So, you’re staring at a black-and-white image that looks like a grainy Rorschach test, and someone just told you it’s your prostate. It’s scary. Honestly, looking at MRI pictures of prostate cancer for the first time is overwhelming because, to the untrained eye, everything looks like a smudge. But for a radiologist, these images are a map. They aren't just snapshots; they are data-rich slices of your anatomy that can literally change the course of your treatment.
The shift toward using multiparametric MRI (mpMRI) has been a total game-changer in urology. Ten years ago, if your PSA was high, a doctor might have just gone in for a "blind" biopsy, poking around and hoping to hit the right spot. Now? We use these detailed images to see exactly where the trouble might be hiding. It’s about precision.
Why MRI Pictures of Prostate Cancer Aren't Just "Photos"
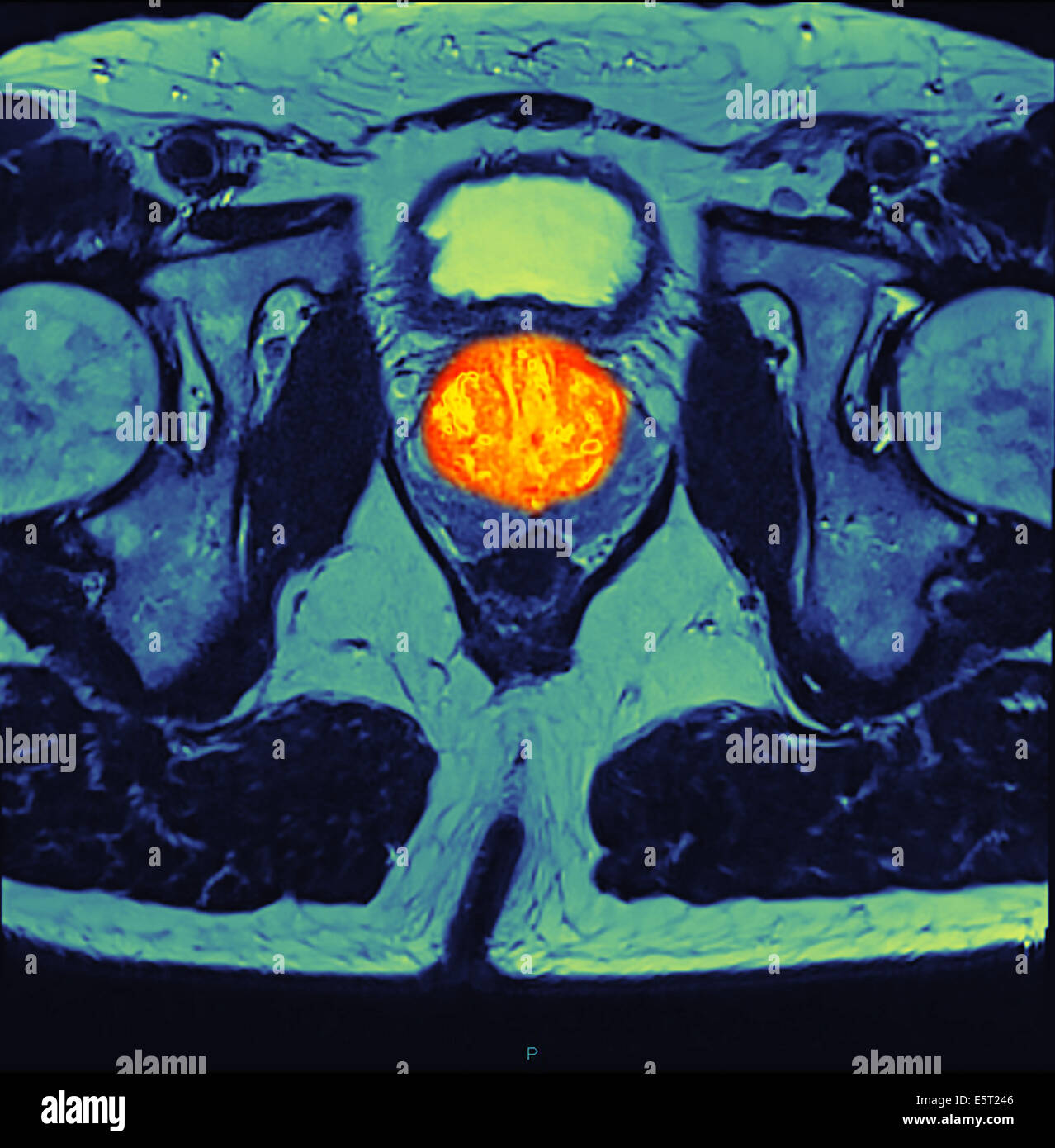
When we talk about an MRI, we aren't just talking about one picture. We’re talking about sequences. Think of it like a filtered camera lens. One sequence shows the anatomy (T2-weighted imaging), another shows how water molecules are moving (Diffusion-weighted imaging), and another shows blood flow (Dynamic Contrast Enhanced).
Prostate cancer cells are crowded. They’re packed together much tighter than healthy tissue. Because they are so cramped, water molecules can't move around as easily. This shows up on the "Diffusion" sequence as a bright white spot or a dark "hole," depending on which map the doctor is looking at. It’s this specific behavior of water—the way it gets trapped by tumors—that makes MRI pictures of prostate cancer so incredibly useful for spotting aggressive cells.
