It is a terrifying thought. You’re looking at baby clothes, picking out a crib, and suddenly this dark shadow creeps in: what if something goes wrong? Most of the time, we treat pregnancy like a purely joyous countdown, but for a lot of people, the fear is real. So, let’s just get into it. How common is death during childbirth, really?
Honestly, the answer depends entirely on where you are standing on a map. If you are in a high-income country, the numbers are low, but they are not zero. If you are in the United States, the numbers are actually higher than they should be for a nation with so much wealth. It’s a bit of a gut punch. According to the World Health Organization (WHO), roughly 800 women die every single day from preventable causes related to pregnancy and childbirth. That is one person every two minutes.
It sounds like a lot. It is a lot. But context is everything here.
The Numbers Game: Maternal Mortality in 2026
When we talk about maternal mortality, we aren't just talking about the moment the baby comes out. Doctors look at the "maternal mortality ratio," which tracks deaths during pregnancy, delivery, and up to 42 days after the baby is born.
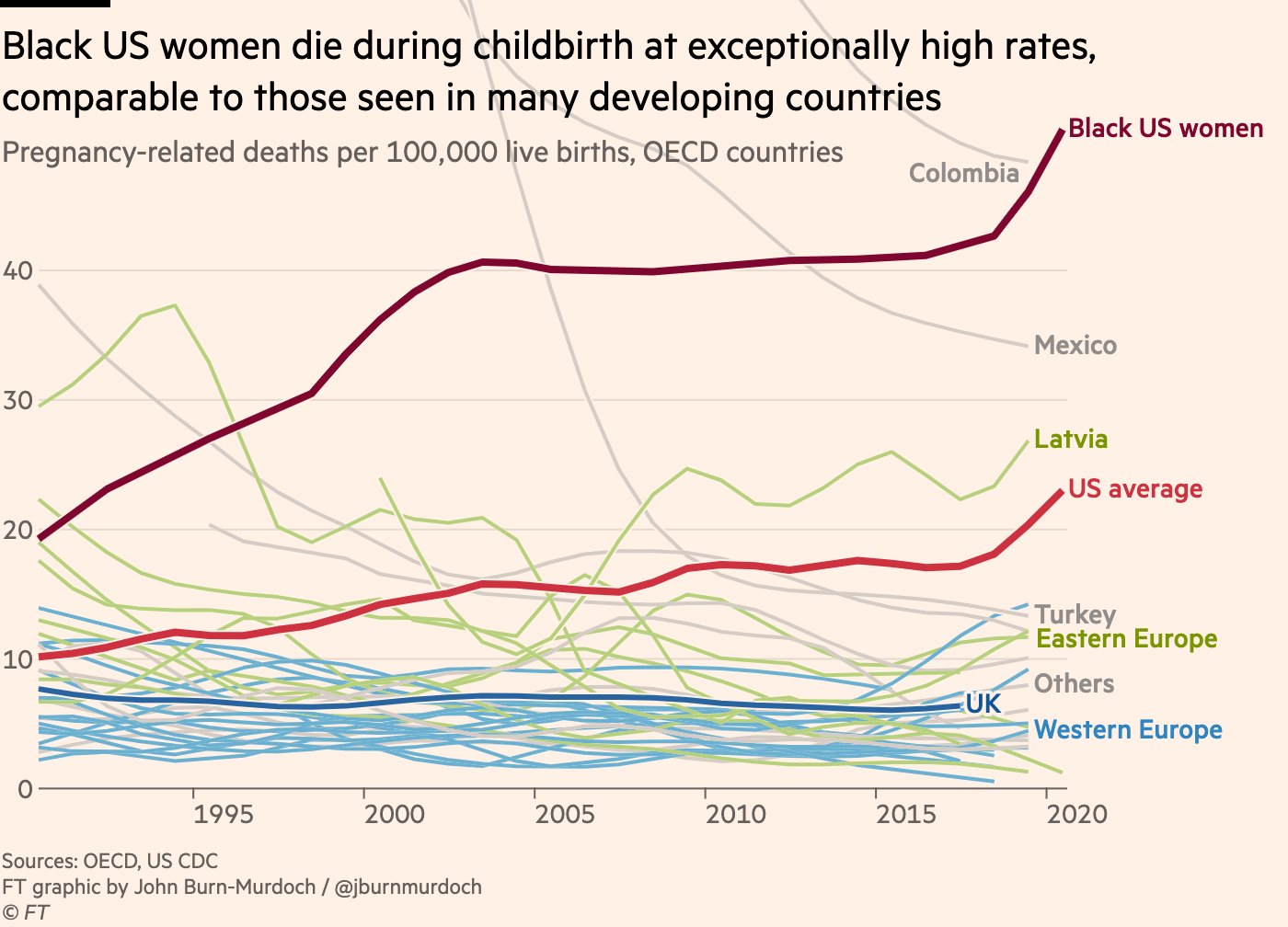
In the United States, the Centers for Disease Control and Prevention (CDC) has been tracking a worrying trend for years. While most developed nations have seen these numbers drop, the U.S. has struggled. We’re looking at roughly 22 to 32 deaths per 100,000 live births, depending on the year and the specific data set you're pulling from. Compare that to a place like Norway or Japan, where the number is closer to 2 or 3.
Why the gap? It’s not just one thing. It's a messy mix of healthcare access, underlying health conditions like hypertension or diabetes, and—honestly—how well doctors listen to patients.
