It starts with a tingle. Maybe you think you stubbed your toe or wore shoes that were a bit too tight during that long walk yesterday. Then, usually around 2:00 AM, the world ends. Your big toe—or your ankle, or your knee—feels like it’s being crushed in a hydraulic press while simultaneously being roasted over an open flame. Even the weight of a bedsheet feels like a lead slab. If you’re searching for how to get rid of gout quickly, you’re probably in that exact moment of desperation.
Gout isn't just a "rich man's disease" from Victorian novels. It’s a form of inflammatory arthritis triggered by monosodium urate crystals. Basically, your body has too much uric acid, and it decides to park that extra grit in your joints.
You want the pain gone. Now.
The immediate "get out of pain" protocol
If you are currently mid-flare, the first thing you need to do is stop the inflammatory cascade. You can't just "walk it off." In fact, walking on a gout-afflicted joint is a terrible idea because you're literally grinding needle-like crystals into your synovial tissue.
Hydrate like it’s your job. Seriously. Drink water until you’re tired of walking to the bathroom. Uric acid is processed by your kidneys. If you’re dehydrated, those kidneys can’t flush the crystalline sludge out of your system. Aim for at least 8 to 12 glasses of water a day during a flare. Avoid soda. Definitely avoid beer. Alcohol is a double whammy; it’s high in purines and it dehydrates you, which is why flares often happen the morning after a few drinks.
Ice, don't heat. While a warm bath sounds relaxing, heat can actually increase blood flow to the area and potentially worsen the swelling during the acute phase. Use an ice pack for 20 minutes at a time. It numbs the nerves and helps constrict the blood vessels that are pumping inflammatory markers into the joint.
NSAIDs are your best friends (with a caveat). Over-the-counter options like ibuprofen (Advil) or naproxen (Aleve) are the standard starting line. However, avoid aspirin. It sounds counterintuitive, but aspirin can actually interfere with uric acid excretion, potentially making the flare last longer or get worse. If you have a prescription for Indomethacin or Celecoxib, those are usually heavy hitters that doctors prefer for gout.
📖 Related: Why the 45 degree angle bench is the missing link for your upper chest
Why Colchicine is the "Gold Standard" (If you're fast enough)
If you can call your doctor the second you feel that first "twinge," ask about Colchicine. It’s an old-school drug derived from the autumn crocus plant. It doesn't lower uric acid levels, but it stops the white blood cells from attacking the crystals.
The trick? You have to take it early.
If you wait two days into a flare to start Colchicine, the "inflammatory party" is already in full swing, and the drug won't do much. Research published in the Journal of Rheumatology suggests that low-dose colchicine is just as effective as high doses but with way fewer... let's call them "gastrointestinal surprises."
The cherry juice myth vs. reality
You've probably heard that tart cherry juice is a miracle cure. People swear by it. Honestly, there is some actual science here, not just "woo-woo" folklore.
Tart cherries contain anthocyanins. These are antioxidants that have been shown to lower uric acid levels and reduce inflammation. A study involving 633 gout patients found that consuming cherries or cherry extract reduced the risk of gout attacks by 35% over a two-day period.
Is it going to stop a massive flare in its tracks like a steroid shot? Probably not. But drinking 8 ounces of unsweetened tart cherry juice twice a day during a flare might shave a day or two off your recovery time. Just make sure it’s the tart stuff (Montmorency), not the sugary "cherry cocktail" from the soda aisle. Sugar—specifically fructose—is a massive trigger for gout.
👉 See also: The Truth Behind RFK Autism Destroys Families Claims and the Science of Neurodiversity
How to get rid of gout quickly when OTC meds fail
Sometimes, Advil is like throwing a squirt gun at a forest fire.
If the pain is 10/10 and you can’t put your foot on the floor, you need a corticosteroid. This is usually Prednisone. It’s the "nuclear option." Within 4 to 12 hours of taking a high-dose steroid, most people feel a significant drop in pressure.
