Look, let’s be real for a second. Sitting in a cold doctor’s office waiting room, flipping through a three-year-old magazine while everyone wonders why you’re there, is basically nobody's idea of a good time. It’s awkward. It’s often expensive. And for a lot of people, that discomfort is exactly why they skip testing entirely. That is why the home std test kit has become such a massive deal lately. You can basically pee in a cup or prick your finger while watching Netflix, mail it off, and get your results on your phone. It sounds like the perfect solution for the modern age of convenience, but there is a lot of nuance people miss when they're scrolling through options on Amazon or pharmacy websites.
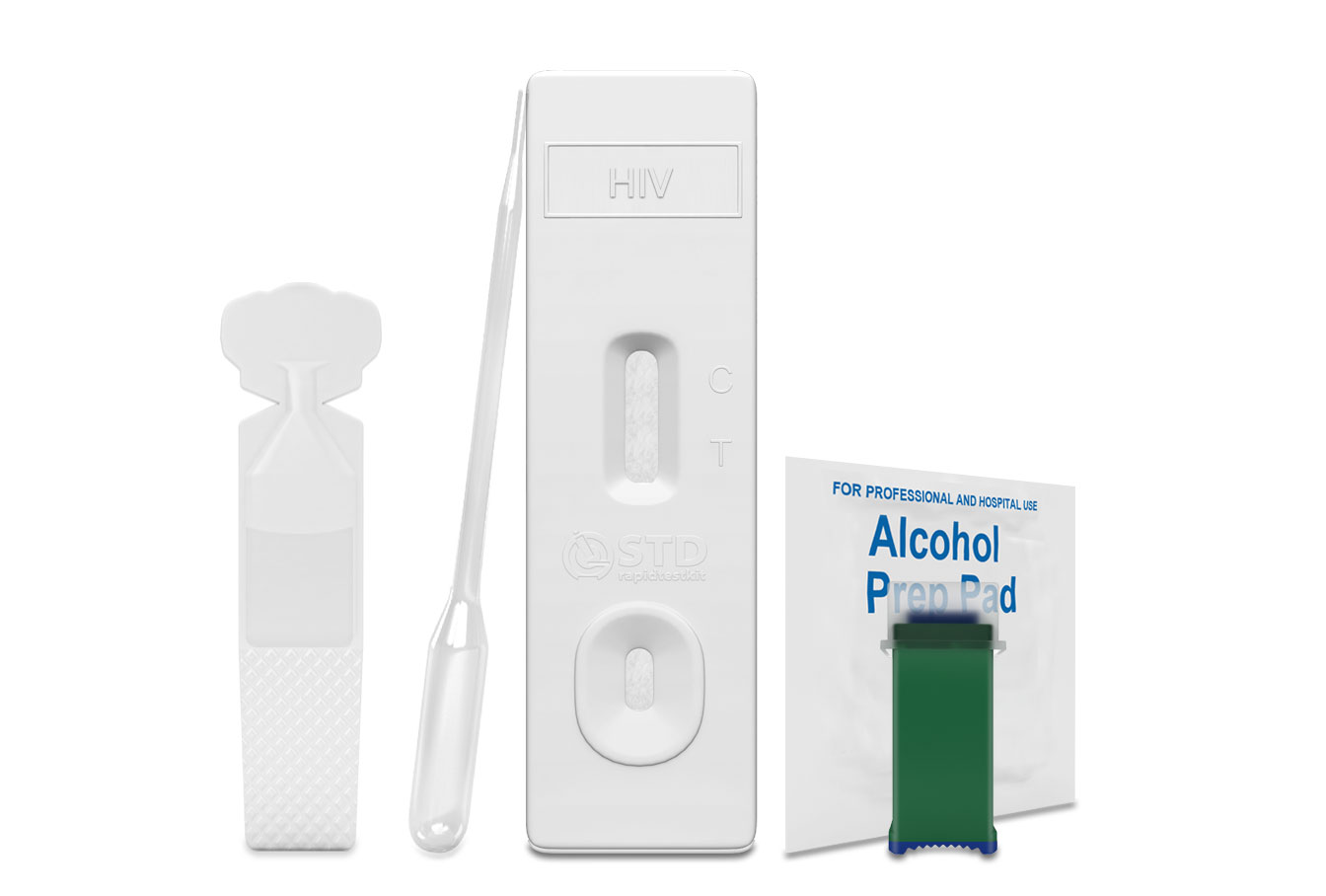
Testing at home isn't just one thing. It's a whole spectrum of technology, from the "instant" kits that look like pregnancy tests to the sophisticated mail-in labs that use the exact same machinery as your local hospital.
