You’re lying on the exam table, staring at a poster of the human anatomy, and suddenly you feel that sharp, breathtaking pinch. It’s done. The IUD is in. But then the real question hits you as you’re trying to stand up without wobbling: how long should cramping last after IUD insertion, and when does "normal" cross the line into "something is wrong"?
Most doctors give you a quick pat on the shoulder and say you’ll feel "some discomfort" for a few days. Honestly, that’s a bit of an understatement for a lot of people.
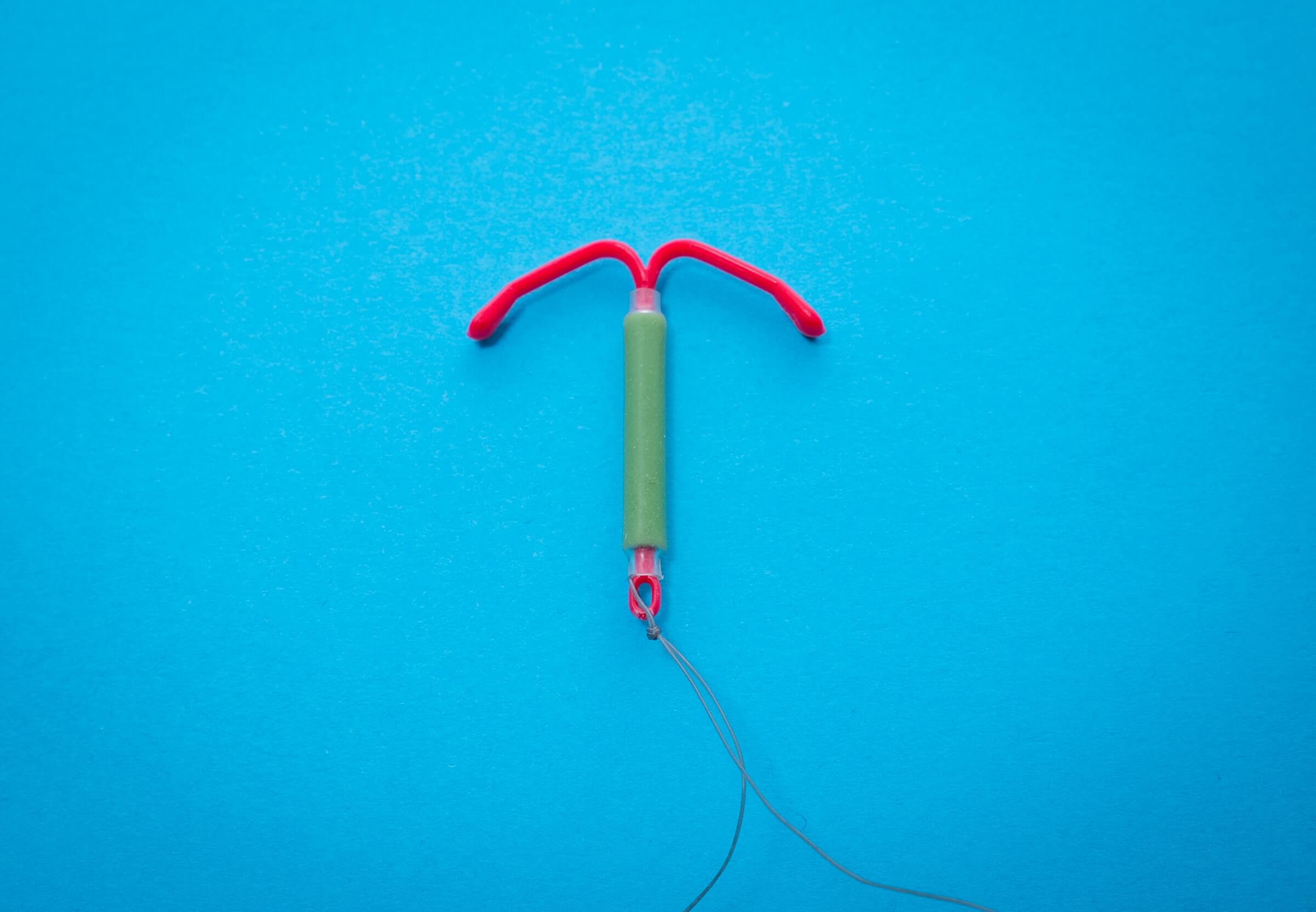
The reality is that your uterus just had a foreign object—granted, a very small, medical-grade one—placed inside it. It’s going to complain. For some, the cramps are a brief afternoon annoyance. For others, it’s a weeks-long saga of heating pads and Ibuprofen. Understanding the timeline helps you stop panicking every time you feel a twinge.
The immediate aftermath: The first 24 to 48 hours
The first two days are usually the peak.
During the procedure itself, the tenaculum (the tool used to steady the cervix) and the insertion tube cause acute localized pain. Once you leave the clinic, the "IUD crash" or the immediate inflammatory response kicks in. According to the American College of Obstetricians and Gynecologists (ACOG), most patients experience the most intense cramping within the first 24 to 48 hours.
It feels like heavy period cramps. Sometimes it’s a dull ache; sometimes it’s a sharp, stabbing sensation that radiates down your thighs or into your lower back. This happens because the uterus is a muscle. When something is inserted, it contracts to try and push it out. It’s literally trying to do its job.
