Ever felt that strange, foggy "slump" after a massive pasta dinner? Or maybe you've noticed you’re suddenly thirsty enough to drink a lake, even though you haven't been hitting the gym. Honestly, most of us just shrug it off. We call it a food coma. We blame the salt. But usually, it’s just your blood sugar spiking. When we talk about the effects of high glucose levels, we aren't just talking about a temporary energy crash. We are talking about a systemic chemical event that touches almost every organ you own. It's complex. It’s kinda scary if you ignore it, but it’s also something you can actually wrap your head around once you stop looking at it as just "a number on a lab test."
Blood sugar—or glucose—is your body’s primary fuel. It’s the gasoline. But imagine pumping high-octane racing fuel into a lawnmower engine for ten years straight. Something is going to melt. That’s basically what hyperglycemia does to your vasculature and nerves.
Why High Glucose Levels Mess With Your Head (Literally)
Your brain is a glucose hog. It uses about 20% of your body's total energy. But it doesn't have a "storage tank" for fuel. It depends on a steady, metered stream. When you experience the effects of high glucose levels, that stream becomes a flood.
According to research from Harvard Medical School, chronic high sugar actually changes the brain's functional connectivity. It’s not just "brain fog." It’s structural. People often report feeling irritable or "snappy." That’s because the brain is struggling to process the excess. You might find yourself staring at a spreadsheet for twenty minutes without processing a single row. This isn't laziness. It’s neurochemistry.
Then there’s the mood aspect. The "sugar high" is a bit of a myth in adults, but the "sugar low" or the inflammatory state caused by high peaks is very real. Over time, this can lead to an increased risk of cognitive decline. Dr. Mary DeMay and other geriatric specialists have often pointed toward "Type 3 Diabetes"—a term some use to describe how Alzheimer's might be linked to insulin resistance in the brain. It’s a sobering thought.
The Sticky Blood Problem
Think about maple syrup. Now think about water.
