It starts as a dull thrum. Then, it’s a roar. You’re sitting at the dinner table, maybe you just finished a bowl of pasta or a perfectly seared steak, and suddenly, your midsection feels like it’s being wrung out like a wet rag. It’s not just "fullness." It is horrible abdominal pain after eating, the kind that makes you double over and wonder if you need an ER trip or just a very long nap.
Pain is a liar. It tells you everything is a catastrophe, but the "why" behind postprandial distress (the medical term for after-meal agony) ranges from "oops, too much fiber" to "your gallbladder is throwing a literal tantrum." Most people assume it’s just gas. Sometimes it is. But when the pain is sharp, localized, or accompanied by a cold sweat, your body is trying to file a formal complaint.
The Immediate Suspects: When Your Gut Just Quits
Usually, if the pain hits within thirty minutes of your last bite, the issue is "upstairs"—meaning the stomach or esophagus. We’re talking about things like Peptic Ulcer Disease. If you have an open sore in the lining of your stomach, the arrival of gastric acid (which spikes when you eat) is like pouring lemon juice on a paper cut. It burns. It gnaws. It makes you regret the very concept of lunch.
Then there’s the gallbladder. This little pear-shaped organ stores bile. When you eat fat, the gallbladder squeezes to squirt that bile into the small intestine. If you have gallstones, that squeeze is more like a vice grip on a bag of marbles. This typically feels like a sharp, stabbing sensation in the upper right quadrant of your abdomen, and it often radiates to your back or right shoulder blade. Doctors like Dr. Elena Ivanina, a board-certified gastroenterologist, often note that gallbladder pain is notoriously "heavy" and can last for hours. It doesn't just go away with a burp.
Is it Gastroparesis? When the Engine Stalls
Sometimes the plumbing isn't clogged; it's just broken. Gastroparesis is a condition where your stomach muscles essentially stop moving. Food just sits there. It ferments. It creates pressure. For people with diabetes, this is a common, albeit miserable, complication because high blood sugar can damage the vagus nerve.
Imagine putting a pound of raw meat in a warm, dark, wet bag and leaving it there for six hours. That's essentially what happens in a gastroparetic stomach. You feel full after three bites. You feel nauseated. And the pain? It’s a constant, bloating ache that makes you want to swear off solid food forever.
The "Hidden" Culprit: Celiac and Non-Celiac Gluten Sensitivity
We talk about gluten so much it has become a punchline, but for those with Celiac disease, the horrible abdominal pain after eating a piece of sourdough is an autoimmune response. The villi in the small intestine—tiny hair-like structures that absorb nutrients—get flattened. It’s an inflammatory firestorm.
✨ Don't miss: Why Sometimes You Just Need a Hug: The Real Science of Physical Touch
Even if you don't have Celiac, you might have Non-Celiac Gluten Sensitivity or even SIBO (Small Intestinal Bacterial Overgrowth). In SIBO, bacteria that belong in the large intestine migrate north. When they hit the carbohydrates you just swallowed, they throw a party, producing gas so quickly that your intestines distend like a balloon. It’s incredibly painful. It’s also hard to diagnose without a specific breath test, which is why many people languish for years being told they just have "stress."
Pancreatitis: The Warning You Can't Ignore
If the pain is so intense you’re "boring" into your back, and it feels better when you lean forward, we might be talking about the pancreas. Chronic pancreatitis or an acute flare-up is serious. The pancreas produces enzymes to digest food. If those enzymes activate inside the pancreas instead of the intestine, the organ starts digesting itself.
This isn't a "take an antacid" situation.
Real-world cases, often cited in the American Journal of Gastroenterology, show that post-meal pancreatic pain is frequently linked to high triglycerides or heavy alcohol use, though sometimes it’s just a rogue gallstone blocking the pancreatic duct. If you’re also running a fever or vomiting, get to a professional.
Why Your "Healthy" Salad is Hurting You
It sounds counterintuitive. You ate a giant bowl of kale, chickpeas, and broccoli. You should feel like a superhero. Instead, you feel like you’ve swallowed a brick.
This is often due to FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols). These are short-chain carbohydrates that the small intestine struggles to absorb. They drag water into the gut and then get fermented by bacteria.
🔗 Read more: Can I overdose on vitamin d? The reality of supplement toxicity
- Apples and Pears: High in fructose.
