Ever feel like your brain is running on a battery that just won't hold a charge? Most people think vitamins are just these little things you take to prevent scurvy or something. But for a growing number of people dealing with chronic fatigue, POTS, or Parkinson's, the high dose thiamine protocol isn't just a supplement routine. It’s a total metabolic reboot.
Thiamine is Vitamin B1. Simple, right? Well, not really.
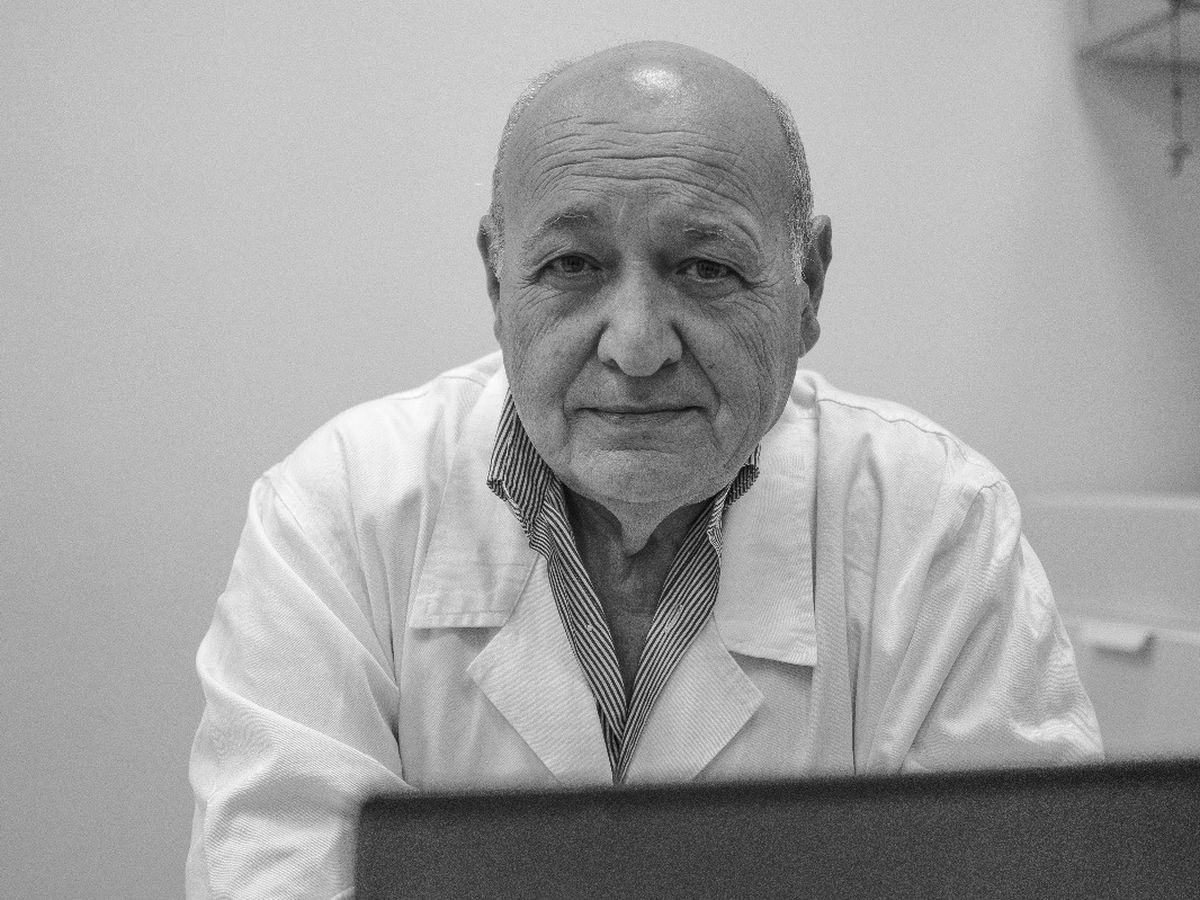
Most doctors will tell you that if you don't have Beriberi, you're fine. They look at a standard blood test, see you’re in the "normal" range, and send you home with a shrug. But there’s a massive difference between "not dying of a deficiency" and having enough cellular energy to actually function. This is where the work of the late Dr. Costantini and researchers like Dr. Derrick Lonsdale comes in. They realized that some people have what’s called "high-demand" states or genetic kinks where they need massive, almost pharmacological doses of B1 to get their mitochondria to actually fire up.
The Science Behind Why Standard Doses Fail
You’ve probably seen the RDA (Recommended Dietary Allowance) for B1. It's tiny. We're talking 1.1 to 1.2 milligrams. That's enough to keep your heart from failing, sure. But B1 is the literal gatekeeper of the Krebs cycle. If you don't have enough thiamine, your body can't turn glucose into ATP efficiently. Instead, you end up with a backup of pyruvate and lactate. You feel heavy. You feel "brain fogged."
Honestly, it’s like trying to run a high-performance engine through a coffee stirrer.
The high dose thiamine protocol pushes past the standard absorption limits of the gut. See, the body has these transporters (THTR-1 and THTR-2) that carry B1 into your cells. In many people with chronic illness, these transporters are either broken or just plain overwhelmed. By using massive doses—sometimes 500mg, 1000mg, or even 4000mg—you're essentially using "passive diffusion" to force the vitamin into the cells where it's needed most.
Not All B1 is Created Equal
If you walk into a drugstore, you’ll find Thiamine Hydrochloride (HCL). It’s cheap. It works for some. But if you're serious about a high dose thiamine protocol, you need to know about the different "flavors" of B1.
