You’re lying in bed, your bones ache like you’ve been run over by a freight train, and your forehead feels like a stovetop. You check your temperature. It's high. You probably assume it’s "the flu," but which one? Most people spend their lives worrying about the big, scary Type A strains—the ones that cause global pandemics and jump from birds to humans. But flu virus type b is a different beast entirely. It’s sneaky. It doesn't care about your neighbor’s pig farm or a flock of ducks in another country. It is a strictly human pathogen, and honestly, that’s exactly what makes it so efficient at making our lives miserable every winter.
It hits kids harder. That's the reality. While Influenza A might be the one making headlines for "Spanish Flu" or "Swine Flu," Type B is often the quiet driver behind those pediatric hospitalizations that keep parents up at night. It doesn't mutate as fast as its cousin, sure, but it’s remarkably stable in its ability to ruin your month.
What Flu Virus Type B Actually Is (and Isn't)
Let's clear something up. Influenza B isn't "stomach flu." If you're throwing up but don't have a fever or a cough, you've likely got a norovirus. True flu virus type b is a respiratory infection. It lives in your nose, throat, and lungs. Unlike Influenza A, which can infect everything from horses to seals, Type B is almost exclusively a human problem. This limited "host range" means it doesn't shift its genetic makeup in massive, earth-shattering ways like Type A does. We don't see "shifts" where a totally new virus emerges; instead, we see "drifts."
Small changes. Tiny tweaks.
These subtle mutations are why you still need a vaccine every single year. The virus evolves just enough so that your immune system's "Most Wanted" posters from last year are slightly out of date. Currently, the world deals with two main lineages: Victoria and Yamagata. Interestingly, since the COVID-19 pandemic, the Yamagata lineage has basically vanished from global surveillance. Scientists at the World Health Organization (WHO) are actually discussing whether we even need to include it in future vaccines. It might be extinct. Imagine that—a virus lineage potentially wiped out not by a specific cure, but by a global shift in human behavior.
Why the Symptoms Feel Different
You’ll know it when it hits. Usually, it starts with a sudden fever. One minute you're fine; the next, you're shivering under three blankets.
Common symptoms of flu virus type b include:
✨ Don't miss: Ankle Stretches for Runners: What Most People Get Wrong About Mobility
- An exhausting, dry cough that feels like it’s coming from your toes.
- Extreme fatigue—the kind where walking to the bathroom feels like running a marathon.
- Severe muscle aches, particularly in the back and legs.
- A sore throat that makes swallowing feel like sandpaper.
- Congestion, though often less "drippy" than a common cold.
Kids often get hit with gastrointestinal issues alongside the respiratory stuff, which is where the confusion about "stomach flu" comes from. But make no mistake, the primary site of the war is the lungs. If you're an adult, you might just feel like you have a "bad cold" for the first 24 hours. Then the hammer drops. The fatigue associated with Type B can linger for weeks. You might clear the fever in five days, but the "brain fog" and lethargy can stick around like an unwanted houseguest.
The Victoria vs. Yamagata Divide
For years, we’ve used quadrivalent vaccines. These shots contain two strains of Influenza A and two of Influenza B. Specifically, they target one virus from the Victoria lineage and one from the Yamagata lineage. Why both? Because for decades, they took turns being the dominant strain. Victoria tended to hit younger people more frequently, while Yamagata was often seen in older adults.
But as mentioned, the Yamagata strain hasn't been seen in the wild since early 2020. This is a massive deal in the virology world. Dr. Kanta Subbarao, a leading flu expert and director of the WHO Collaborating Centre for Reference and Research on Influenza, has noted that the disappearance of Yamagata could simplify how we manufacture vaccines. If it’s gone, we could move back to trivalent vaccines, focusing more energy on the strains that are actually still circulating and killing people.
Is It More Dangerous Than Type A?
That's a bit of a trick question. For a long time, the medical community thought Type B was "milder." We were wrong. Research published in Clinical Infectious Diseases has shown that the clinical severity of flu virus type b is actually quite similar to Type A. In some seasons, especially for children and teenagers, it can actually be more lethal.
Complications are real. We aren't just talking about a runny nose.
