You’re sitting in the doctor’s office. The cuff squeezes your arm until it pulses. The nurse rattles off two numbers, maybe 120 over 95, and suddenly there’s a look of concern. You probably know the top number—the systolic—is the "big" one everyone worries about. But that high bottom number on blood pressure, known as diastolic pressure, is often the part of the reading that leaves people scratching their heads. It’s the pressure in your arteries when your heart is resting between beats.
Think about that for a second. Even when your heart isn't actively pumping, your blood is still pushing against your vessel walls with significant force. If that "rest" pressure is high, your system never actually gets a break.
For a long time, doctors focused almost exclusively on the top number, especially in older patients. They figured the systolic reflected the hardening of the pipes. But recent data, including a massive study published in the New England Journal of Medicine involving over 1.3 million people, suggests that both numbers independently predict the risk of heart attack and stroke. If your bottom number is consistently over 80, you’re looking at what’s called isolated diastolic hypertension (IDH). It's more common in younger adults than you'd think. It's sneaky.
The Mystery of Isolated Diastolic Hypertension
What actually causes a high bottom number on blood pressure?
Usually, it's about the resistance in your peripheral blood vessels. If the tiny arteries throughout your body are narrowed or stiff, the pressure stays high even between heartbeats. It's like trying to force water through a garden hose that someone is stepping on. In younger folks, this is often the first sign that the cardiovascular system is struggling. You might feel totally fine. No headaches. No chest pain. Just a number on a screen that won't go down.
Weight plays a huge role here. So does alcohol. If you’re having more than two drinks a night, your diastolic pressure is likely taking a hit. Interestingly, some research suggests that stress and high sodium intake impact the diastolic reading more acutely in certain populations. It's not just about "eating salt"; it's about how your kidneys handle that salt and how your nervous system reacts to the daily grind.
The 80 vs. 90 Debate
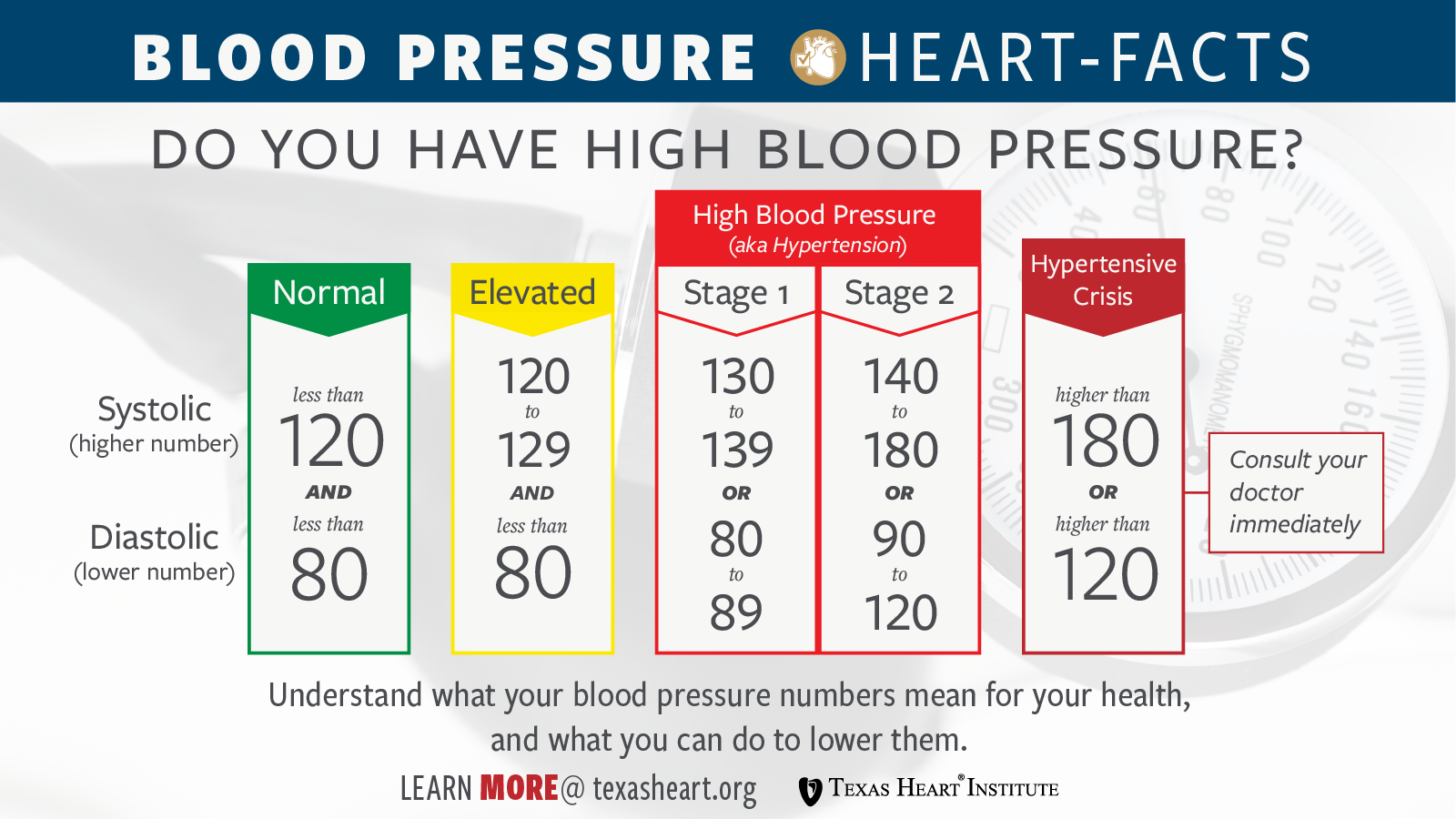
The American Heart Association (AHA) shifted the goalposts a few years ago. They used to say 90 was the cutoff for the bottom number. Now? It’s 80.
