You’re sitting in a cramped exam room, and your doctor looks at your blood work with that specific, neutral "doctor face." They tell you your LDL is high. Then comes the recommendation for a little pill you’ve heard about a thousand times: a statin. It sounds simple enough, but honestly, have you ever stopped to wonder how does statin work once it actually hits your bloodstream? It isn’t just some chemical vacuum cleaner that sucks grease out of your veins. It’s way more tactical than that. It’s a molecular heist that happens inside your liver cells every single day.
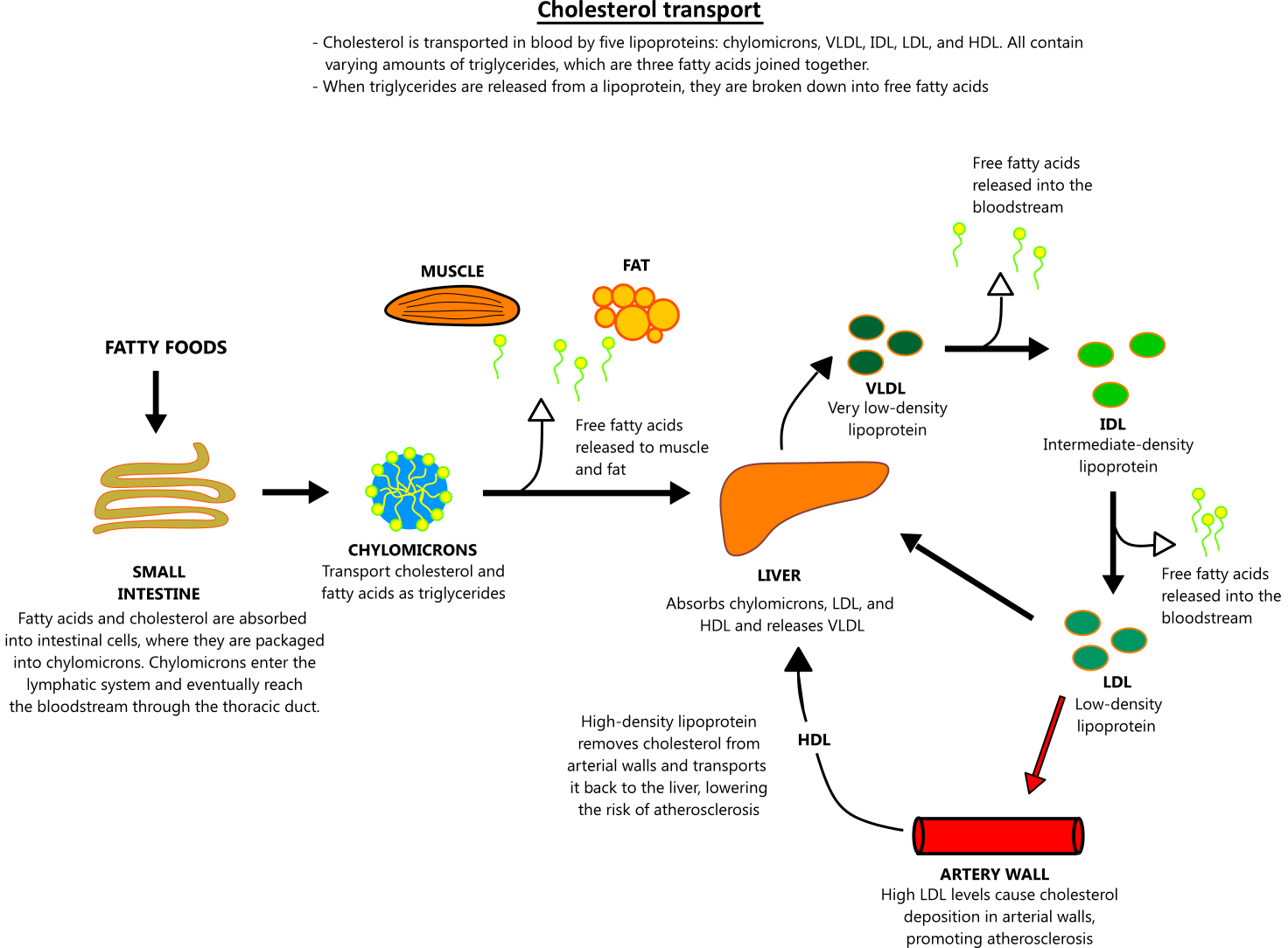
Most people think cholesterol comes entirely from the double cheeseburger they ate last Tuesday. Not really. Your liver is actually the primary manufacturer, churning out the vast majority of the cholesterol circulating in your body. It uses a complex assembly line to build this waxy substance because your body actually needs it for things like hormone production and cell walls. But when the assembly line goes into overdrive, you end up with too much "bad" cholesterol (LDL) floating around, looking for a place to crash. That "place" is usually the walls of your arteries.
