It’s the question everyone asks while staring at the popcorn ceiling of the doctor’s office. You’re lying there, feet in stirrups, feeling that weird, sharp "pinch" that definitely feels more like a structural rearrangement of your internal organs than a simple pinch. You want to know one thing. How long do you cramp after an iud insertion?
Honestly, the answer is rarely a clean "twenty-four hours."
If you’ve just had a Paragard (copper) or a hormonal option like Mirena or Kyleena tucked into place, your uterus is currently throwing a bit of a tantrum. It’s a muscle. It’s confused. There is a new, T-shaped guest in its living room, and it’s trying to evict it. This process isn't always a quick one, and for some people, the cramping can feel like a dull background hum for weeks, while for others, it’s a three-day storm that clears out completely.
The First 48 Hours: The Peak of the Protest
Most people experience the most intense discomfort within the first two days. This is the acute phase. Your cervix was dilated slightly, and the "sounding" process—where the provider measures the depth of your uterus—causes the most immediate, sharp cramping. Once the device is actually in, the uterus tends to spasm.
According to various clinical guidelines from the American College of Obstetricians and Gynecologists (ACOG), most patients can return to normal activities almost immediately, but "normal" is a relative term. You might be able to walk to your car, but you probably won't want to hit a CrossFit class. The initial cramping usually feels like very heavy period pains. It’s deep. It’s achy. Sometimes it radiates into your lower back or down your thighs.
Expect the first 24 to 48 hours to be the roughest. You’ll likely find yourself clutching a heating pad and wondering if you made a mistake. You didn’t. Your body is just doing what it’s designed to do when a foreign object is introduced.
📖 Related: Why the EMS 20/20 Podcast is the Best Training You’re Not Getting in School
Moving Into the First Month: The Transition Period
After those first few days, the sharp, "take-your-breath-away" cramps should subside. However, many people find that they still get random twinges or "phantom" cramps for the first few weeks.
Why?
Because your uterus is still adjusting to the physical presence of the IUD. If you have a hormonal IUD (like Mirena, Liletta, Kyleena, or Skyla), the progestin is starting to thin your uterine lining. This process can cause irregular spotting and intermittent cramping as the tissue changes. If you have the copper IUD, it works by producing an inflammatory response that is toxic to sperm. That inflammation can, unfortunately, make your first few periods after insertion feel significantly more intense.
Generally, doctors tell you to wait out the first three to six months for things to "settle." That sounds like a long time. It is a long time. But the frequency of the cramps usually drops off significantly after the first cycle. If you are still asking yourself how long do you cramp after an iud after the three-month mark, it’s worth noting that the intensity should be much lower than it was on day one.
Differences Between Copper and Hormonal IUDs
The type of IUD you chose changes the math on the cramping timeline.
👉 See also: High Protein in a Blood Test: What Most People Get Wrong
- Copper IUD (Paragard): This one is the marathon runner of birth control, but it has a steeper "adjustment tax." Because it doesn't use hormones, it relies on a local inflammatory reaction. This often leads to heavier, crampier periods for the first 6 months. Some users find their periods stay slightly more intense for the duration of the device's life.
- Hormonal IUDs: These usually lead to less cramping in the long run. While the first month might involve some annoyance as your body adjusts to the hormones, most people eventually experience much lighter periods—or no periods at all. This means that while you might cramp initially, you’re often trading that for years of pain-free cycles.
