You’re sitting in the doctor’s office. The cuff tightens. It keeps tightening until your arm pulses. Then, the hiss of air. The nurse mutters two numbers. Usually, we only focus on the first one—that high top number on blood pressure that makes everyone look a bit concerned.
It’s called systolic pressure.
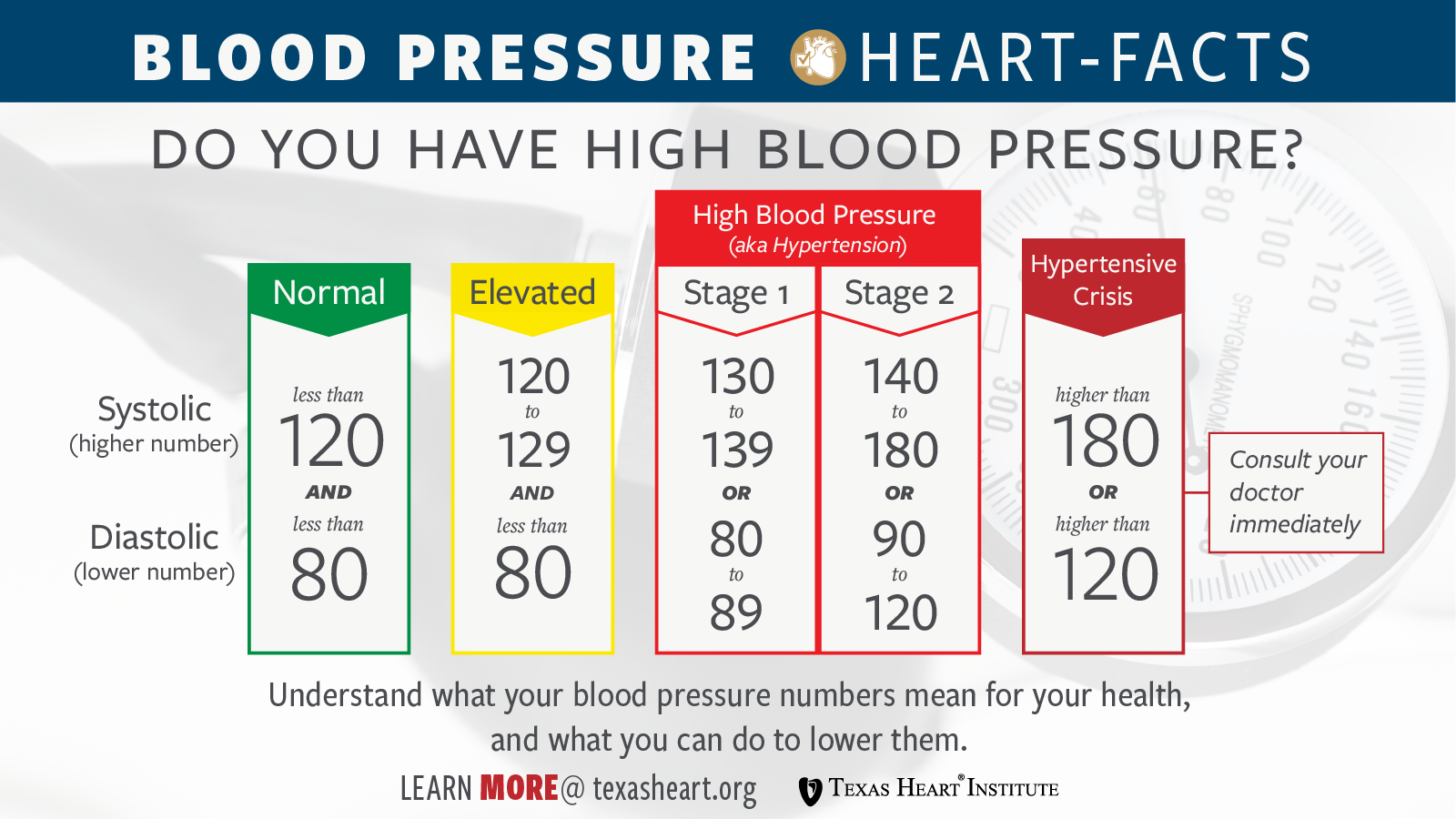
Honestly, most of us just see it as a "score." If it’s under 120, you win. If it’s over 140, you’re stressed. But that number isn’t just a digit on a screen; it’s a physical measurement of the force your heart exerts against your artery walls every single time it beats. When that top number climbs, it’s basically telling you that your pipes are under too much pressure. Over time, things start to leak or burst.