The Molecular Hijack: HMG-CoA Reductase
To understand how does statin work, we have to look at a very specific enzyme with a mouthful of a name: HMG-CoA reductase. Think of this enzyme as the project manager of the cholesterol factory in your liver. Without this manager giving the green light, the production line grinds to a halt. Statins are what scientists call "competitive inhibitors." They are shaped almost exactly like the raw materials the enzyme usually grabs to start making cholesterol.
When you take a drug like atorvastatin (Lipitor) or rosuvastatin (Crestor), the statin molecules rush to the liver and sit in the enzyme's "active site." They basically take the manager’s chair before the real worker can get there. Because the enzyme is busy dealing with the statin "imposter," it can't facilitate the chemical reaction needed to create mevalonate, which is the precursor to cholesterol.
Production drops. Fast.
📖 Related: Theory of Comfort by Katharine Kolcaba: Why Nursing Care is More Than Just Medicine
But here is the cool part. The liver isn't just going to sit there and let its cholesterol levels bottom out. It panics a little. When the liver senses that it isn't producing enough internal cholesterol, it looks for an external source to fill the gap. It starts "upregulating" LDL receptors on the surface of the liver cells. These receptors act like tiny hooks that reach out into your bloodstream, grab passing LDL particles, and pull them into the liver to be broken down and recycled. This is the dual-action secret: you’re making less cholesterol and your liver is actively hunting down the stuff already in your blood.
Beyond the Numbers: The "Pleiotropic" Effects
If we only talked about lowering numbers on a lab report, we’d be missing half the story. There is a lot of buzz in the medical community—backed by major trials like the JUPITER study—about the "pleiotropic" effects of statins. This is just a fancy medical way of saying these drugs do extra jobs they weren't originally hired for.
Inflammation is the real villain in heart disease. You can have high cholesterol and be fine if your artery walls are smooth and calm. But when those walls get inflamed, they become "sticky." This is where plaque starts to build up. Statins seem to possess a remarkable ability to dial down inflammation in the vascular system. They reduce C-reactive protein (CRP) levels, which is a major marker for systemic inflammation.
Ever heard of a "vulnerable plaque"? It’s the kind that is soft, fatty, and prone to rupturing. If a plaque ruptures, it causes a blood clot, which leads to a heart attack or stroke. Statins actually help stabilize these plaques. They make the "cap" on the plaque thicker and less likely to burst. So, even if the statin doesn't completely disappear the blockage, it makes the blockage much, much safer to live with. It’s sort of like reinforcing a levee before a storm hits.
The Muscle Myth and the Nocebo Effect
We have to talk about the elephant in the room: muscle pain. It’s the number one reason people stop taking their meds. You’ve probably seen the horror stories online. While "statin-associated muscle symptoms" (SAMS) are real, they are statistically way less common than the internet would have you believe. In many double-blind trials, the rate of muscle pain in the statin group is almost identical to the placebo group.