What’s Actually Causing These Deaths?
People often assume it's some freak accident in the delivery room. While those happen, the reality is often more "slow burn" than "sudden trauma."
Postpartum hemorrhage is a big one. It’s basically heavy bleeding after birth. If the uterus doesn’t contract back down properly, or if there’s a tear that goes unnoticed, a person can lose a dangerous amount of blood very quickly. Hospitals have protocols for this—stages of intervention—but if the team misses the early signs, things get dicey fast.
Then you have preeclampsia and eclampsia. This is high blood pressure that can lead to seizures or organ failure. It’s sneaky. You might just feel like you have a bad headache or some swelling, which, let's be real, describes almost every pregnant person in their third trimester. But if that blood pressure spikes, it becomes a medical emergency.
Cardiovascular Conditions and Embolisms
The heart takes a beating during pregnancy. Your blood volume increases by about 50%. That is an insane amount of extra work for your pump. Cardiovascular diseases are actually a leading cause of death in the U.S. for pregnant people. Then there are pulmonary embolisms—blood clots that travel to the lungs. These are the "sudden" ones. One minute you’re fine, the next you can’t breathe.
The Racial Disparity We Can’t Ignore
We have to talk about the elephant in the room. If you are a Black woman in the United States, how common is death during childbirth for you? It is nearly three times more common than it is for white women.
This isn't just about income or education. We’ve seen stories from people like Serena Williams, who almost died after giving birth because her concerns about a blood clot weren't taken seriously at first. If one of the greatest athletes in the world struggles to get her symptoms recognized, imagine what it’s like for someone without those resources. Implicit bias in healthcare is a documented, scientific fact. It affects how pain is managed and how quickly interventions are started.
Is It Getting Safer?
Yes and no.
On a global scale, we’ve made huge strides since the 90s. More people are giving birth in facilities with skilled attendants. But in the West, we are seeing a rise in "maternal near-misses." These are cases where someone almost died but was saved by emergency medicine. For every one person who dies, about 70 to 100 others experience a severe complication.
The age of parents is also shifting. More people are having babies in their late 30s or 40s. While modern medicine makes this very safe for most, it does come with a slightly higher risk profile for things like gestational diabetes or preeclampsia, which feeds back into those mortality statistics.
Red Flags That Actually Matter
Knowing the symptoms can literally be the difference between life and death. This isn't about being paranoid; it's about being informed.
- A headache that won't quit. If Tylenol doesn't touch it and you’re seeing spots, that’s not "just a headache."
- Shortness of breath. Not the "I just walked up the stairs" kind, but the "I’m sitting still and can't catch my breath" kind.
- Extreme swelling. Specifically in the face or hands, or if one leg is way more swollen than the other.
- Thoughts of self-harm. Mental health is part of this too. Postpartum depression and psychosis are leading contributors to maternal mortality in the first year after birth.
Doctors use the "Save Her" or "AIM" protocols now to standardize care. If a patient says, "Something is wrong," the goal is to trigger a specific set of checks regardless of who the patient is or what the doctor thinks.
The Role of Midwifery and Doulas
There is a growing movement to bring more midwives into the fold. In places like the UK or the Netherlands, midwives handle the majority of low-risk births. The data suggests that this model leads to fewer unnecessary interventions, which can sometimes reduce the risk of complications.
Doulas are also becoming a huge part of the conversation. They aren't medical professionals, but they are advocates. Having someone in the room whose only job is to support you and make sure your voice is heard has been shown to improve outcomes, especially for marginalized groups.
What You Can Do Right Now
If you're pregnant or planning to be, don't let these numbers paralyze you. The vast, overwhelming majority of births end with a healthy parent and a healthy baby. But you shouldn't just "hope for the best" and stay quiet.
Find a provider who listens. If you ask a question and your doctor rolls their eyes or brushes you off, find a new one. You need a partner, not a dictator.
Build your "Postpartum Plan." Everyone plans for the birth, but the weeks after are when many complications happen. Who is checking your blood pressure? Who is watching your mood? Make sure you have a "village" that knows the warning signs of infection or hemorrhage.
🔗 Read more: Wet dreams meaning in english: What your body is actually doing while you sleep
Understand your history. If your mom had preeclampsia, tell your doctor. If you have a history of high blood pressure, be aggressive about monitoring it.
The reality is that how common is death during childbirth is a question that reveals the cracks in our social and medical systems. It is rare, but it is often preventable. By demanding better care, staying informed, and refusing to stay silent when something feels "off," we can push those numbers down where they belong.
Actionable Steps for a Safer Pregnancy
- Request a cardiovascular screening if you have any pre-existing risks or are over the age of 35.
- Monitor your own blood pressure at home during the third trimester and for six weeks postpartum. You can buy a cuff for $30, and it might save your life.
- Interview your birth hospital. Ask them about their "Hemorrhage Cart" and if they have standardized protocols for maternal emergencies.
- Trust your gut. If you feel like you are dying or something is "deeply wrong," do not let a nurse tell you it's just anxiety. Demand an evaluation.
- Secure postpartum support. Schedule a check-up for yourself at the 2-week mark, not just the standard 6-week mark. Many issues arise long before that second month.
The statistics are a sobering reminder that bringing life into the world is a massive physical undertaking. It deserves respect, and it deserves the highest level of medical attention. You aren't being "difficult" by asking questions; you're being your own best advocate.