The PI-RADS Language
You might see a number on your report: PI-RADS 1 through 5. This isn't a "cancer score" in the way a Gleason score is, but rather a probability scale.
🔗 Read more: Why Having Sex in Bed Naked Might Be the Best Health Hack You Aren't Using
- A PI-RADS 1 or 2 means things look pretty normal.
- PI-RADS 3 is the "maybe" zone—it’s indeterminate.
- PI-RADS 4 and 5? That’s where the radiologist sees something highly suspicious.
It’s not perfect. Nothing in medicine is. But it gives your urologist a massive head start.
The T2-Weighted Image: The Anatomy Slice
The T2-weighted sequence is usually the "pretty" one. It shows the prostate’s zones clearly. Most prostate cancers—about 70% to 75%—start in the peripheral zone, which is the outer part of the gland. On a healthy T2 image, this area looks bright white. If cancer is present, it often shows up as a dark, "smudgy" area.
Radiologists look for what they call "circumscribed" or "ill-defined" masses. If the dark spot has ragged edges or looks like it's pushing through the capsule (the outer skin of the prostate), that’s a red flag. It suggests the cancer might be trying to escape into nearby tissues. This is vital. Knowing if the cancer is "organ-confined" versus "extracapsular" is the difference between a simple surgery and a much more complex treatment plan involving radiation or hormones.
What Happens When the Image Is "Noisy"?
Not everything that looks like cancer is cancer. This is the part that trips people up. Prostatitis (inflammation) or Benign Prostatic Hyperplasia (BPH) can create shadows that mimic tumors on MRI pictures of prostate cancer. BPH usually happens in the transition zone—the inner part of the prostate—and it can look like a chaotic mess of "nodules."
💡 You might also like: Why PMS Food Cravings Are So Intense and What You Can Actually Do About Them
This is why the radiologist's expertise matters so much. A study published in The Lancet (the PROMIS trial) showed that MRI is excellent at ruling out aggressive cancer, but it can still have "false positives." You might have a PI-RADS 4 lesion that turns out to be a bunch of inflamed cells once the biopsy needle actually hits it. It’s frustrating, but it’s part of the process of narrowing things down.
The Fusion Biopsy: Bringing Pictures to Life
The coolest thing happening right now is MRI-Ultrasound Fusion. Traditionally, urologists used ultrasound to guide biopsies. The problem? Ultrasound is great at seeing the shape of the prostate but terrible at seeing the actual cancer. It’s like trying to find a specific person in a crowd while wearing blurry glasses.
By taking the MRI pictures of prostate cancer and "overlaying" them onto the live ultrasound, the doctor can see exactly where the suspicious lesion is in real-time. They aren't guessing anymore. They are aiming. This has significantly increased the detection of "clinically significant" prostate cancer—the kind that actually needs treatment—while helping men avoid treatment for the slow-growing stuff that would never have bothered them.
Limitations You Should Know
Don't let anyone tell you an MRI is a 100% guarantee. Some small, low-grade tumors are "invisible" on MRI. They just don't have enough cell density to change the signal. Also, the quality of the image depends heavily on the machine. A 3-Tesla (3T) MRI provides much clearer pictures than an older 1.5T machine. If you're getting an MRI, ask if it's a 3T. It makes a difference in the "graininess" of the shot.
📖 Related: 100 percent power of will: Why Most People Fail to Find It
How to Read Your Own Report (Without Panicking)
When you get your results, don't just look for the word "cancer." Look for descriptions of "restricted diffusion." That’s the big one. If the report says "no restricted diffusion," that’s usually a very good sign, even if there are some dark spots on other sequences.
Also, look for mentions of the "neurovascular bundles." These are the nerves that control erections. They run right alongside the prostate. If the MRI pictures show the tumor is far away from these nerves, your surgeon has a much better chance of "nerve-sparing" surgery, which is huge for your quality of life afterward.
Actionable Next Steps
If you’ve just received an MRI report or you’re scheduled for one, here is how to handle it:
- Verify the Equipment: Ensure the scan is being done on a 3T MRI machine. The higher field strength is standard for high-quality prostate imaging in 2026.
- Request a Specialized Radiologist: Not all radiologists specialize in the pelvis. Ask if your scan will be read by an abdominal radiologist or someone who specifically focuses on prostate imaging. Experience matters in interpreting those "smudges."
- Get the CD/Digital Link: Always ask for a copy of the actual images, not just the written report. If you want a second opinion at a major cancer center like Memorial Sloan Kettering or Mayo Clinic, they will want to see the "raw" MRI pictures of prostate cancer themselves.
- Compare PSA to Volume: Ask your doctor about PSA Density. This is your PSA score divided by the volume of your prostate (which the MRI measures). A high PSA in a very small prostate is more concerning than a high PSA in a massive, BPH-riddled prostate.
- Discuss Fusion Biopsy: If the MRI shows a PI-RADS 3, 4, or 5, don't settle for a standard 12-core biopsy. Insist on an MRI-targeted fusion biopsy to ensure the suspicious area is actually sampled.
Understanding these images is about moving from fear to strategy. The "pictures" aren't a diagnosis on their own; they are the most powerful tool we have to make sure your diagnosis is accurate and your treatment is necessary.