- Garlic and Onions: High in fructans.
- Beans: GOS (Galacto-oligosaccharides).
If you have Irritable Bowel Syndrome (IBS), these "healthy" foods are high-octane fuel for cramping. You might find that you can eat a burger without much trouble, but a cauliflower crust pizza sends you to the floor. It’s not the calories; it’s the chemistry.
The Vascular Angle: Mesenteric Ischemia
This one is rare, but it's the "stealth" cause of post-meal agony. Think of it as a "heart attack of the gut." Just like your heart needs more blood when you run, your intestines need more blood when they’re digesting. If the arteries supplying the gut are narrowed by plaque, they can't keep up.
Patients often describe this as "food fear." They’re hungry, but they’re terrified to eat because they know the pain is coming 15 to 30 minutes later. It’s a dull, cramping sensation that doesn't go away until the meal is processed. If you’re older or have a history of smoking and heart disease, this is a possibility that your doctor needs to rule out via ultrasound or CT angiography.
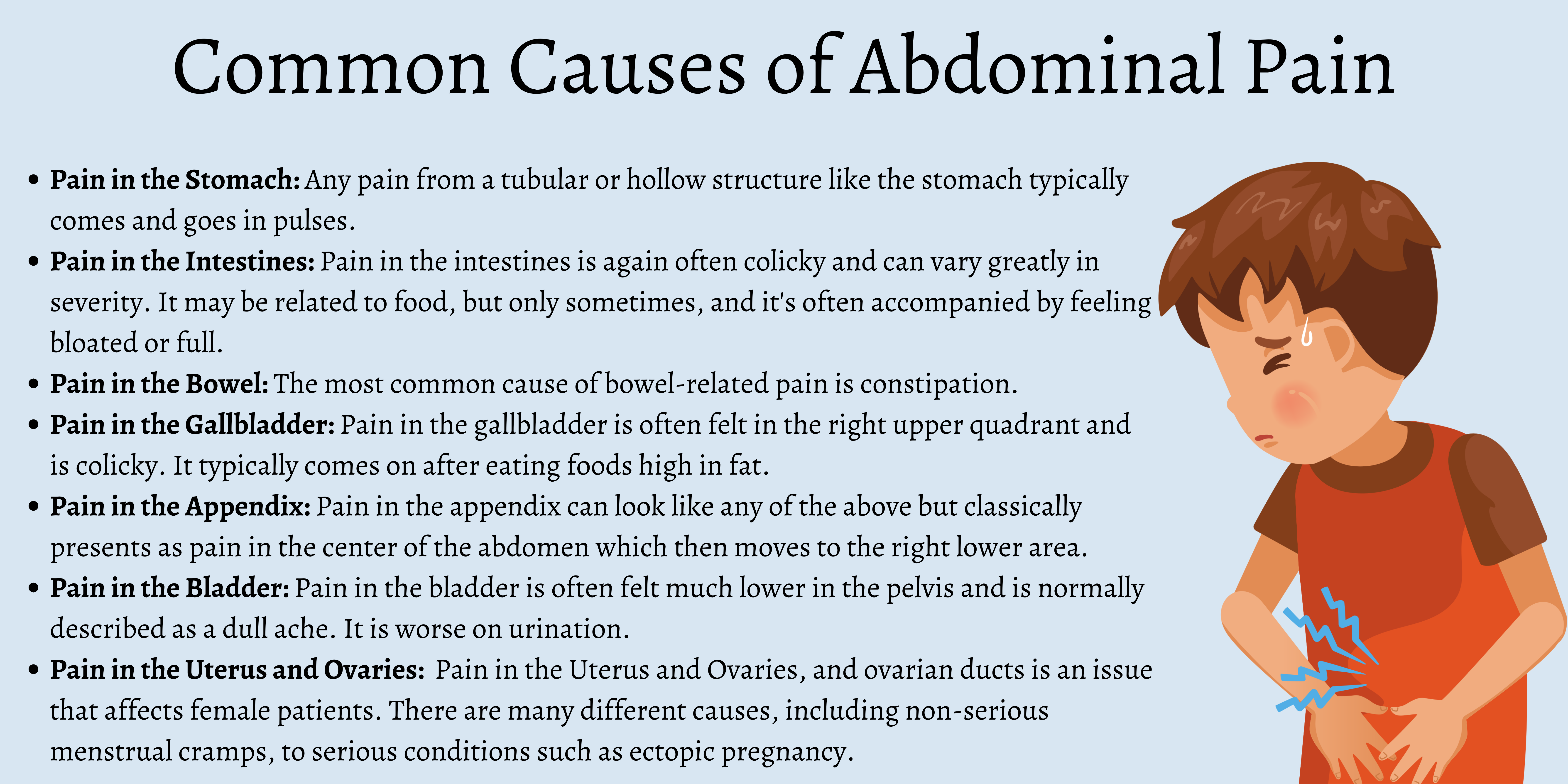
Mapping the Pain: Where Does It Hurt?