✨ Don't miss: Inside a Female Body: Why Everything You Learned in Health Class Was Probably Too Simple
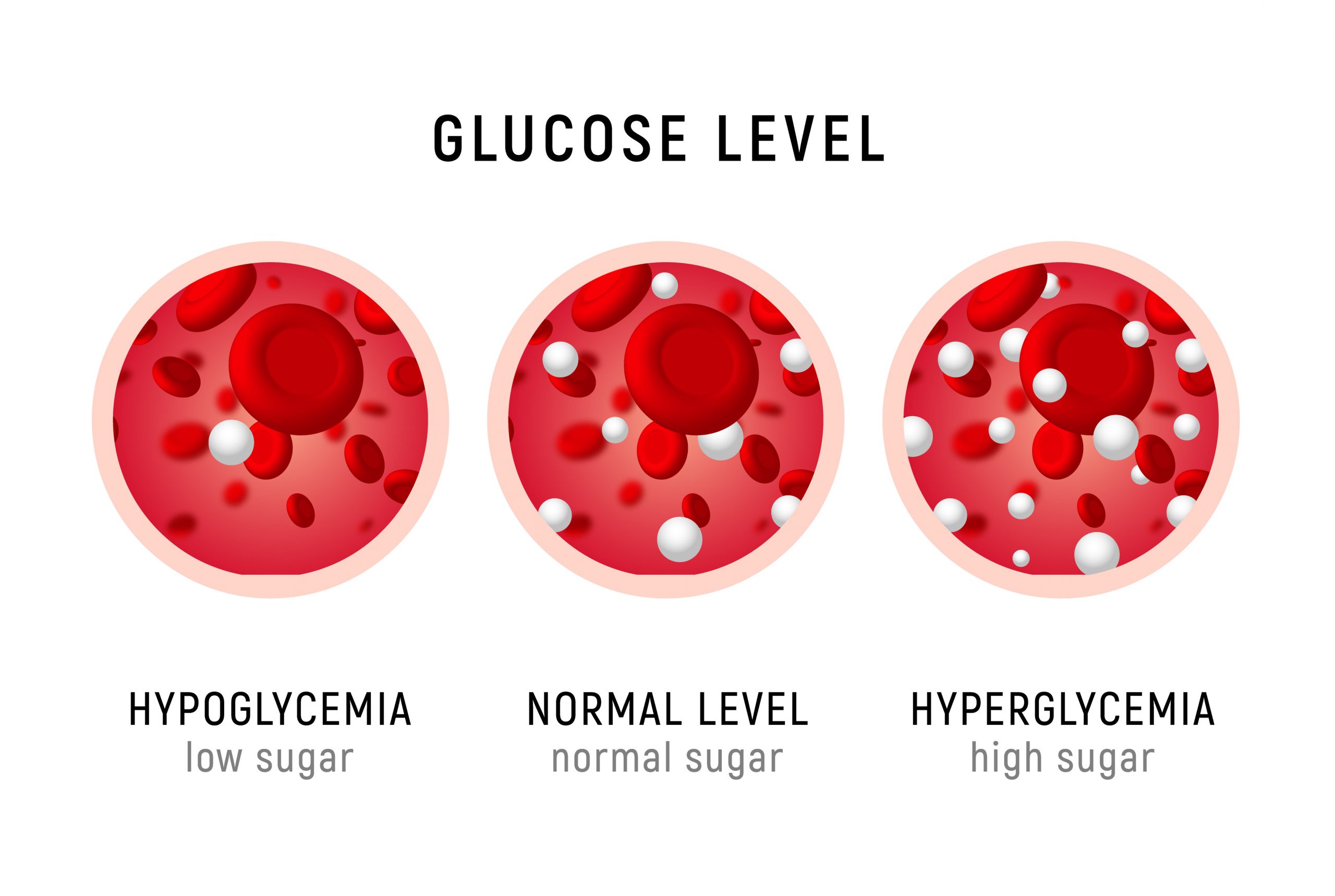
When your glucose levels are high, your blood becomes more viscous. It’s "stickier." This is a nightmare for your smallest blood vessels—the capillaries. These tiny tubes are so narrow that red blood cells sometimes have to line up in single file to pass through. When the blood is thick with sugar, it doesn't flow right.
This leads to the "starvation in the midst of plenty" paradox. Your blood is full of energy (glucose), but it can't get that energy into the cells because the delivery system is jammed.
What your kidneys are trying to tell you
If you find yourself waking up three times a night to pee, that’s your kidneys screaming for help. They are trying to filter that excess sugar out of your blood and dump it into your urine. But glucose pulls water with it.
- You pee more.
- You get dehydrated.
- You drink more water.
- The cycle repeats.
It’s an exhausting loop. This is why "unquenchable thirst" is the classic red flag for high glucose. If you're drinking gallons and your mouth still feels like it's full of cotton balls, your glucose is likely redlining.
The Damage to Your "Wiring"
Neuropathy is a fancy word for nerve damage, and it’s one of the most common long-term effects of high glucose levels. Usually, it starts in the feet. Why? Because those are the longest nerves in your body. They have the furthest to go, and they are the first to lose their "supply line" when blood flow gets restricted.
It starts as a tingle. Kinda like pins and needles.
Then it might turn into a burn.
Eventually, it can turn into nothing—numbness.
Numbness is actually worse than pain. If you can't feel your feet, you won't feel a blister or a pebble in your shoe. That small sore doesn't heal because—remember the sticky blood?—the circulation is too poor to bring healing white blood cells to the area. This is how minor issues turn into "diabetic foot ulcers." It’s a cascading failure.
Your Heart and the "Invisible Scars"
High glucose is like pouring sand into a delicate engine. It causes oxidative stress. This stress creates tiny, microscopic tears in the lining of your arteries (the endothelium).