Why the High Top Number on Blood Pressure Is Usually the One to Watch
For a long time, doctors went back and forth on which number mattered more. The bottom number (diastolic) represents the pressure when your heart is resting between beats. It’s important, sure. But for most adults—especially those of us over 50—the systolic reading is the real crystal ball for cardiovascular risk.
Why? Because it reflects the "stiffness" of your major arteries.
As we age, our blood vessels lose their stretch. They get brittle. Think of an old garden hose left out in the sun for three summers. When you turn the water on full blast, that hose doesn't expand to accommodate the flow; instead, the pressure inside skyrockets. That is exactly what happens in your body. This phenomenon is often called Isolated Systolic Hypertension. You might have a perfectly normal bottom number, but a high top number on blood pressure that’s pushing 150.
Don't ignore it just because the bottom number looks fine.
The Framingham Heart Study Connection
The famous Framingham Heart Study, which has been tracking heart health across generations since 1948, really hammered this home. Researchers found that as people age, the systolic number becomes a much more potent predictor of strokes and heart attacks than the diastolic number.
👉 See also: Nuts Are Keto Friendly (Usually), But These 3 Mistakes Will Kick You Out Of Ketosis
Basically, your heart is working too hard to move blood through a rigid system.
What Is Causing That Spike?
It’s rarely just one thing. Life is messy, and so is biology.
Sometimes it’s just genetics. You could be a marathon runner who eats nothing but kale and still have a high top number because your DNA decided your arteries would be less elastic. But more often, it’s a combination of the "usual suspects" that we all know but hate to address.
Salt is a big one. Not just the salt you shake onto your eggs. It’s the hidden sodium in bread, canned soups, and "healthy" frozen dinners. Sodium pulls water into your bloodstream. More water means more volume. More volume means higher pressure. It’s simple physics, really.
Then there’s the "White Coat" effect.
I’ve seen people whose blood pressure jumps 20 points the second they see a stethoscope. Their brain perceives the medical environment as a threat, triggers the sympathetic nervous system, and boom—the heart pumps harder, narrowing the vessels. If your top number is only high at the clinic, you might not actually have hypertension. You might just have a very reactive nervous system. This is why many cardiologists, like those at the Mayo Clinic, now insist on home monitoring or 24-hour ambulatory checks before prescribing meds.
Stress and the "Stiffening" Factor
Chronic stress doesn't just make you grumpy. It keeps your body bathed in cortisol and adrenaline. These hormones are great if you're being chased by a predator, but if they’re elevated because of a spreadsheet or a traffic jam, they keep your arteries constricted. Over years, this constant constriction leads to structural changes in the vessel walls. They thicken. They stiffen. And that high top number on blood pressure becomes your new, dangerous baseline.
✨ Don't miss: That Time a Doctor With Measles Treating Kids Sparked a Massive Health Crisis
The SPRINT Trial: Why 120 Is the New 140
For years, the "safe" threshold for the top number was 140. If you were 135, your doctor might just tell you to lose a few pounds and check back in six months.
Then came the SPRINT trial (Systolic Blood Pressure Intervention Trial).
This was a massive study funded by the National Institutes of Health. It looked at over 9,000 adults. They split them into two groups: one aiming for a top number of 140, and another aiming for a much more aggressive 120.
