You’re sitting in the doctor’s office. The cuff tightens. You hear that rhythmic whoosh-whoosh in the stethoscope, and then the numbers pop up on the screen. 120 over 95. The doctor frowns a little. You know the top number—the systolic—is fine. It’s perfect, actually. But that bottom number? It’s creeping up. This is high lower number blood pressure, known in medical circles as Isolated Diastolic Hypertension (IDH).
Most people obsess over the top number. We’ve been conditioned to think the systolic is the "important" one because it represents the force of your heart pumping. But the diastolic, that bottom number, represents the pressure in your arteries when your heart is resting between beats. If that pressure stays high, your blood vessels never get a break. They’re under constant tension. It’s kinda like keeping a garden hose turned on full blast even when you aren't spraying anything. Over time, things start to leak or burst.
Honestly, for a long time, many physicians didn't treat IDH as aggressively as they did "standard" hypertension. But new data is changing that perspective.
What High Lower Number Blood Pressure Actually Means
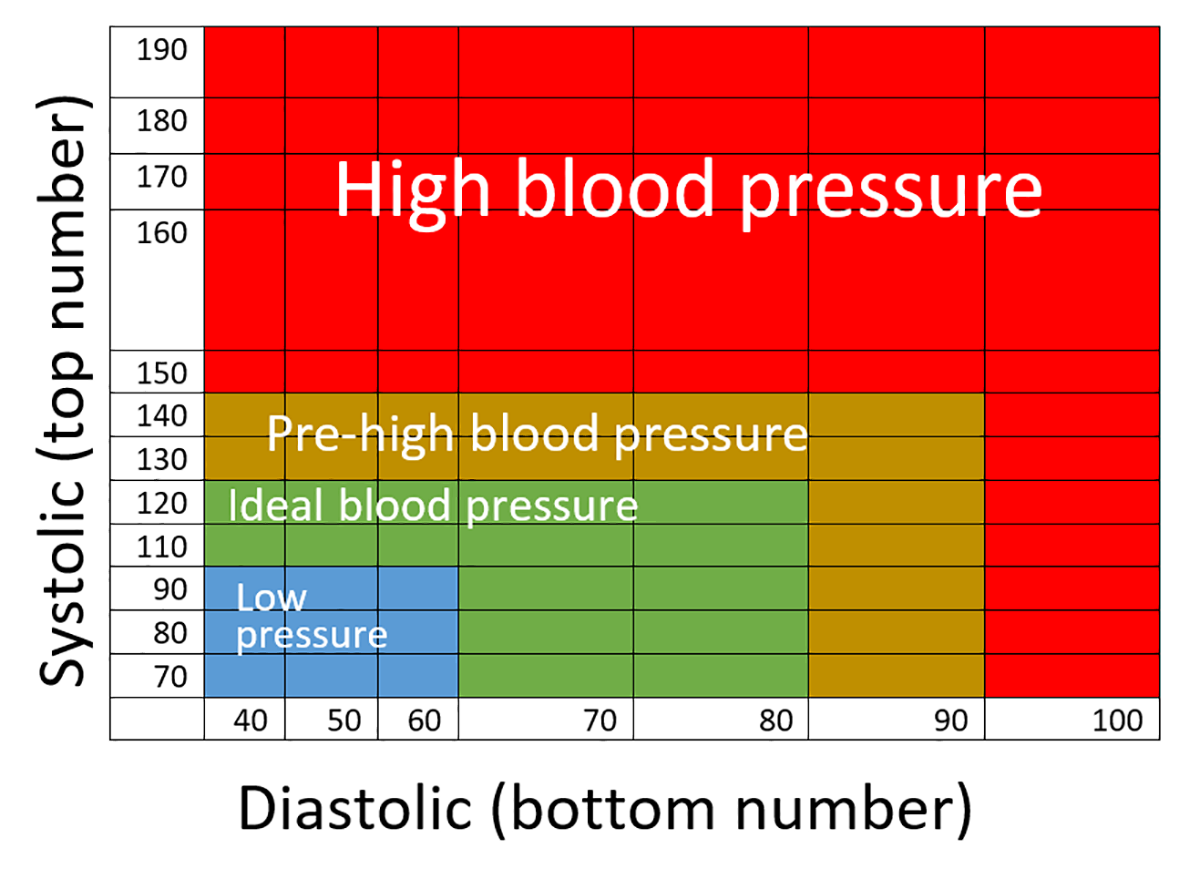
The diastolic pressure is the "baseline" tension in your circulatory system. When it’s high—specifically 80 mmHg or higher according to the American Heart Association—it suggests that your small blood vessels (arterioles) are constricted.
Why does this happen? Usually, it's about resistance.
Your heart is a pump. If the pipes it’s pumping into are narrow or stiff, the pressure stays high even when the pump isn't actively pushing. This is particularly common in younger adults, often those under 50. While older adults tend to see their systolic pressure climb as their large arteries stiffen with age, younger people often struggle with this isolated diastolic spike.
It’s sneaky. You might feel totally fine. No headaches. No blurry vision. Just a number on a screen that won't behave.
📖 Related: How to Hit Rear Delts with Dumbbells: Why Your Back Is Stealing the Gains
The Myth of the "Safe" High Bottom Number
There’s a dangerous idea floating around that as long as the top number is low, you’re in the clear. That's simply not true. Research published in the Journal of the American College of Cardiology has indicated that while systolic pressure is a better predictor of overall cardiovascular risk in older populations, high diastolic pressure is a significant red flag for younger people.