If you’re using a copper IUD like ParaGard, the initial inflammatory response might be slightly more aggressive than with hormonal versions like Mirena or Kyleena. Copper works by creating an environment that's toxic to sperm, which involves a bit of a localized immune response. That means more prostaglandins. More prostaglandins mean more cramping.
Settling in: The first 2-4 weeks
So, you’ve made it past the first weekend. You’re back at work or school, but you still feel that familiar tugging in your pelvis.
Is this normal? Usually, yes.
It’s very common for intermittent cramping to persist for the first few weeks. It might not be constant. You might feel totally fine at 10:00 AM and then be doubled over by 3:00 PM. This is often triggered by physical activity, sex, or just the uterus continuing to adjust to its new roommate.
💡 You might also like: Mutual Masturbation: Why More Men Are Rethinking Solo Sex
Dr. Jennifer Gunter, a noted OB-GYN and author of The Vagina Bible, often points out that the uterus needs time to accommodate the device. It isn't an instant adaptation. Think of it like a new pair of shoes—not the most scientific analogy, sure, but it fits. The first few days are blisters; the next few weeks are just "breaking them in."
If you find that the cramps are manageable with over-the-counter meds like Naproxen (Aleve) or Ibuprofen (Advil), you’re likely on a standard trajectory.
The long game: Three to six months
This is where the divergence happens between the copper IUD and hormonal IUDs.
If you have a hormonal IUD, your periods might start thinning out or disappearing entirely. However, during those first three to six months, "random" cramping can happen as your endometrial lining thins. Your body is recalibrating its hormonal rhythm.
With the copper IUD, the story is different. The ParaGard is known for potentially causing heavier, more painful periods for the first six months. Many users report that their period cramps are significantly more intense during this adjustment phase. If you're wondering how long should cramping last after IUD insertion with a copper device, the answer is often "until your sixth cycle." After that half-year mark, things usually level off.
When the timeline isn't normal: Red flags to watch for
We need to talk about the scary stuff for a second, because "toughing it out" isn't always the right move.
While cramping is expected, certain symptoms mean the IUD isn't sitting right or there's a complication.
Malposition and Expulsion
Sometimes the uterus is just too good at its job. In about 2% to 10% of cases, the uterus successfully pushes the IUD out. This is called expulsion. If you feel sudden, worsening pain followed by a feeling of "something" in your vaginal canal, your IUD might be partially expelled.
Perforation
This is rare—occurring in about 1 out of every 1,000 insertions—but it happens. This is when the IUD pokes through the wall of the uterus. The pain here isn't usually a "cramp." It’s a sharp, intense, persistent pain that doesn't respond to painkillers.
Pelvic Inflammatory Disease (PID)
There is a slight increase in the risk of PID in the first 20 days after insertion, usually because bacteria were introduced into the uterus during the procedure. If your cramping is accompanied by:
- Fever or chills.
- Foul-smelling discharge.
- Pain during intercourse that feels "deep."
- Severe tenderness in the lower abdomen.
Then stop reading this and call your doctor. Honestly.
🔗 Read more: Pull Up Training: Why Your Progress Has Probably Stalled
Managing the discomfort (What actually works)
You don't just have to sit there and suffer.
Prostaglandin inhibitors are your best friend. Prostaglandins are the chemicals that tell your uterus to contract. Ibuprofen is a prostaglandin inhibitor. Taking it on a schedule—rather than waiting for the pain to become unbearable—is the most effective way to stay ahead of the curve.
Heat is also a legitimate medical intervention here. A heating pad increases blood flow to the pelvic region, which helps the uterine muscle relax. If you’re at work, those stick-on heating patches that go inside your underwear are a lifesaver.
Some people find that light movement—like a gentle walk—helps, while others find it makes the "tugging" sensation worse. Listen to your body. If it says "stay on the couch," stay on the couch.
The psychological aspect of IUD pain
There’s a weird mental toll when you have pain inside your body that you can’t "see."
It’s easy to spiral into thinking the IUD is falling out or that something is wrong. Check your strings. Your doctor should have shown you how to feel for the two thin plastic threads at the top of your vaginal canal. If you can feel the strings (and only the strings, not the hard plastic of the IUD), the device is where it should be. Knowing that can significantly lower your stress levels, which in turn helps your muscles relax.
✨ Don't miss: Finding Your Way to the Strada Center Mobile AL: What to Expect and Why It Matters
Actionable steps for your recovery
If you are currently in the thick of it, here is the roadmap for what to do next.
- Track the timing: Use a period tracking app to note when the cramps happen. Are they random? Or are they tied to your cycle? This data is gold for your doctor if you need a follow-up.
- The 48-hour rule: If your pain is getting worse after the 48-hour mark rather than better, call the clinic. It might be nothing, but they can do a quick ultrasound to check the placement.
- Optimize your Meds: Don't just take one pill. Take the recommended dose of Ibuprofen every 6 hours (if your stomach can handle it) for the first two days to keep those prostaglandins suppressed.
- Check the strings once a month: Do this after your period. It’s the easiest way to confirm everything is still in place without needing a doctor’s visit.
- Wait for the six-month "Gold Standard": Most providers agree that you shouldn't give up on an IUD until you’ve hit the six-month mark. This is usually when the "random" cramping stops and the body fully accepts the device.
If you are beyond the three-month mark and still find yourself relying on painkillers daily, it is time to schedule a transvaginal ultrasound. It's possible the IUD is sitting slightly low or tilted, which can cause chronic irritation. You don't have to live with constant pain for the sake of contraception; sometimes a simple adjustment or a different brand is all it takes to fix the issue.