- Secondary bacterial pneumonia. This is what often leads to hospitalization. Your immune system is so busy fighting the flu that a bacteria like Streptococcus pneumoniae moves in and sets up shop.
- Myocarditis. Inflammation of the heart muscle. It’s rare, but it’s a documented complication of Influenza B.
- Encephalitis. Brain inflammation that can cause seizures or permanent damage.
- Myositis. This is specifically common with Type B in children—severe calf pain that makes it hard for them to walk.
If you see a child struggling to breathe, or if they seem suddenly confused or won't wake up, that’s an emergency. Don't wait.
🔗 Read more: Can DayQuil Be Taken At Night: What Happens If You Skip NyQuil
The Timing: When Does It Strike?
Influenza A often peaks early in the winter—December or January in the Northern Hemisphere. Flu virus type b is the "late bloomer." It often shows up in February, March, or even as late as May. Just when you think you've survived the flu season, Type B walks through the door.
This bimodal peak—two waves of sickness—is why doctors get frustrated when people skip their shots in late autumn. If you only have immunity against the early-season Type A, you're a sitting duck when the Type B wave hits in the spring.
Testing and Diagnosis
You can't diagnose this yourself. You just can't. A "rapid flu test" at an urgent care center is the standard move. They stick a swab up your nose, and fifteen minutes later, you have an answer. However, these rapid tests aren't perfect. They have a decent rate of false negatives. If it says you're negative but you feel like death, your doctor might send a sample for a PCR test.
PCR (Polymerase Chain Reaction) is the gold standard. It’s the same tech used for COVID-19. It looks for the actual genetic material of the flu virus type b. It takes longer—maybe a day or two—but it’s incredibly accurate.
Treatment Options That Actually Work
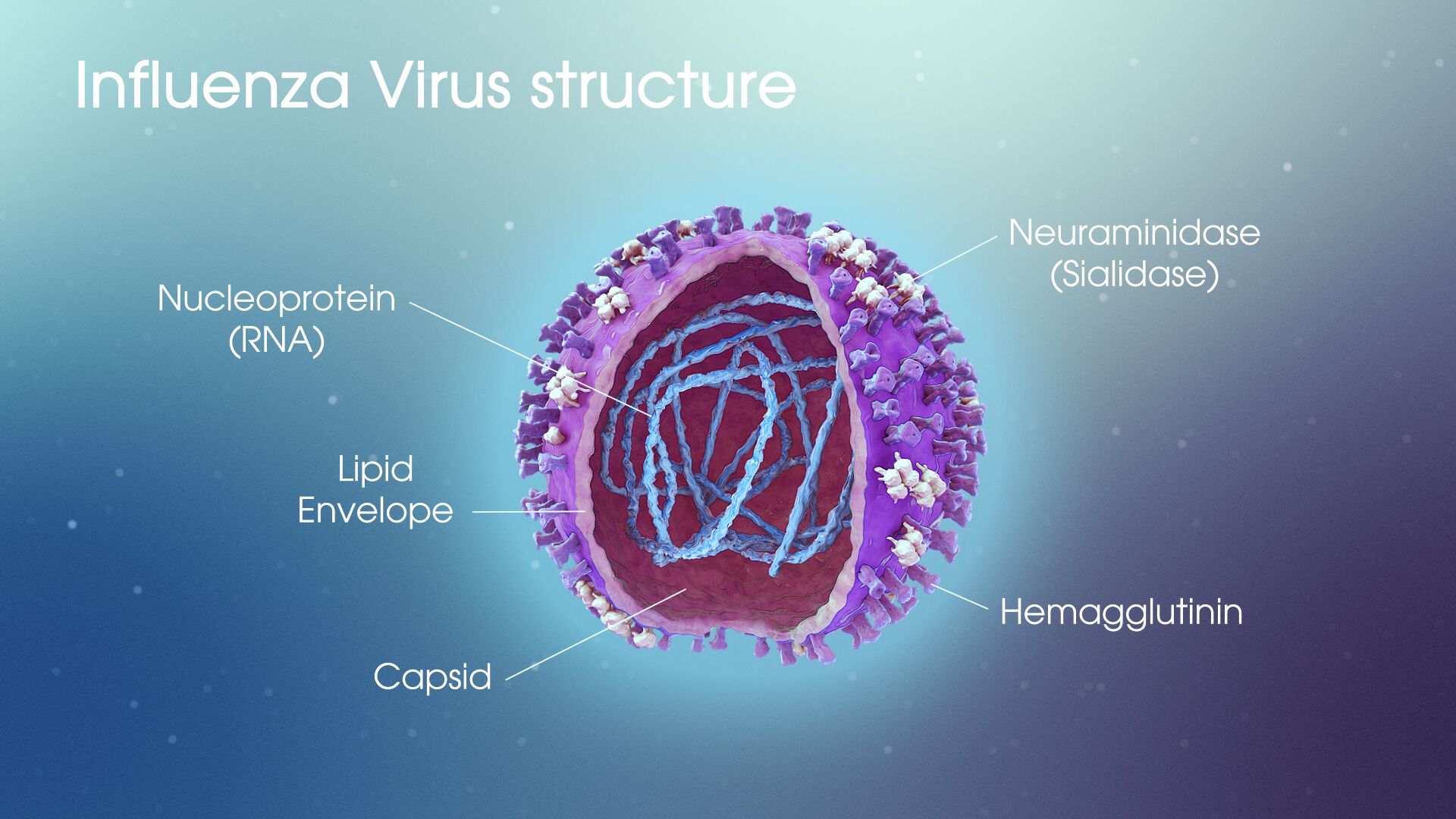
Antivirals are the name of the game. Oseltamivir (Tamiflu) is the one everyone knows. It doesn't "kill" the virus like an antibiotic kills bacteria. Instead, it’s a neuraminidase inhibitor. Basically, it prevents the virus from escaping an infected cell to go infect new ones.
Timing is everything here. If you don't start Tamiflu within the first 48 hours of symptoms, it's mostly useless. It might shave half a day off your sickness, but it won't prevent the heavy hitting. If you get it early, it can significantly reduce the risk of those scary complications like pneumonia.