✨ Don't miss: Magnesium Side Effects: Why You Might Actually Be Getting Too Much
The Reality of How a Home STD Test Kit Actually Works
There's a common misconception that you just swipe a swab and a light turns green. It’s rarely that simple. Most reputable services, like LetsGetChecked, Everlywell, or Nurx, operate on a "collection at home, processing at lab" model. You order the box, it arrives in discreet packaging—no big red "I HAVE AN STD" stickers on the front—and you follow the instructions. This usually involves a vaginal swab, a urine sample, or a finger-prick blood draw.
The blood part is where people usually get squeamish. You aren’t drawing a vial of blood. It’s a few drops into a tiny tube. But honestly? If you have thick skin or poor circulation, getting enough drops for a valid sample can be a total pain. If you don't fill that tube to the line, the lab might reject it, and then you’ve just wasted seventy bucks and a week of your time.
Once you mail it back using the prepaid envelope, the sample goes to a CLIA-certified lab. This is the gold standard. If a company doesn't mention CLIA (Clinical Laboratory Improvement Amendments) or CAP (College of American Pathologists) accreditation, run the other way. Those certifications mean the lab meets federal standards for accuracy. Without them, you’re basically just guessing.
The Window Period: Why Timing is Everything
This is the part where people mess up most often. If you had an "encounter" on Saturday night and you use a home std test kit on Monday morning, you are almost certainly wasting your money. Most infections have a "window period." This is the time it takes for the pathogen or your body's immune response (antibodies) to reach detectable levels.
For something like Chlamydia or Gonorrhea, you usually need to wait about one to two weeks. HIV? That can take anywhere from a few weeks to a few months depending on the type of test (antigen vs. antibody). If you test too early, you get a "false negative." You think you're in the clear, but you’re actually just in the waiting room of biology. It's frustrating, but biology doesn't care about our anxiety.
Accuracy vs. Convenience
Are they as good as a doctor's visit? Mostly, yes.
A 2021 study published in The Lancet Regional Health highlighted that for common bacterial infections like chlamydia and gonorrhea, the sensitivity of home-collected samples is remarkably high—often over 90-95%. The tech behind Nucleic Acid Amplification Tests (NAAT) is incredibly sensitive. It looks for the DNA of the bacteria. It doesn't need a massive colony to find it; it just needs a trace.
However, the "human factor" is the weak link. When a nurse takes your blood, they know what they’re doing. When you’re doing it yourself in your bathroom at 11 PM, you might contaminate the swab or not use enough buffer liquid. This is why some doctors still prefer in-person visits. They want to ensure the sample is pristine.
What about the "Rapid" kits?
You might see "Rapid HIV" or "Rapid Syphilis" tests that give results in 15 minutes. The OraQuick In-Home HIV Test is the only FDA-approved rapid HIV test for home use. It’s a mouth swab. It’s great for peace of mind, but it has a slightly higher rate of false negatives than a blood draw because antibody levels in oral fluid are lower than in blood. If you get a positive on a rapid kit, you must follow up with a lab-based blood test. No exceptions.
The Privacy Trade-off
Privacy is the big selling point. But "private" doesn't mean "anonymous."
Legally, STD results are "reportable conditions." This means if you test positive for something like Syphilis or HIV, the lab is required by law to report that finding to the local or state health department. This happens whether you go to a fancy clinic or use a home std test kit. The health department uses this data for tracking outbreaks and, in some cases, for partner notification services.
Also, consider your data. When you sign up for these apps, you’re handing over your name, address, and health status to a private company. Most of these companies, like CVS Health or Ro, have robust privacy policies, but in the era of data breaches, it's something to keep in the back of your mind.
