You’re staring at that little plastic blister pack and realize there’s still a pill sitting in yesterday’s slot. Your stomach drops. It’s that classic, panicked moment millions of people face every year. We’re told these tiny things are medical miracles, but the gap between the lab results and what happens in your real, messy life is actually pretty huge.
So, how effective is birth control pill therapy when life gets in the way?
If you ask a pharmaceutical rep, they’ll tell you it’s 99%. That’s the "perfect use" number. It assumes you are a literal robot who never sleeps through an alarm, never gets a stomach flu, and never forgets their purse on a weekend trip. In the real world—where humans are forgetful and pharmacies run out of stock—the "typical use" effectiveness is closer to 91%. That’s a massive difference. It means about 9 out of 100 people using the pill will get pregnant over the course of a year.
👉 See also: Is There Still an Adderall Shortage 2025: What Most People Get Wrong
The Math Behind the Hormone
Let’s get into the weeds. Most combined oral contraceptives (COCs) work by shutting down ovulation. No egg, no party. They also thicken your cervical mucus, making it basically a brick wall for sperm.
But here is the catch.
The hormones need to stay at a consistent level in your bloodstream to keep the ovaries "asleep." When you miss a dose, those levels dip. If they dip low enough, your brain might send a signal to the ovaries saying, "Hey, false alarm, go ahead and release an egg." According to the CDC and the Faculty of Sexual and Reproductive Healthcare (FSRH), the risk level depends entirely on when in the pack you messed up.
Missing a pill in the middle of the pack? Usually not a crisis. Missing one at the very beginning or the very end of the hormone cycle? That’s the danger zone. This is because you’re essentially extending the "placebo week," giving your body too much time to recover and potentially ovulate.
Progestin-Only vs. Combined Pills
Timing isn't just a suggestion for everyone. If you’re on the "mini-pill" (progestin-only), your window for error is tiny. Three hours. That’s it. If you’re 181 minutes late, your protection might be compromised because these pills rely heavily on thinning the uterine lining and thickening mucus, which wears off fast. Combined pills (estrogen and progestin) are a bit more forgiving, usually giving you a 12-to-24-hour grace period before you’re officially in "missed pill" territory.
Real Factors That Tank Your Protection
It isn't just about memory. Your body is a chemistry lab, and other things can mess with the formula.
Antibiotics and Interactions
You’ve probably heard that antibiotics ruin the pill. That’s mostly a myth, with one big exception: Rifampin. This drug, used for tuberculosis, is a known pill-killer. However, certain anti-seizure medications and even St. John’s Wort (that herbal supplement for mood) can rev up your liver enzymes. When your liver works too fast, it clears the birth control hormones out of your system before they can do their job.
The Stomach Flu Factor
If you throw up within two hours of taking your pill, your body didn't absorb it. Period. It's the same as if you never took it. Severe diarrhea for more than 24 hours also prevents absorption. Most people forget to count "sick days" as "missed pill days," which is how many "miracle" pregnancies actually start.
BMI and Effectiveness
There has been ongoing debate in the medical community, specifically regarding studies published in the American Journal of Obstetrics and Gynecology, about whether a higher Body Mass Index (BMI) impacts how effective is birth control pill metabolism. Some data suggests that for individuals with a BMI over 30, the hormones might take longer to reach steady levels, or the "steady state" might be lower. It's not a settled science, but it's a nuance many doctors fail to mention during a ten-minute checkup.
What Happens If You Miss One?
Don't spiral. Honestly, the protocol is usually straightforward, but you have to be clinical about it.
If you missed one pill (even if it’s been 24 hours):
Take it as soon as you remember. Even if that means taking two pills in one day. You are likely still protected against pregnancy.
If you missed two or more:
This is where you need backup. Use a condom for the next seven days. If you had unprotected sex in the days leading up to the double-miss, and it was in the first week of the pack, you might actually need emergency contraception (the Morning After Pill).
Why the Failure Rate is Higher Than You Think
We focus on the pills, but we should focus on the pharmacy. "Access failure" is a huge part of the 91% statistic. A 2022 study highlighted in JAMA Network Open noted that many users experience "gaps" in their prescription due to insurance hurdles or pharmacy stocking issues. A three-day gap between packs is a recipe for ovulation.
Then there's the "Midnight Shift" problem. People who work irregular hours—nurses, bartenders, pilots—struggle the most with pill consistency. When your "morning" is at 4 PM one day and 11 AM the next, your hormonal baseline becomes a rollercoaster.
Moving Toward Better Protection
If you find that your "typical use" is nowhere near "perfect use," it might be time to stop fighting your own biology. The pill is an incredible tool, but it’s high-maintenance. It requires 365 correct decisions a year.