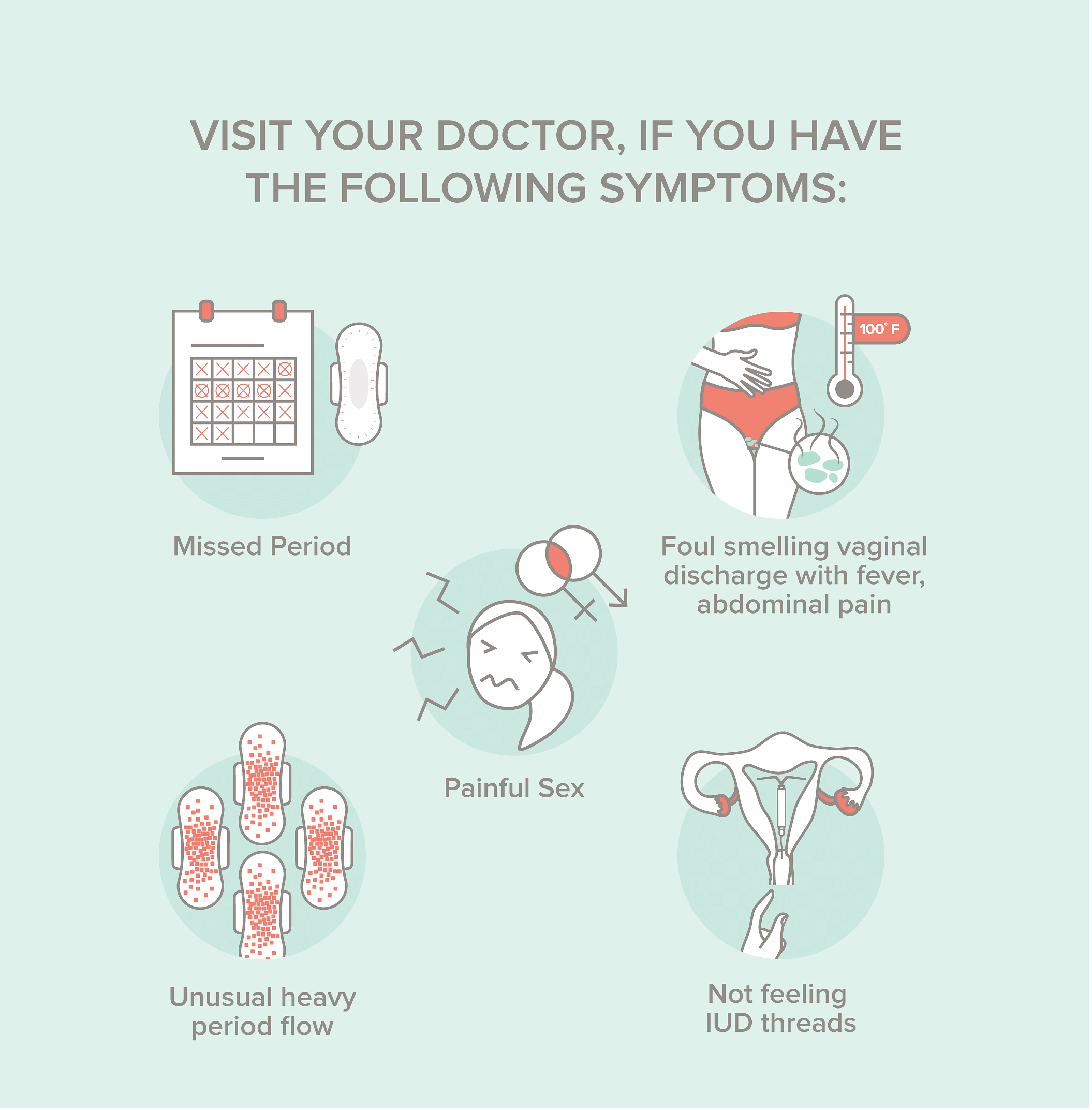
When the Cramping Is Actually a Warning Sign
It’s easy to dismiss pain as "normal," but there are specific times when you need to stop toughing it out.
If the cramping is so severe that over-the-counter meds like ibuprofen or naproxen don’t touch it, that’s a red flag. If you develop a fever, or if the vaginal discharge smells... well, wrong... you could be looking at an infection like Pelvic Inflammatory Disease (PID), which occasionally happens if bacteria are introduced during insertion.
There is also the "E" word: Expulsion.
About 2% to 10% of IUDs are pushed out by the uterus. This usually happens in the first few months. If your cramping suddenly becomes excruciating or you feel like something is literally "poking" out of your cervix, your uterus might be winning the fight and pushing the IUD out. You’ll need an ultrasound to check the placement.
Then there’s perforation. It’s rare—occurring in about 1 out of every 1,000 insertions—but if the IUD pokes through the uterine wall, the pain won't feel like a period cramp. It will feel like a medical emergency.
✨ Don't miss: How to take out IUD: What your doctor might not tell you about the process
Strategies for Managing the Post-Insertion Ache
You don't have to just sit there and suffer. There are ways to make this transition smoother.
- Scheduled Ibuprofen: Don't wait for the pain to peak. If your doctor clears it, taking 400-600mg of ibuprofen every six hours for the first two days can keep the prostaglandin levels down. Prostaglandins are the chemicals that make your uterus contract. Shut them down early.
- Heat is Your Best Friend: A high-quality heating pad or those wearable heat patches can increase blood flow to the pelvic region and relax the uterine muscle.
- Check Your Strings: Once a month, after your period (if you still have one), feel for the strings. Knowing the IUD is in the right place can alleviate the anxiety that often makes physical pain feel more intense.
- Magnesium Supplements: Some experts suggest magnesium can help relax smooth muscle tissue. Talk to your doctor, but a little extra magnesium in the week following insertion might take the edge off the spasms.
The Long-Term Outlook
So, how long do you cramp after an iud in total?
For the vast majority of people, the story ends within 3 to 7 days for the "real" pain, and 3 to 6 months for the occasional "reminders." By the time you hit the one-year mark, most hormonal IUD users actually report a significant reduction in menstrual pain compared to what they had before the IUD.
If you are currently on day three and feeling miserable, hang in there. Your body is doing a massive amount of internal recalibration. It’s annoying. It’s uncomfortable. But for most, the "set it and forget it" peace of mind that comes after the cramping stops is well worth the initial few days of heating pads and sweatpants.
Real-World Action Steps
- Track the pain: Keep a simple note on your phone. Is it getting better each day? If the trend line is going down, you’re likely fine. If the pain is ramping up on day four or five, call the clinic.
- Stay Hydrated: Dehydration can actually make muscle cramps worse, including uterine ones.
- Pelvic Floor Awareness: Sometimes we hold so much tension in our pelvic floor because we expect pain. Try some diaphragmatic breathing to consciously relax the muscles around your pelvis.
- Follow-up Appointment: Most clinics want to see you 4 to 6 weeks after insertion. Don't skip this. They will check the strings and ensure the IUD hasn't shifted, which is the best way to get a definitive answer on why you might still be feeling those twinges.
The "adjustment period" is a real thing, not just something doctors say to get you out of the office. Give your body some grace while it figures out its new roommate.