The Cortiscone Injection.
If only one joint is screaming, a doctor can inject a steroid directly into the joint. It’s not fun to have a needle put into a joint that already hurts, but the relief is almost instantaneous. It bypasses your digestive system and goes straight to the source of the agony.
Understanding the "Uric Acid Paradox"
Here’s something most people get wrong: Do not start Allopurinol during a flare.
If you aren't already on a uric-acid-lowering medication, a flare is the worst time to start one. Why? Because a sudden drop in blood uric acid levels can cause the crystals in your joints to shift or partially dissolve, which actually triggers more inflammation. You have to wait until the flare is completely gone—usually about two weeks—before you start the long-term maintenance drugs.
What you should eat right now (and what to bury in the backyard)
Dietary triggers are real, but they aren't the only cause. Most uric acid comes from your own body's cell turnover, not just your dinner. Still, you don't want to add fuel to the fire.
✨ Don't miss: Medicine Ball Set With Rack: What Your Home Gym Is Actually Missing
- The "No" List: Shellfish (shrimp, scallops, mussels), organ meats (liver), red meat (especially game meats like venison), and high-fructose corn syrup.
- The "Yes" List: Low-fat dairy. This is a weird one, but proteins in milk (casein and lactalbumin) actually help your kidneys excrete uric acid. A bowl of low-fat yogurt might actually be better for your gout than a salad.
- Coffee: Good news! Coffee consumption is associated with lower uric acid levels. If you’re a caffeine addict, don't stop now.
Lifestyle shifts that actually matter
Getting rid of the pain is phase one. Keeping it away is phase two.
Gout is often a "canary in the coal mine" for other issues like hypertension, kidney disease, or insulin resistance. If you’re carrying extra weight, that fat tissue produces inflammatory cytokines that make gout flares more frequent.