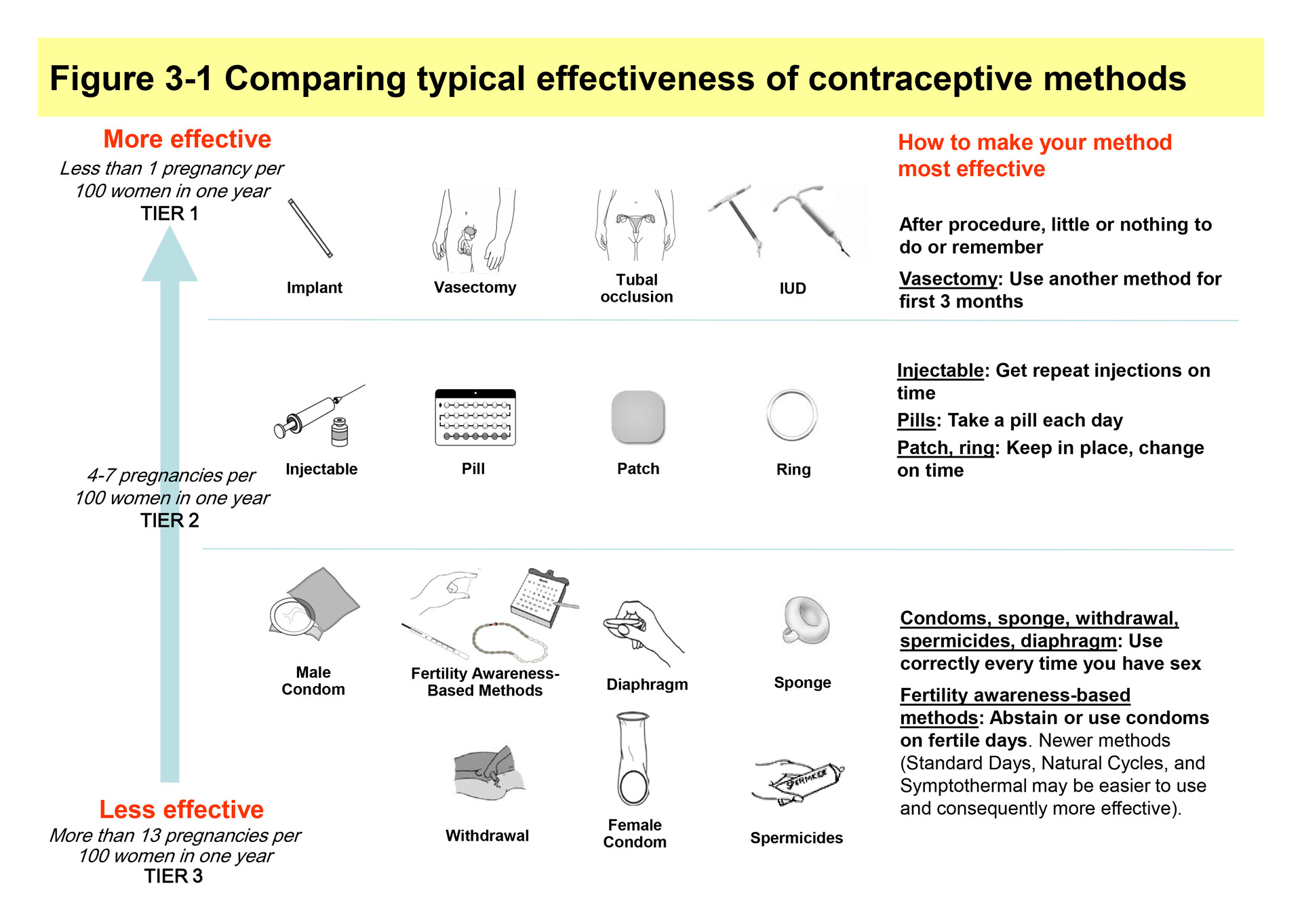
Long-Acting Reversible Contraceptives (LARCs), like the IUD or the arm implant (Nexplanon), remove the human element. Their typical use and perfect use rates are almost identical (over 99%) because you can't "forget" an IUD.
Actionable Steps for Pill Users
- Set an Alarm with a Safety Net: Don't just set one alarm. Set a "Last Chance" alarm for three hours later.
- Use an App: Use something like Clue or Spot On that pester you with notifications until you click "taken."
- The Seven-Day Rule: If you miss more than one pill or start a pack late, the "Seven-Day Rule" is your best friend. Use condoms for seven days of continuous pill-taking before trusting the hormones again.
- Keep Emergency Contraception on Hand: Don't wait until 2 AM on a Sunday to realize you need Plan B. Keep a dose in your medicine cabinet just in case. It's cheaper to buy in advance than to pay for an emergency clinic visit.
- Audit Your Meds: Check your vitamins and any new prescriptions against a drug interaction database.
Understanding how effective is birth control pill usage in your specific life requires being honest about your habits. If you're great at routines, the pill is a powerhouse. If you're chaotic, the pill is a gamble. Know which one you are before you rely on that 99% promise.