Your body tries to fix these tears. It uses cholesterol as a sort of "spackle" to patch the holes. But when your glucose stays high, the tearing continues, and the patching continues. Eventually, you have a pipe that’s more "patch" than "pipe." This is atherosclerosis.
It’s why heart disease is so closely linked to blood sugar management. You aren't just dealing with a "sugar problem"; you're dealing with a plumbing problem. Cardiologists like Dr. Ethan Weiss have pointed out that even "pre-diabetic" levels can start this inflammatory process. You don't need a formal diagnosis to start feeling the impact on your cardiovascular system.
The Myth of the "Quick Fix"
A lot of people think they can just "walk off" a massive sugar spike. While exercise is the best way to sensitize your muscles to insulin, it’s not a magic eraser. If your glucose is already dangerously high—say, over 240 mg/dL—exercising can sometimes actually make it rise because your body perceives the activity as stress and dumps even more stored glucose from the liver.
It’s a delicate balance.
We also need to talk about "The Dawn Phenomenon." Have you ever noticed your blood sugar is high in the morning, even though you didn't eat anything all night? It feels like a betrayal. But it’s just your liver doing its job. Around 3:00 AM to 8:00 AM, your body pumps out cortisol and growth hormones to gear you up for the day. This triggers the liver to release glucose for energy. If your insulin isn't keeping up, you wake up with a high reading.
How to Actually Move the Needle
Dealing with the effects of high glucose levels isn't about "dieting" in the way we usually think about it. It’s about managing the "area under the curve." You want to avoid the jagged mountain peaks and aim for rolling hills.
💡 You might also like: The Chest and Back Split: Why Training Antagonistic Muscle Groups Actually Works
Stop the "Naked" Carbs
Never eat a slice of bread alone. Honestly. If you're going to have carbs, "dress" them. Add fat, fiber, or protein. This slows down gastric emptying. The glucose enters your bloodstream like a slow trickle rather than a flash flood. A piece of toast is a spike; a piece of toast with avocado and an egg is a slow burn.
The Power of the 10-Minute Walk
You don't need to run a marathon. A ten-minute walk after your largest meal of the day can significantly blunt a glucose spike. Your muscles use that sugar for fuel immediately. It’s the most underutilized tool in the health shed.
Vinegar? Actually, yes.
It sounds like old wives' tale territory, but studies (like those published in Diabetes Care) suggest that consuming a tablespoon of apple cider vinegar in water before a carb-heavy meal can improve insulin sensitivity. It’s not a miracle cure, but it’s a measurable nudge in the right direction.
Get Brutally Honest with Sleep
Sleep deprivation is a fast track to high glucose. When you’re tired, your cortisol is high. High cortisol tells your body to keep glucose levels elevated for "emergencies." One night of bad sleep can make you as insulin resistant as someone with Type 2 diabetes the next morning. It’s that dramatic.
Actionable Steps for Today
If you suspect your levels are consistently high, don't just guess. Data is your friend here.
- Get a CGM if you can. Continuous Glucose Monitors aren't just for people on insulin anymore. Seeing how a "healthy" oatmeal bowl spikes your sugar to 180 mg/dL is a wake-up call that a standard finger prick might miss.
- Test your A1c. This gives you a three-month average. It’s the "big picture" view. Anything above 5.7% is a signal that your body is struggling to keep up with the load.
- Prioritize Muscle. Muscle is your "glucose sink." The more lean muscle mass you have, the more places your body has to store glucose without needing a massive insulin response. Strength training is metabolic medicine.
- Hydrate, but with electrolytes. If you're flushing out sugar, you're flushing out minerals too. Water alone isn't always enough to fix the cellular dehydration caused by hyperglycemia.
The effects of high glucose levels are often quiet until they aren't. They are "silent" because the body is incredibly good at compensating—until the systems just wear out. Taking control now isn't about restriction; it's about making sure your internal "machinery" doesn't rust out from the inside. Start small. Walk after dinner. Add some protein to your snacks. Your future self—and your kidneys—will thank you.