The results were so lopsided that they actually stopped the study early.
The 120 group had significantly lower rates of heart disease and death. This study is the reason why the American Heart Association shifted the guidelines. Now, 130 is considered Stage 1 Hypertension. It’s a lower bar, which means more people are being diagnosed, but the goal is to catch the damage before it becomes irreversible.
Understanding the "Pulse Pressure" Gap
Here is a detail most people miss: the gap between your top and bottom numbers.
If your reading is 150/70, that gap is 80. Doctors call this your pulse pressure. A wide pulse pressure (anything over 60) is often a sign of significant arterial stiffness or even a leaky heart valve (aortic regurgitation).
🔗 Read more: Dr. Sharon Vila Wright: What You Should Know About the Houston OB-GYN
If your top number is high while your bottom number is very low, it actually makes treatment trickier. Doctors have to be careful not to lower the bottom number too far while trying to bring the top one down, because your heart muscle itself needs that diastolic pressure to get its own blood supply. It’s a delicate balancing act.
Real-World Ways to Bring That Number Down
You don't always have to jump straight to pills, though for many, they are literal lifesavers. There are nuanced ways to shift the needle that go beyond "exercise more."
- Potassium is the secret weapon. Most people focus on cutting salt, but increasing potassium is just as vital. Potassium helps your kidneys flush out sodium and actually relaxes the walls of your blood vessels. Bananas are okay, but avocados, spinach, and white beans are absolute powerhouses for this.
- The "Power Nap" Effect. Lack of sleep is a massive, underrated driver of systolic spikes. If you aren't getting into deep REM sleep, your nervous system never fully "resets," keeping your baseline pressure higher the next day.
- Magnesium Supplementation. This isn't medical advice—always talk to your doctor—but many people are deficient in magnesium. Magnesium acts like a natural calcium channel blocker, helping the smooth muscles in your arteries relax.
- Nitric Oxide Foods. Beets and leafy greens contain nitrates that your body converts into nitric oxide. This gas tells your blood vessels to "open up." It’s like a natural vasodilator. Drinking beet juice has been shown in some small trials to drop the top number by several points within hours.
When Is It an Emergency?
We need to talk about the "Hypertensive Crisis."
If that top number hits 180 or higher, you aren't just in the "red zone"—you’re in the danger zone. If that high number is accompanied by a headache, chest pain, or blurred vision, it’s not a "wait and see" situation. That is your body telling you that the pressure is so high it’s starting to damage the organs right now.
Most of the time, high blood pressure is a silent killer because it doesn't feel like anything. You can walk around with a 160 systolic reading for years and feel totally fine. Until you don't.
Actionable Steps for Today
If you’ve seen a high top number on blood pressure lately, don't panic, but do take it seriously.
- Buy a validated home monitor. Look for one that is "cuff-style" for the upper arm. Wrist monitors are notoriously flaky.
- Track it for a week. Take your pressure at the same time every morning and evening. Don't drink coffee or smoke 30 minutes before. Sit still for five minutes first. This "log" is 100x more valuable to a doctor than a single reading in a cold office.
- Watch the "Hidden" Salts. Check the labels on your salad dressings and bread. You’d be shocked how much sodium is in a "healthy" turkey sandwich.
- Breathwork. It sounds "woo-woo," but five minutes of slow, diaphragmatic breathing (6 breaths per minute) can acutely lower systolic pressure by calming the vagus nerve. It’s a physical override for your stress response.
High blood pressure isn't a failure; it’s a biological reality of living in a modern, high-stress, high-sodium world. Understanding that the top number is a reflection of your arterial health gives you the power to actually change the narrative before it becomes a chronic problem.
Next Steps:
Check your blood pressure tomorrow morning before you have your first cup of coffee. Record that number. If it’s consistently over 130, schedule a baseline checkup with a provider to discuss a long-term strategy for arterial elasticity, focusing specifically on your sodium-to-potassium ratio and sleep hygiene.