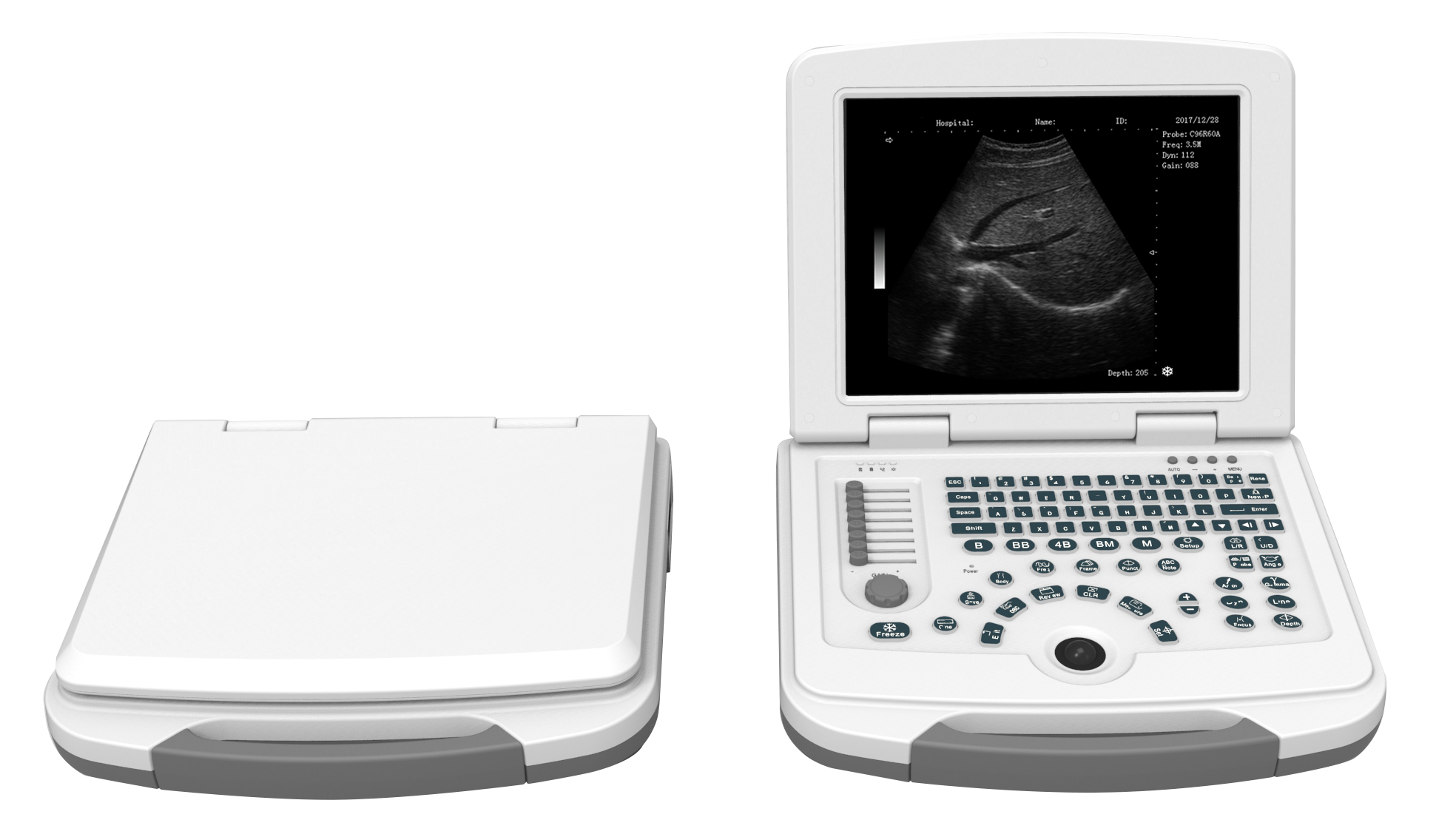
It’s small. Smaller than you’d think. For decades, if you wanted to see inside a patient’s body in real-time without radiation, you had to wheel in a machine the size of a refrigerator. It was clunky, expensive, and lived in a dedicated basement room. But things have changed. A modern hand held ultrasound machine now fits in a coat pocket, plugs into an iPhone, and costs less than a used Honda Civic.
Honestly, it’s a bit of a revolution.
We are seeing a massive shift in how doctors, paramedics, and even rural health workers diagnose problems at the bedside. This isn't just about making things smaller for the sake of it; it’s about "democratizing" imaging. If you can carry a high-quality scanner in your pocket, the "physical exam" changes forever. You’re no longer just poking a sore abdomen and guessing; you’re looking at the gallbladder right then and there.
The Death of the Stethoscope?
People have been saying the stethoscope is dead for ten years. It’s not. Not yet. But the hand held ultrasound machine is definitely making it look like a relic from the 1800s. Why listen to heart murmurs when you can actually see the mitral valve failing?
Dr. Eric Topol, a cardiologist and a huge advocate for digital medicine, has been vocal about this for years. He’s often pictured with a device like the Butterfly iQ, arguing that the "visual stethoscope" is the future. And he’s right, mostly. But there’s a catch. Having the tech doesn’t make you an expert. You can buy a professional-grade camera, but that doesn't make you Annie Leibovitz.
The biggest hurdle isn't the hardware anymore. It’s the "image acquisition" and "interpretation." Basically, can you actually find the kidney, and do you know what a stone looks like when you see it?
How the Tech Actually Works (No, It’s Not Just Shrunken Parts)
Traditional carts use piezoelectric crystals. You zap them with electricity, they vibrate, send out sound waves, and catch the echoes. Shrinking those crystals is hard and expensive.
Then came Silicon.