Vitamin C Supplementation. Some studies suggest that 500mg of Vitamin C daily can modestly lower uric acid levels. It’s not a cure-all, but it’s a cheap, low-risk way to help your kidneys out.
Check your blood pressure meds. Are you on a "water pill" (diuretic) like Hydrochlorothiazide? Diuretics are notorious for causing gout flares because they decrease the amount of fluid in your body, concentrating the uric acid. Talk to your doctor about switching to Losartan if you have high blood pressure; Losartan is one of the few BP meds that actually helps lower uric acid.
Real-world recovery timeline
How long does this actually take?
- Untreated: A flare can last 7 to 14 days.
- Treated with NSAIDs/Colchicine: Usually 3 to 5 days.
- Treated with Steroids: Often 24 to 48 hours for major relief.
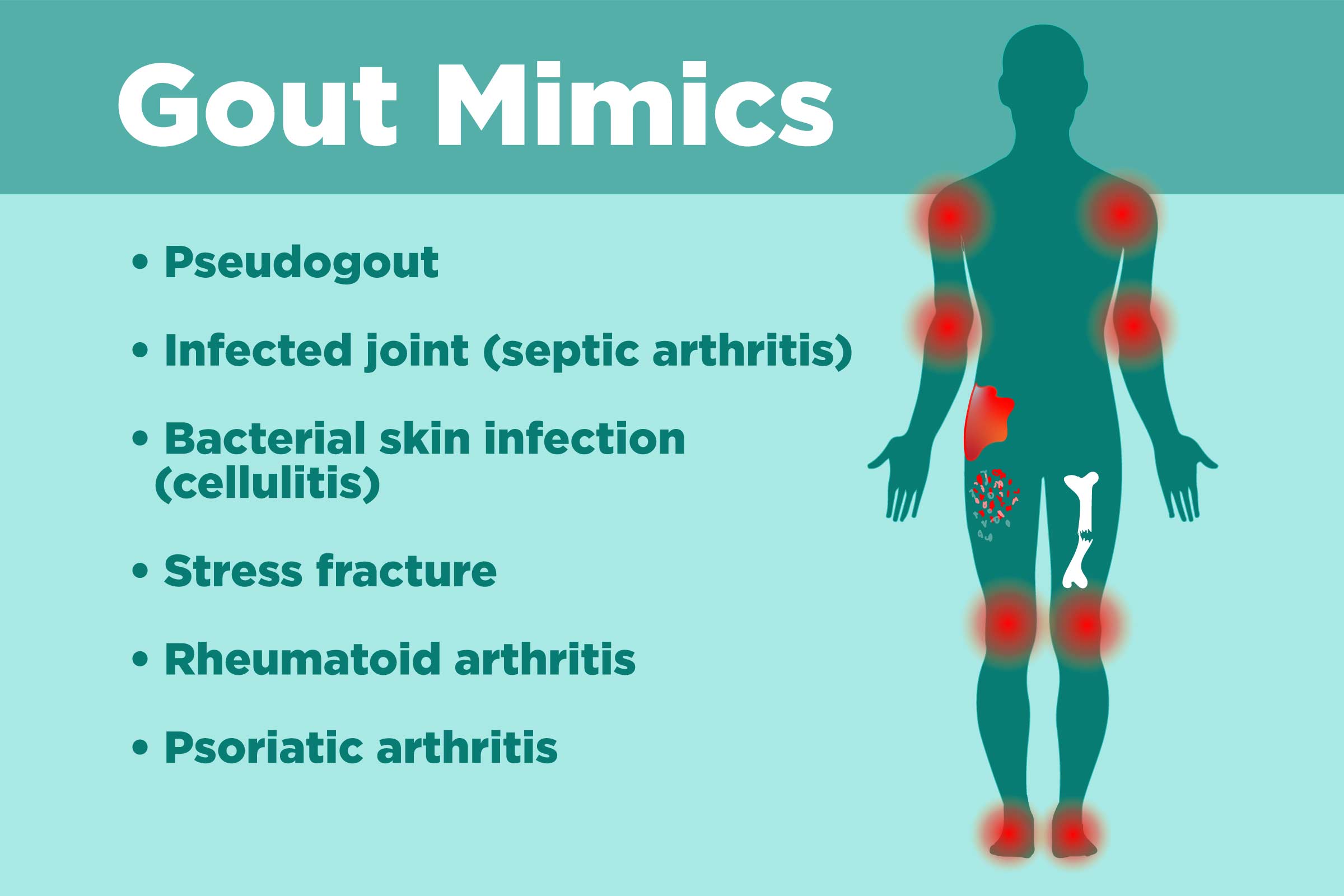
If you are on day four and things are getting redder, hotter, or you develop a fever, stop reading and go to Urgent Care. That could be "septic arthritis," which is an infection in the joint. It looks exactly like gout but can destroy your joint or lead to sepsis if you just try to "cherry juice" your way through it.
Actionable Steps for Immediate Relief
To wrap this up, if you’re hurting right now, follow this sequence:
- Immobilize and Elevate: Get that joint above the level of your heart. Use pillows. Gravity helps drainage.
- Ice: 20 minutes on, 20 minutes off.
- Hydrate: Drink a tall glass of water every hour you're awake.
- Medicate: Take 400-600mg of Ibuprofen (if your stomach and kidneys allow) or your prescribed Colchicine.
- Call your GP: Ask for a Prednisone pack or a referral to a Rheumatologist if this is your second flare in a year.
- Switch to "Gout-Safe" Fuel: Stick to eggs, low-fat dairy, complex carbs, and plenty of water for the next 72 hours.
Gout is manageable, but it requires being proactive rather than just reactive. Once the fire is out, get a blood test to check your "SUA" (Serum Uric Acid) levels. If they are above 6.0 mg/dL, you’re at risk for another attack, and it’s time to talk about long-term prevention.