This is what doctors call the "nocebo effect." If you expect a pill to make your legs ache, your brain is surprisingly good at making your legs ache. That said, in a small percentage of people, statins can interfere with CoQ10 production in the muscle cells, leading to actual soreness. If that happens, switching to a different type of statin—like moving from a lipophilic one (fat-soluble) to a hydrophilic one (water-soluble) like pravastatin—often fixes the problem because the drug doesn't enter the muscle tissue as easily.
👉 See also: Walking an hour a day: What most people get wrong about the 60-minute habit
Why Some Statins Feel Different Than Others
Not all statins are created equal. You’ve got your heavy hitters and your "gentle" options.
- High-Intensity: Atorvastatin and Rosuvastatin. These are the big guns. They stay in the system longer and can drop LDL by 50% or more.
- Low-to-Moderate Intensity: Simvastatin, Pravastatin, and Lovastatin. These are often used for people who only need a slight nudge or who are sensitive to side effects.
The timing matters too. Older statins like Simvastatin have a very short "half-life." Since your liver does most of its cholesterol manufacturing at night while you sleep, you have to take those pills right before bed. Newer ones like Lipitor last so long in the blood that it doesn't really matter when you take them, as long as you're consistent.
The Reality of the "Statins for Everyone" Debate
There’s a lot of pushback lately about over-prescription. Some critics, including certain cardiologists, argue that we rely too much on these drugs instead of focusing on metabolic health and insulin resistance. It's a fair point. A statin isn't a "get out of jail free" card for a sedentary lifestyle or a diet high in ultra-processed sugars.
However, for someone with familial hypercholesterolemia—a genetic condition where the liver just ignores the "stop" signal for cholesterol production—statins are literally life-saving. For these patients, diet alone usually won't move the needle enough. The drug provides a biological correction that their DNA simply can't manage on its own. It’s about risk stratification. A 45-year-old with no other risk factors might not need one, but a 60-year-old with high blood pressure and a history of smoking is a completely different story.
Making the Most of the Treatment
If you're starting a regimen, you shouldn't just swallow the pill and hope for the best. To truly optimize how does statin work for your specific body, you need a baseline and a follow-up.
First, get a full lipid panel and a liver function test before you start. Since statins work in the liver, a tiny fraction of people see an increase in liver enzymes. It’s usually harmless, but your doctor will want to keep an eye on it. Second, consider your CoQ10 levels. Since the cholesterol pathway is shared with the production of Co-Enzyme Q10, some people find that taking a supplement helps mitigate that "heavy limb" feeling.
Third, watch out for grapefruit. It sounds like an old wives' tale, but grapefruit juice contains compounds that block the enzymes (CYP3A4) that break down certain statins. This can cause the drug level in your blood to spike to dangerous levels. If you love your morning grapefruit, ask for a statin like Rosuvastatin that isn't processed by that specific enzyme.
Actionable Steps for Heart Health
Understanding the mechanism is great, but what do you actually do with this info?
- Ask for a Calcium Score: If you’re on the fence about whether you need a statin, a CAC (Coronary Artery Calcium) scan can show if there is actually hard plaque in your heart already. If the score is zero, you might have more time to try lifestyle changes first.
- Track Your Muscle Response: If you feel achy, don't just quit. Keep a log. Is it worse after a workout? Is it in both legs? This data helps your doctor decide if you need a dose adjustment or a different brand.
- Monitor Your Blood Sugar: In some people, statins can slightly raise fasting blood sugar. It’s usually not enough to cause diabetes, but it’s worth watching if you're already pre-diabetic.
- Don't Ignore Diet: Fiber is the unsung hero here. Soluble fiber (like in oats and beans) binds to bile acids in the gut and drags them out of the body. Since bile is made of cholesterol, this forces the liver to use even more LDL to make new bile, compounding the effect of the statin.
The goal isn't just a lower number on a page. It's about ensuring your blood vessels stay flexible and your "pipes" stay clear of unstable gunk that could cause a disaster ten years down the road. Statins are a tool—a very specific, enzyme-blocking tool—but they work best when they're part of a broader strategy that includes movement, stress management, and a decent diet.