments more. Also, stressed people tend to gulp air or have "nervous stomachs." If you're chronically gassy, your life stress might be just as much of a factor as your diet.
Building a "low-gas" lifestyle without being boring
You don't have to live on white rice and water to avoid pain. It’s more about strategy. For example, if you love beans, soak them overnight and rinse them thoroughly; this washes away some of the fermentable sugars. If you love salads, try steaming your kale or spinach slightly instead of eating it raw—it pre-breaks down some of the fibers your stomach struggles with.
Drinking water is non-negotiable. It keeps things moving. If you’re dehydrated, your colon will pull water from your waste, making it hard and causing that "traffic jam" we talked about earlier. Aim for consistency over perfection.
📖 Related: Horizon Treadmill 7.0 AT: What Most People Get Wrong
Practical steps for long-term relief:
- Eat smaller meals. Massive plates of food overwhelm your enzymes. Breaking it up into 4-5 smaller sittings gives your gut a fighting chance to keep up.
- Slow down. Try to chew each bite 20 times. It sounds tedious, but it prevents you from swallowing air and starts the chemical breakdown of food in your mouth.
- Identify triggers. Keep a simple note on your phone for three days. What did you eat, and how did you feel two hours later? You might find that "healthy" sugar-free gum with sorbitol is actually the secret villain.
- Check your posture. Slumping at a desk all day literalizes the "kink in the hose" metaphor for your intestines. Sit up, stretch, and give your organs some room to breathe.
- Try the low-FODMAP approach. If the pain is chronic, look into the Monash University FODMAP diet. It’s an elimination protocol designed specifically to identify which carbohydrates are fermenting too quickly in your gut.
Learning how to help gas pain is really about becoming an expert on your own body. What works for your friend might not work for you because your internal bacterial makeup is as unique as your fingerprint. Start with the physical moves—the poses and the walks—and then look at the chemistry of what you're putting into the system. Most of the time, relief is just a stretch or a lifestyle tweak away.
Keep a bottle of peppermint oil or tea in your desk. Keep a heating pad at home. Most importantly, stop worrying about the "embarrassment." Everyone gasses. The goal isn't to stop it entirely—that's impossible—it's just to make sure it doesn't hurt when it happens.
If you've been dealing with this for more than a few weeks without improvement despite changing your habits, it's worth asking a gastroenterologist about SIBO (Small Intestinal Bacterial Overgrowth). This is when bacteria that should be in your large intestine migrate up into the small intestine, causing gas to form much higher up than it should, often leading to intense pain and bloating almost immediately after eating. Identifying this requires a specific breath test, but it's a common "missing link" for people who feel like they've tried everything else.