The Cost Factor: Out of Pocket vs. Insurance
Most home kits are not covered by insurance upfront. You’re looking at anywhere from $45 for a single-condition test to $250 for a "complete" panel that checks for 10+ different things.
✨ Don't miss: Pelvic floor muscle stimulator: Why your Kegels aren't working and what actually helps
- LetsGetChecked usually hits around the $99 mark for a basic 3-test panel.
- Everlywell is similar, often offering subscription models (which feels a bit weird for STD testing, but hey, if you’re active, it might make sense).
- myLAB Box offers some of the most comprehensive panels, including things like Trichomoniasis and Mycoplasma genitalium.
If you have an HSA (Health Savings Account) or FSA (Flexible Spending Account), you can usually use those funds to pay for the kit. That’s a huge plus. But if you're broke and need a test, your local Planned Parenthood or county health clinic might still be the better option, as they often scale fees based on income—sometimes even making it free.
When You Should Skip the Home Kit
Don't buy a kit if you actually have symptoms.
If you're experiencing pain, unusual discharge, or sores, you shouldn't wait for a box to arrive in the mail and then wait another five days for lab results. You need a physical exam. A doctor can look at things a swab can't—like pelvic inflammatory disease (PID) or other complications.
Also, if you think you were exposed to HIV in the last 72 hours, a test kit is useless. You need PEP (Post-Exposure Prophylaxis), which is a round of emergency meds that can prevent infection. You can only get that from an ER or an urgent care clinic.
Navigating the Results
So, the email hits your inbox. "Your results are ready." Your heart does a little jump.
If it’s negative: Great. But remember that window period. If you had a risky encounter yesterday, this negative result just tells you about your status from a few weeks ago.
If it’s positive: Don't panic. Most things these kits find are easily curable with a round of antibiotics. Many of the top-tier home test companies now include a "telehealth" component. If you test positive for Chlamydia or Gonorrhea, they can often have a doctor call you and send a prescription directly to your local pharmacy. This is a game-changer. It completes the loop without you ever having to walk into a clinic.
However, for things like Herpes (HSV-2), it's more complicated. Blood tests for Herpes are notoriously finicky and can show "false positives" if the levels (IgG index) are low. Many doctors actually recommend against testing for Herpes if you don't have symptoms because the psychological stress of a "maybe" positive often outweighs the clinical benefit.
Practical Steps for Staying Safe
Testing is just one part of the puzzle. It’s a snapshot in time.
- Check the Expiration: These kits have chemicals and buffers that expire. Don't use a kit that's been sitting in your bathroom cabinet since 2023.
- Follow the Instructions Exactly: If it says "first morning urine," it means it. The concentration of DNA is highest then. If you've been chugging water all day, your sample might be too dilute.
- Talk to Your Partners: It's a "sorta" awkward conversation, but it's better than the "hey, I have a surprise" conversation later.
- Confirm the Lab: Ensure they use NAAT technology for bacterial tests. It is significantly more accurate than the older "culture" methods.
- Verify Telehealth Support: Before buying, see if they offer a consultation if the result is positive. You don't want to be left holding a positive result with no idea what to do next.
The home std test kit has fundamentally changed how we handle sexual health. It has removed the "shame" barrier for millions of people. While it isn't a perfect replacement for a relationship with a primary care doctor, it is a massive step forward in making healthcare accessible. If the choice is between not testing because you're embarrassed and testing at home—test at home. Every single time.
💡 You might also like: Rice Left Out Overnight: What You Need To Know About Fried Rice Syndrome
Knowledge is power, but only if the data is accurate. Buy from a reputable brand, watch the window period, and if something feels "off" physically, go see a human doctor.
To get started, look for kits that explicitly state they use CLIA-certified labs and offer physician-led follow-up. Check your HSA balance to see if you can cover the cost, and make sure you're at least two weeks out from your last potential exposure to ensure the most accurate reading possible. Once the kit arrives, read the instructions twice before you even open the collection vials—getting it right the first time saves you a lot of headache.