You’ve probably heard the hype. Everyone is telling you to take more Vitamin D. Your doctor, your trainer, that one influencer on TikTok—they all say we’re deficient. And honestly? Most of us are. But there is a point where the "sunshine vitamin" stops being a health hack and starts becoming a legitimate problem. When we talk about high vit d levels, we aren't just talking about a number on a lab report; we’re talking about a physiological tipping point that can mess with your heart and your kidneys in ways that are hard to reverse.
It’s called hypervitaminosis D. It sounds fancy, but it basically means your body has more than it can handle.
Unlike Vitamin C, which you just pee out if you take too much, Vitamin D is fat-soluble. It sticks around. It builds up in your fat stores like a long-term savings account you can't easily close. If you keep depositing, eventually the bank overflows. And when Vitamin D overflows, it brings a lot of calcium along for the ride. That's where things get messy.
The Calcium Connection: What High Vit D Levels Actually Do to Your Blood
The primary job of Vitamin D is to help your gut absorb calcium. That's great for bones. We love strong bones. But when you have high vit d levels, your body starts absorbing calcium with reckless abandon. It’s like an over-eager vacuum cleaner sucking up everything in sight.
This leads to hypercalcemia.
Suddenly, your blood is swimming in excess calcium. This isn't the "strong teeth" kind of calcium; it's the "clogging up your machinery" kind. This excess mineral starts looking for a place to land. It often chooses your soft tissues. Imagine your arteries, which are supposed to be flexible like rubber hoses, slowly turning into stiff pipes because of calcium deposits. This is known as vascular calcification. It's a significant risk factor for heart disease and it’s a direct consequence of sustained, excessively high levels of the vitamin.
It's not just the heart, either. Your kidneys are the filters. When they have to process blood that is sludge-heavy with calcium, they struggle. This is how you end up with "nephrocalcinosis"—a terrifying term for calcium deposits in the kidney tissue—or just plain, agonizing kidney stones. If you've ever had a kidney stone, you know you'd do almost anything to avoid another one.
The Mayo Clinic Threshold and the "Sweet Spot"
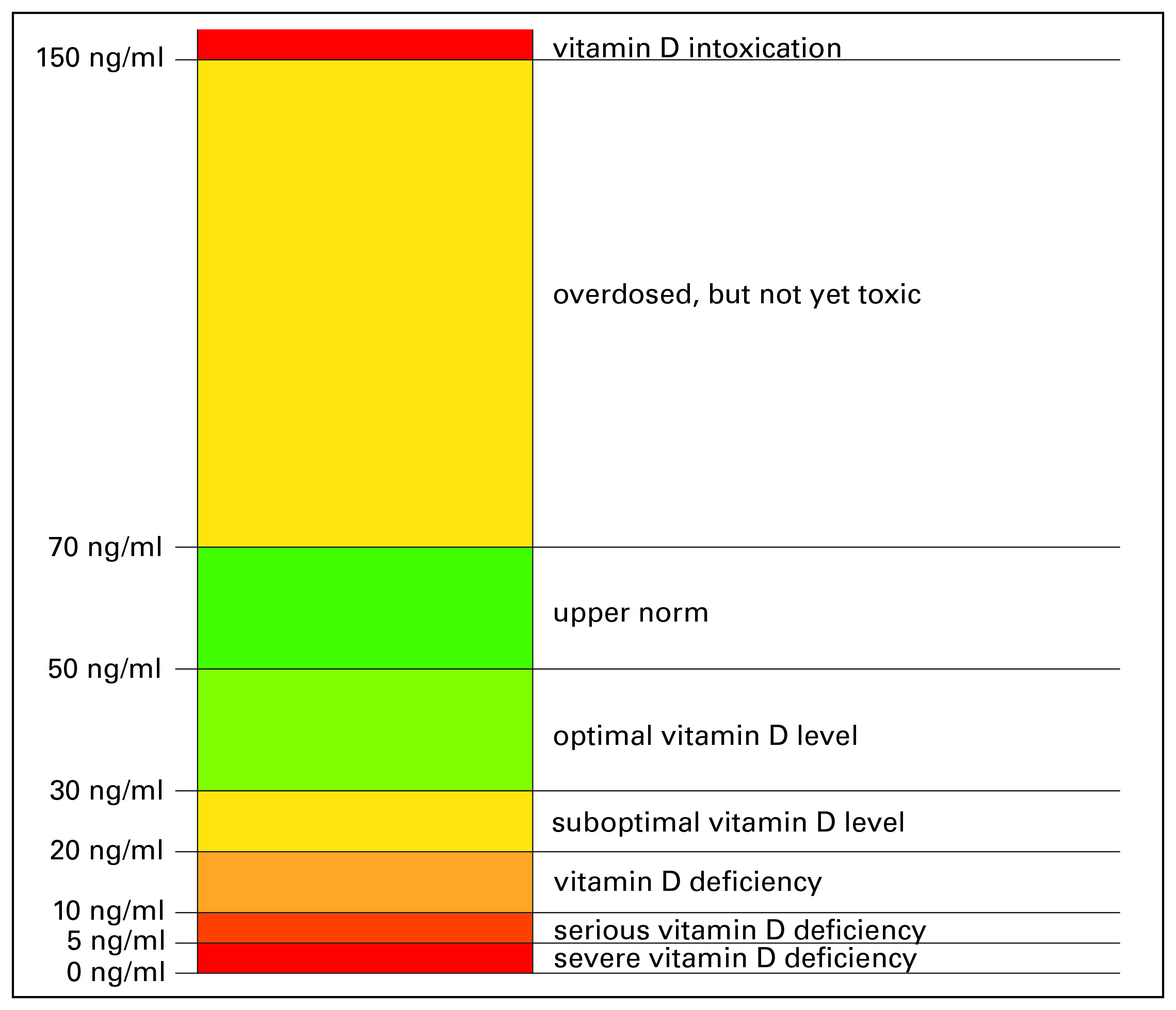
Most labs define a normal range for 25-hydroxyvitamin D as 30 to 100 ng/mL. The Mayo Clinic and other major health institutions generally agree that toxicity rarely occurs below 100 ng/mL, but once you cross that line, you're in the danger zone.