If you're 35 and your diastolic is consistently 92, you’re putting a decade of unnecessary wear and tear on your heart muscle. The heart has to work harder to "overcome" that baseline pressure just to get blood moving. This can lead to left ventricular hypertrophy—basically, the heart muscle gets thick and stiff, like a bodybuilder who can’t move their arms properly anymore. It’s not a good look for an internal organ.
Why Your Diastolic Number Is High (And Others Aren't)
It isn't always about salt. Sure, salt matters, but high lower number blood pressure is often a lifestyle "check engine" light.
One of the biggest culprits? Alcohol.
You might think a couple of beers helps you relax, but ethanol is a vasoconstrictor in the long term. It messes with the way your kidneys handle fluids and how your nervous system regulates vessel tone. If you're a "weekend warrior" with the drinks, don't be surprised if your Monday morning blood pressure reading shows a bottom number in the 90s.
Then there’s sleep apnea. This is a big one. If you snore or stop breathing in your sleep, your body panics. It releases a surge of adrenaline to wake you up so you don't, well, die. That adrenaline spike tightens your blood vessels. Even after you wake up, that "tightness" can linger throughout the day, manifesting as a high diastolic reading.
👉 See also: How to get over a sore throat fast: What actually works when your neck feels like glass
- Stress and the Sympathetic Nervous System: If you’re constantly in "fight or flight" mode, your body keeps your vessels constricted.
- Weight Distribution: Specifically, visceral fat—the stuff around your organs—secretes inflammatory markers that stiffen the smaller vessels.
- Sedentary Behavior: If you sit at a desk for 10 hours, your circulation gets sluggish, and the vessels lose their "stretchiness."
The "White Coat" Factor
We have to talk about anxiety. Some people only have high lower number blood pressure when they see a doctor. This is "White Coat Hypertension." Your nervous system sees the white coat and reacts by tightening up.
To find out if your high diastolic is real or just a "stage fright" reaction, you need a home monitor. Take your pressure at 7:00 AM and 7:00 PM for a week. Throw out the first day’s results (everyone is nervous on day one). Average the rest. If that bottom number is still over 80, it’s not the doctor—it’s you.
The Long-Term Stakes: It's Not Just About Your Heart
When we talk about high lower number blood pressure, we usually focus on heart attacks. But your brain cares just as much.
Recent longitudinal studies have looked at the link between mid-life diastolic hypertension and late-life cognitive decline. Because the diastolic pressure affects the smallest vessels—the ones deep in your brain—it can cause "micro-bleeds" or "silent strokes." You won't notice them when they happen. But twenty years later, they contribute to vascular dementia.
It’s also the leading cause of kidney strain. The kidneys are essentially a massive bundle of tiny filters. High diastolic pressure beats up those filters 24/7. Once the filters are scarred, they can't be fixed.
Real-World Strategies to Bring That Number Down
So, what do you actually do? You don't necessarily need a pharmacy's worth of pills immediately, especially if your systolic is still normal.
✨ Don't miss: How Much Should a 5 7 Man Weigh? The Honest Truth About BMI and Body Composition
First, look at your potassium. Most people focus on cutting salt, which is fine, but increasing potassium is often more effective for the diastolic number. Potassium helps the walls of your blood vessels relax. It’s like a natural "undo" button for the constriction caused by salt. Bananas are okay, but avocados, spinach, and white beans are the real heavy hitters.
Second, grip strength exercises. This sounds weird. It sounds like bro-science. But it’s actually backed by clinical trials. Using an isometric grip trainer—basically squeezing a spring-loaded handle for a few minutes a day—has been shown to lower diastolic pressure significantly. It triggers a reflex that tells your entire vascular system to relax.
- Magnesium Supplementation: Many people are deficient. Magnesium acts as a natural calcium channel blocker, helping vessel walls stay supple.
- Zone 2 Cardio: This isn't sprinting. It’s a slow, boring jog or a fast walk where you can still hold a conversation. It improves the "compliance" (the bounce) of your arteries.
- Cutting Liquid Carbs: Sugar spikes insulin, and insulin tells your kidneys to hold onto sodium. That extra sodium keeps the pressure high.
When to Talk to a Professional
If you’ve tried the lifestyle stuff for three months and that lower number is still stuck at 90 or above, it’s time for a real medical intervention.
Sometimes, genetics just win. You can be a marathon-running vegan and still have high lower number blood pressure because your receptors are just wired "tight." In these cases, low-dose medications like ACE inhibitors or ARBs are often used. These drugs specifically target the hormones that cause vessel constriction. They aren't "failures" on your part; they are tools to prevent your 60-year-old self from having a stroke.
Actionable Steps for Today
Don't panic, but don't ignore it. Start here:
- Buy an upper-arm monitor. Wrist monitors are notoriously inaccurate for diastolic readings because of the way the bones in the wrist interfere with the sensor.
- Test your "resting" state. Sit quietly for five minutes before taking a reading. No phone. No TV. No talking. If you take it right after walking up stairs, the number is meaningless.
- Audit your caffeine. If you’re drinking four cups of coffee, that bottom number will stay elevated. Try cutting back to one and see what happens to your 2:00 PM reading.
- Check your waist-to-height ratio. If your waist is more than half your height, that visceral fat is likely driving your diastolic pressure up through inflammatory signaling.
- Focus on "Deep Work" breathing. Slow, diaphragmatic breathing for 10 minutes a day can reset the autonomic nervous system, lowering the baseline tension in your vessels.
High lower number blood pressure is a warning. It’s your body’s way of saying the system is under constant tension. Addressing it now is significantly easier than dealing with the structural damage it causes a decade down the line. Keep the top number where it is, but give that bottom number the attention it deserves. Your future self will thank you for the lack of "wear and tear."