💡 You might also like: Nuts Are Keto Friendly (Usually), But These 3 Mistakes Will Kick You Out Of Ketosis
There’s also Baloxavir marboxil (Xofluza). It’s a newer, single-dose pill. It works differently by stopping the virus from replicating its RNA in the first place. It's expensive, but for many, the convenience of one pill vs. five days of Tamiflu is worth it.
Honestly? Most people just need rest. Hydration is boring advice, but it's essential. When you have a fever, you lose fluids fast. Dehydration makes the muscle aches ten times worse. Drink water, electrolytes, or even just hot tea with honey.
Prevention and the Annual Shot
The vaccine is your best defense, even if it’s not 100% effective. Even if the "match" is off, having some antibodies in your system usually means if you do get flu virus type b, you’ll have a "mild" case rather than one that puts you in the ICU.
Masks work too. We learned that the hard way in 2020. If you’re in a crowded subway or a tiny office and you hear someone hacking their lungs out, a high-quality mask (like an N95 or KF94) provides a literal physical barrier. Flu travels in droplets. Stop the droplets, stop the virus.
Actionable Steps for Recovery and Protection
If you suspect you have the flu, or you're trying to avoid it, here is what you actually need to do:
- Get tested early. If you feel that sudden "hit" of fever and body aches, get to a clinic within 24 hours. This opens the window for antivirals to actually work.
- Watch for the "Second Dip." If you feel better for a day and then your fever comes back worse than before, call your doctor immediately. This is the classic sign of a secondary bacterial infection.
- Humidity is your friend. Use a cool-mist humidifier. It keeps your respiratory membranes moist, which helps your body trap and expel the virus more effectively.
- Isolate. You are contagious from the day before symptoms start until about 5 to 7 days after you get sick. Stay home. Don't be the person who brings flu virus type b to the office party.
- Check your vaccine status. If it’s late in the season and you haven't had a flu shot, get one. Remember, Type B often peaks late into the spring.
The reality of the flu is that it’s a manageable but serious illness. Respect the virus. Give your body the time it needs to recover, and don't ignore the warning signs of complications. Modern medicine has given us the tools to track and treat these infections, but they only work if we use them correctly and quickly.