Some "biohackers" aim for 80 or 90 ng/mL, thinking it's optimal performance territory. But the gap between 90 and 150 (where real toxicity symptoms often kick in) is smaller than you think, especially if you’re megadosing with 10,000 IU or 50,000 IU supplements without regular blood work.
Signs You've Crossed the Line
How do you know if you've overdone it? It’s tricky. The symptoms of high vit d levels are frustratingly vague at first. You might just feel "off."
- Brain Fog and Fatigue: You feel like you're moving through molasses.
- Digestive Chaos: Nausea, vomiting, and stomach pain are classic signs of hypercalcemia.
- Excessive Thirst: Because your kidneys are trying to flush the excess calcium, you're constantly thirsty and running to the bathroom.
- Bone Pain: Ironically, the vitamin meant to help bones can cause deep, aching pain when levels are toxic.
I once spoke with a patient who had been taking "super-supplements" he found online. He thought his fatigue was a sign he needed more Vitamin D. By the time he got a blood test, his levels were over 200 ng/mL. He wasn't just tired; he was on the verge of kidney failure. He had to stop all supplements and stay out of the sun for months to let his body reset.
The Role of Vitamin K2
We can't talk about Vitamin D toxicity without mentioning Vitamin K2. They are partners. If D is the usher that brings calcium into the building, K2 is the security guard that tells the calcium exactly where to sit (in the bones and teeth). Without enough K2, the calcium wanders into the hallways (the arteries). Many experts, like Dr. Kate Rhéaume-Bleue, argue that many "Vitamin D problems" are actually Vitamin K2 deficiencies. If you’re pushing for higher D levels, your K2 needs to keep up.
💡 You might also like: Writing a sober letter to drunk self: Why it works and how to actually do it
Why Do We Get It Wrong?
The supplement industry is a bit of a Wild West. You can buy 10,000 IU capsules over the counter, even though the Recommended Dietary Allowance (RDA) for most adults is only 600–800 IU. While the RDA is arguably too low for many, jumping to 10k every day without a deficiency is a recipe for trouble.
Genetic factors also play a massive role. Some people have variations in the CYP24A1 gene. This gene is responsible for breaking down Vitamin D. If yours is sluggish, you will reach high vit d levels much faster than the average person. It’s not a one-size-fits-all situation.
Then there’s the "loading dose" trend. Some doctors prescribe 50,000 IU once a week for people with severe deficiencies. This is fine under medical supervision. But people see that number and think, "Hey, if my doctor gave me that once, I should just take it all the time." That is exactly how toxicity happens. It’s a slow creep.
Real-World Risks: The Kidney Factor
Your kidneys are incredibly resilient, but they have their limits. Chronic hypercalcemia from high vit d levels can cause "calcium phosphate" to precipitate in the renal tubules. This is physical damage. It’s like putting sand in an engine. Over time, this leads to decreased kidney function or chronic kidney disease (CKD).
A study published in the American Journal of Medicine documented cases of individuals developing acute kidney injury after taking incorrectly formulated supplements that contained way more Vitamin D than the label claimed. Quality control matters. If you're buying the cheapest bottle on the shelf from a brand you've never heard of, you're taking a gamble with your filtration system.
Actionable Steps for Balancing Your Levels
Don't panic and throw your supplements in the trash. Vitamin D is still essential for immune function and mental health. You just need to be smart about it.
🔗 Read more: Why The Business of Being Born Still Matters Almost Two Decades Later
1. Get a baseline 25(OH)D test. Do not supplement blindly. You need to know where you are starting. If you're at 45 ng/mL, you probably don't need a high-dose supplement. If you're at 12, you do.
2. Test every 3 to 6 months if you're supplementing. Levels change. As you lose weight (Vitamin D is stored in fat) or change your diet, your requirements shift. Regular testing prevents the "slow creep" into toxicity.
3. Prioritize food and sun. It is almost impossible to get toxic levels of Vitamin D from the sun. Your skin has a built-in "off switch" where it stops producing the vitamin once you've had enough. Fatty fish like salmon and egg yolks provide D in a matrix of other nutrients that your body understands.
4. Watch your magnesium and K2 levels. Vitamin D requires magnesium to be converted into its active form. If you take tons of D, you can actually deplete your magnesium stores, leading to cramps and anxiety. Ensure you're getting enough of these co-factors to keep the system balanced.
5. Check your labels for "UI" vs "mcg." Some labels are confusing. 400 IU is 10 mcg. 1,000 IU is 25 mcg. Make sure you aren't misreading the dosage and taking ten times more than you intended.
The goal isn't to have the "highest" score on your lab report. It’s to stay in the functional range where your immune system is supported, but your heart and kidneys aren't being calcified. Balance is boring, but it's what keeps you out of the hospital. If you suspect your levels are too high, stop the supplements immediately and speak to a healthcare provider about a comprehensive metabolic panel to check your calcium and kidney function.