Location matters. A lot.
- Upper Middle (Epigastric): Likely reflux, gastritis, or an ulcer.
- Upper Right: Likely gallbladder or liver issues.
- Lower Right: Could be Crohn’s disease flare or, if acute, appendicitis.
- Lower Left: Often diverticulitis (inflammation of small pouches in the colon).
- Diffuse (Everywhere): Likely gas, bloating, IBS, or a food allergy.
Honestly, the human body is a messy machine. Sometimes the pain is "referred," meaning the problem is in your gallbladder but you feel it in your back. Or it's your heart—yes, some women experience heart attacks as intense indigestion or upper abdominal pain.
Practical Steps to Stop the Cycle
You can't live on broth forever. If you’re dealing with regular, horrible abdominal pain after eating, you need a strategy. This isn't medical advice—I'm an expert writer, not your doctor—but these are the evidence-based steps most specialists recommend starting with.
💡 You might also like: What Does DM Mean in a Cough Syrup: The Truth About Dextromethorphan
The Low-FODMAP Reset
Try an elimination diet for two weeks. Cut out the garlic, onions, wheat, and high-fructose fruits. If the pain vanishes, you’ve found your trigger. Monash University has the gold-standard app for tracking this. It’s tedious, but it works.
Check Your Speed
Chewing isn't just a suggestion. Your stomach doesn't have teeth. If you’re inhaling your food, you’re also inhaling air (aerophagia), which leads to massive bloating. Try the 20-chew rule. It sounds like something your grandma would say, but it fundamentally changes how much work your stomach has to do.
The Ginger Protocol
Ginger is a prokinetic. It helps the stomach empty faster. If your pain is caused by slow motility or mild gastritis, sipping ginger tea 20 minutes after a meal can actually stimulate the "migrating motor complex" to move things along.
Keep a "Pain Diary"
Don't just write what you ate. Write how you felt emotionally. The gut-brain axis is real. Stress causes the release of CRH (Corticotropin-Releasing Hormone), which makes your gut more sensitive to pain. If you only hurt when you eat lunch at your desk while reading emails, the problem might be your job, not the sandwich.
When to Seek Immediate Help
If your pain is accompanied by any of these "red flags," stop reading and call a clinic:
- Unintentional weight loss.
- Blood in the stool (black or bright red).
- Difficulty swallowing.
- Persistent vomiting.
- Pain that wakes you up in the middle of the night.
Abdominal pain is a puzzle. It takes time to solve. Start by simplifying your meals—think plain rice, steamed chicken, or clear broths—and slowly reintroduce foods one by one. This helps you isolate the culprit without having to go through invasive testing right away. Most importantly, don't ignore it. Chronic inflammation in the gut isn't just uncomfortable; it's a long-term health risk that's often entirely fixable once you identify the trigger.
Actionable Insights for Recovery
- Download a tracking app: Use something like "Bowelle" or "mySymptoms" to log every meal and the subsequent pain level for seven days. This data is gold for your doctor.
- Test for H. pylori: This common bacteria causes ulcers and can be found with a simple breath or stool test. It’s easily treated with antibiotics.
- Rule out the "Big Three": Ask your doctor specifically about Celiac disease, gallstones, and SIBO. These are the most common missed diagnoses for post-meal pain.
- Adjust meal timing: Try eating five small meals instead of three large ones. This reduces the "load" on the gallbladder and pancreas, often providing immediate relief while you search for the root cause.
- Mind your posture: Don't slump or lie down immediately after eating. Stay upright for at least 90 minutes to let gravity assist your esophageal sphincter in keeping acid where it belongs.
By narrowing down the location and type of pain, you move from "it just hurts" to a targeted plan for healing your digestive tract.