✨ Don't miss: Horizon Treadmill 7.0 AT: What Most People Get Wrong
This change wasn't just to sell more meds. It was based on the SPRINT trial and other longitudinal observations showing that damage starts much earlier than we realized. When that bottom number hangs out between 80 and 89, you are technically in Stage 1 Hypertension. Many people find this frustrating. You go from "healthy" to "hypertensive" overnight because of a guideline change. But the reality is that your vessels don't care about guidelines; they care about the constant pressure.
Why Younger Adults Should Worry
If you're 30 and your reading is 115/95, you might think you're "mostly" fine because the top number is great. Honestly, that's a mistake. Isolated diastolic hypertension is a strong predictor of future heart failure.
A study led by Dr. Alexander Flint at Kaiser Permanente found that while systolic pressure has a greater overall impact, a high diastolic reading still significantly increases the risk of "adverse cardiovascular events." In younger people, the diastolic number is often the very first red flag. It’s the canary in the coal mine. Ignoring it because you "feel young" is a gamble with your 50-year-old self.
Hormones and the Bottom Number
Secondary causes can sometimes be the culprit. We’re talking about things like primary aldosteronism—a condition where your adrenal glands pump out too much of a hormone that holds onto salt. This can drive that bottom number through the roof while the top number stays relatively normal. Thyroid issues, both overactive and underactive, can also mess with your diastolic pressure. If you’re lean, active, and still seeing a high bottom number on blood pressure, it’s worth asking your doctor to check your hormones or your kidneys. It's not always just about "stress."
The "White Coat" and Home Monitoring
Don't panic over one high reading at the doctor's office. "White coat hypertension" is real. Your nervous system kicks into gear because you're in a sterile room with a person in a lab coat.
To get the real story, you need to monitor at home. But you have to do it right. Sit still for five minutes. No talking. No scrolling on your phone. Feet flat on the floor. If you take your blood pressure right after a stressful meeting or a cup of coffee, that bottom number will be artificially inflated.
🔗 Read more: How to Treat Uneven Skin Tone Without Wasting a Fortune on TikTok Trends
Consistency is king. Track it for a week, morning and night. If the average is still high, then you have a baseline to discuss with a professional.
What Actually Works to Lower It?
You’ve heard the "eat better, exercise more" speech a thousand times. Let's get specific.
To target a high bottom number on blood pressure, focus on potassium. Potassium helps your body flush out sodium and eases the tension in your blood vessel walls. Think bananas, sure, but also avocados, spinach, and white beans. Most people get way too much sodium and nowhere near enough potassium. Shifting that ratio can move the needle on a stubborn diastolic number in a matter of weeks.
Magnesium is another big one. It acts like a natural calcium channel blocker, helping your arteries relax.
Then there’s the cardio. Not just a stroll, but "zone 2" exercise where you’re breathing heavy but can still talk. This improves the elasticity of your arteries. If your vessels are more elastic, they can "snap back" better between beats, which naturally lowers that resting pressure.
The Alcohol Connection
This is the one nobody wants to hear. Alcohol is a potent vasoconstrictor. For many people, cutting out the nightly glass of wine or the weekend binge is the fastest way to drop the diastolic number by 5 or 10 points. It's almost immediate. If you're struggling with a high bottom number, try a "dry" month and watch the monitor. The results usually speak for themselves.
💡 You might also like: My eye keeps twitching for days: When to ignore it and when to actually worry
When Do You Need Meds?
If lifestyle changes don't work after three to six months, it might be time for a prescription.
Doctors often start with ACE inhibitors or ARBs. These drugs don't just "lower pressure"; they protect your kidneys and help your blood vessels dilate. For some, a low-dose diuretic is the answer. The goal isn't to be on pills forever, though for some it’s a genetic necessity. The goal is to keep your arteries from stiffening into concrete.
High diastolic pressure is often more responsive to weight loss and salt reduction than systolic pressure is, especially in younger patients. Use that to your advantage.
Actionable Steps for Today
If you're staring at a high bottom number on your latest cuff reading, don't just wait for the next annual check-up.
- Buy a validated home monitor. Look for one that is "clinically validated" (the Omron Silver or Gold series are generally reliable).
- Log your salt. Use an app for three days. Don't change how you eat—just track. You’ll probably be shocked to find you're hitting 4,000mg of sodium. Aim for under 2,300mg.
- The 2-minute breathing trick. Slow, deep breathing (6 breaths per minute) for just 5-10 minutes a day can tone down your sympathetic nervous system. This is the "fight or flight" system that keeps your vessels constricted.
- Check your sleep. Sleep apnea is a massive, often undiagnosed cause of high diastolic pressure. If you snore or wake up tired, get a sleep study. No amount of kale will fix the pressure spike caused by not breathing at night.
- Screen for "Secondary" causes. If you’re under 40 and your bottom number is consistently over 95 despite a healthy lifestyle, demand a blood test for renin and aldosterone levels.
A high bottom number on blood pressure is a manageable metric, but it requires more than just "trying to relax." It's a physiological signal that your vascular resistance is too high. Address the stiffness, address the salt, and give your heart the rest it deserves between beats. Keeping that number under 80 isn't just a clinical goal; it's a long-term insurance policy for your brain and your heart.