First, there’s Benfontiamine. It’s fat-soluble. Sorta. It’s great for peripheral neuropathy and blood sugar issues because it stays in the blood longer. Then there’s TTFD (Thiamine Tetrahydrofurfuryl Disulfide). This is the heavy hitter. TTFD is truly fat-soluble and can cross the blood-brain barrier without needing those broken transporters we talked about. Dr. Lonsdale often pointed to TTFD as the key for neurological issues because it actually gets into the brain tissue.
Then you have Sulbutiamine, which is more of a "nootropic" version often used for mood and focus.
Which one do you choose? It depends on your symptoms. If it’s brain-based (autonomic dysfunction, anxiety, memory), TTFD is usually the gold standard. If it’s physical fatigue or nerve pain in the legs, Benfontiamine or high-dose HCL might be enough.
The Paradox: Why You Might Feel Worse Before You Feel Better
This is the part that scares people away. It’s called the "Paradoxical Reaction."
You start the high dose thiamine protocol and suddenly, you feel like garbage. Your fatigue gets worse. Your heart races. You might get a headache. Most people think, "Oh, I’m allergic" or "This is toxic."
It’s usually neither.
When you suddenly flood a starved system with the fuel it’s been missing, the metabolic machinery starts "waking up." This creates a temporary surge in oxidative stress and shifts in electrolytes. It’s a sign that the thiamine is actually working, but your body is struggling to keep up with the new energy production. Dr. Costantini noted that his Parkinson’s patients would often see a temporary flare in tremors before the long-term improvement kicked in.
The Critical Role of Co-Factors
You cannot do this in a vacuum. If you just hammer B1 and ignore everything else, you’re going to hit a wall.
Thiamine needs Magnesium. Period.
Magnesium is the "key" that unlocks the thiamine. Without it, the B1 just sits there, unable to convert into its active form (Thiamine Pyrophosphate). If you're low on magnesium—and let's be real, almost everyone is—the high dose thiamine protocol will likely fail or cause a nasty paradox reaction.
You also need the other B-vitamins in balance. A good B-complex is usually recommended alongside the high-dose B1 to make sure you don't create an imbalance elsewhere. Potassium is another big one; when your metabolism ramps up, your cells start sucking up potassium, which can lead to low blood levels and heart palpitations.
What the Research Actually Says
This isn't just "internet medicine."
Dr. Antonio Costantini published numerous papers on using high-dose intramuscular or oral thiamine for neurological disorders. In his 2013 study on fatigue in inflammatory bowel disease, patients saw a "near-complete disappearance of fatigue" within days of starting high-dose B1.
💡 You might also like: Advanced Urgent Care Marathon: What Actually Happens When You Need Care in Florida
Think about that. People who had been exhausted for years were suddenly functional.
In another study involving Parkinson’s disease, Costantini found that 2 grams of oral thiamine daily led to significant improvement in motor function. The theory is that these diseases might actually be a form of "localized" thiamine deficiency in the brain, even if the blood levels look fine. It’s about thiamine efficiency, not just the amount in your veins.
How People Actually Start (The Practical Side)
Nobody should just jump into 2000mg of TTFD on day one. That’s a recipe for disaster.
The most successful approach is usually "low and slow."
Start with maybe 50mg of a high-quality B1. See how you feel for a week. If the "paradox" hits, you might even need to drop lower. Once that settles, you bump it up. Some people find their "sweet spot" at 100mg, while others don't see results until they hit that 1000mg+ range. It’s highly individual.
You have to listen to your body. If you get irritable or can't sleep, you might be pushing too fast or missing a co-factor like magnesium.
Addressing the Skeptics
Wait, can you overdose?
Thiamine is water-soluble. Your kidneys are pretty great at peeing out what you don't use. While "toxicity" is almost unheard of with oral B1, you can definitely feel "over-stimulated." This isn't because the vitamin is toxic, but because your nervous system is being revved up faster than it can handle.
Also, doctors often worry about "masking" other deficiencies. This is why regular blood work for things like B12 and folate is still important. But the idea that thiamine is dangerous at high doses simply isn't backed by the clinical literature.
Real World Applications: POTS and Dysautonomia
One of the most exciting areas for the high dose thiamine protocol is in the treatment of Dysautonomia and Postural Orthostatic Tachycardia Syndrome (POTS).
The autonomic nervous system—the stuff that controls your heart rate, digestion, and breathing—is incredibly thiamine-dependent. When thiamine is low, the brainstem can't properly regulate these functions. Patients often report that their heart rate stabilizes and their "air hunger" disappears once they find the right dose of B1.
It's not a cure-all, but for many, it's the missing piece of the puzzle that exercise and salt pills couldn't fix.
Actionable Next Steps for Success
If you’re looking to explore this, don’t just buy the first bottle you see on Amazon.
💡 You might also like: Why Masturbate on the Toilet is More Common Than You Think
- Test, don't guess (with a grain of salt). Ask for an Erythrocyte Transketolase Activity test if you can. It’s more accurate than a standard serum B1 test, though still not perfect.
- Prioritize Magnesium. Start taking a highly absorbable magnesium (like Glycinate or Malate) at least a week before you start the thiamine. This primes the pump.
- Choose your form wisely. If you have "brain fog" or neurological symptoms, look into TTFD (often sold under brand names like Thiamax or Ecological Formulas). If you have nerve pain in your limbs, Benfontiamine might be your best bet.
- Keep a symptom log. Write down what you take and how you feel. The "paradox" can be confusing; having a log helps you see if you're actually making progress over the weeks.
- Work with a functional practitioner. Especially if you have complex health issues, having a professional guide you through the dosing can prevent a lot of trial-and-error frustration.
The high dose thiamine protocol is a tool, not a miracle. But for those whose cells have been starving for energy, it can feel like someone finally turned the lights back on. Just remember to go slow, keep your magnesium up, and pay attention to what your body is trying to tell you.