A company called Butterfly Network changed the game by putting the "ultrasound on a chip." They replaced the crystals with thousands of micro-machined sensors on a semiconductor wafer (CMOS). This is why a hand held ultrasound machine can suddenly cost $2,000 instead of $50,000. It’s the same way computers went from room-sized monsters to the smartphone in your hand.
Other players like GE HealthCare with their Vscan line and Philips with Lumify still use high-end transducer tech, but they've mastered the art of miniaturizing the beamformer. These devices are rugged. They’re meant to be dropped in an ER or wiped down with harsh chemicals after a messy trauma case.
Where This Stuff Actually Matters
Think about a rural clinic in sub-Saharan Africa. Or a LifeFlight helicopter over the Rockies. You can't fit a 300-pound GE Voluson in those spots.
- Point-of-Care Ultrasound (POCUS): This is the buzzword. It means doing the scan wherever the patient is. In the ER, if someone comes in with a suspected collapsed lung (pneumothorax), a doctor can use a handheld probe and get an answer in 30 seconds. That’s faster than an X-ray. Way faster.
- Medical Education: Medical students are now getting these devices on day one. They use them to learn anatomy. Instead of just looking at a drawing of a brachial plexus, they’re finding it on their own necks.
- Home Health: This is the "Wild West" of the industry. We are starting to see devices cleared for home use, specifically for things like bladder scanning or monitoring chronic heart failure.
It’s kinda wild to think about.
But there are serious concerns about "incidentalomas." That’s the medical term for finding something totally harmless that looks scary on a screen, leading to a cascade of expensive, invasive, and unnecessary tests. When everyone has a scanner, everyone finds "something."
The Big Players You Should Know
If you’re looking into this space, you’ll run into a few names constantly.
Butterfly Network is the disruptor. Their iQ3 is the latest iteration. It’s versatile because the chip can emulate different types of probes (linear, curved, phased). Usually, you’d need three different heads for those.
GE HealthCare is the titan. The Vscan Air is their flagship handheld. It’s wireless. That’s a huge deal in a sterile environment like an OR. No cables to trip over or contaminate.
Vave Health and Clarius are also pushing the envelope. Clarius, in particular, is known for high-resolution images that rivals some mid-tier cart systems. They use AI to help with "auto-gain" and "auto-preset," which basically means the machine tries to fix the settings so you don't have to be an expert knob-turner.
The AI Factor
Artificial Intelligence is the "secret sauce" making these devices viable for non-radiologists. Some modern hand held ultrasound machine software can now:
- Calculate "Ejection Fraction" (how well your heart pumps) automatically.
- Count B-lines in the lungs to check for fluid.
- Tell you if you’re actually looking at a carotid artery or a jugular vein.
It’s like having a tiny radiologist whispering in your ear. But—and this is a big "but"—AI can be wrong. It’s a tool, not a replacement for clinical judgment.
The Reality Check: Is It Actually "Good"?
Let’s be real. A $2,000 probe is not going to give you the same image quality as a $150,000 premium cart used for detailed fetal echoes. Physics is physics. Small transducers have smaller apertures.
However, for 80% of clinical questions, the handheld is "good enough."
- Is there internal bleeding? (FAST exam) - Yes.
- Is the heart squeezing? - Yes.
- Is there a blood clot in the leg (DVT)? - Yes.
- Is the baby head-down? - Yes.
For these binary "yes/no" questions, the portability outweighs the slightly lower resolution.
Cost and Subscription Models
Here is where it gets annoying.
Most of these companies have moved to a "SaaS" (Software as a Service) model. You buy the probe for a flat fee, but if you want the cool AI features or cloud storage for your images, you have to pay a monthly or yearly subscription. This is a massive headache for private practices but a standard operating procedure for large hospital systems.
You need to factor this into the "Total Cost of Ownership." A "cheap" probe might end up costing you $5,000 over three years once you add in the software fees.
Privacy and Security
Because these devices often plug into phones or tablets, HIPAA compliance is a major hurdle. You can’t just snap a picture of a patient's heart and save it to your personal Google Photos. The apps that run these scanners have to be encrypted, and the images usually have to be pushed to a secure hospital PACS system.
If you're a solo practitioner, you need a plan for where those images live.
✨ Don't miss: How many grams of protein in a lb of chicken: What your meal prep is probably missing
Actionable Next Steps for Healthcare Providers
If you are considering adding a hand held ultrasound machine to your practice, don't just buy the one with the best Instagram ads.
- Identify your primary use case: If you do aesthetics (fillers), you need a high-frequency linear probe for superficial scanning. If you’re a GP, you need a "generalist" probe like the Butterfly or a dual-headed GE Vscan.
- Check device compatibility: Most run on iOS, but Android support can be spotty for certain brands. Ensure your tablet has the processing power to handle real-time image rendering.
- Get formal training: Look into courses from organizations like the Society of Point of Care Ultrasound (SPOCUS) or the American College of Emergency Physicians (ACEP).
- Test the workflow: Download the app before you buy the hardware. Is the interface intuitive? How many clicks does it take to save an image? In a busy clinic, those clicks matter.
- Review the storage policy: Determine if you need a cloud subscription or if the device allows for local DICOM export to your existing EMR.
The technology has officially moved past the "gimmick" phase. It is now a legitimate clinical tool that, when used correctly, saves lives by catching diagnoses that would have otherwise waited for a formal imaging appointment three weeks later.
Get hands-on with a few demo units. Compare the "near-field" resolution if you’re doing needle guidance. Check the battery life—some units get hot after 15 minutes of continuous scanning. These are the practical realities that don't show up in the glossy brochures but define your experience at the bedside.
The era of the "pocket-sized" hospital is here. It’s just a matter of who learns to use it first.