You’re sitting on the couch. Maybe you’re watching a game or just scrolling through your phone after a long day. Suddenly, there’s this... feeling. It isn't a Hollywood-style "clutch your chest and fall over" moment. It's subtle. Kinda like indigestion, but weirder. You wait. It stays. You wonder if you should call someone or just take an antacid and go to bed.
Most people wait. That wait is the problem.
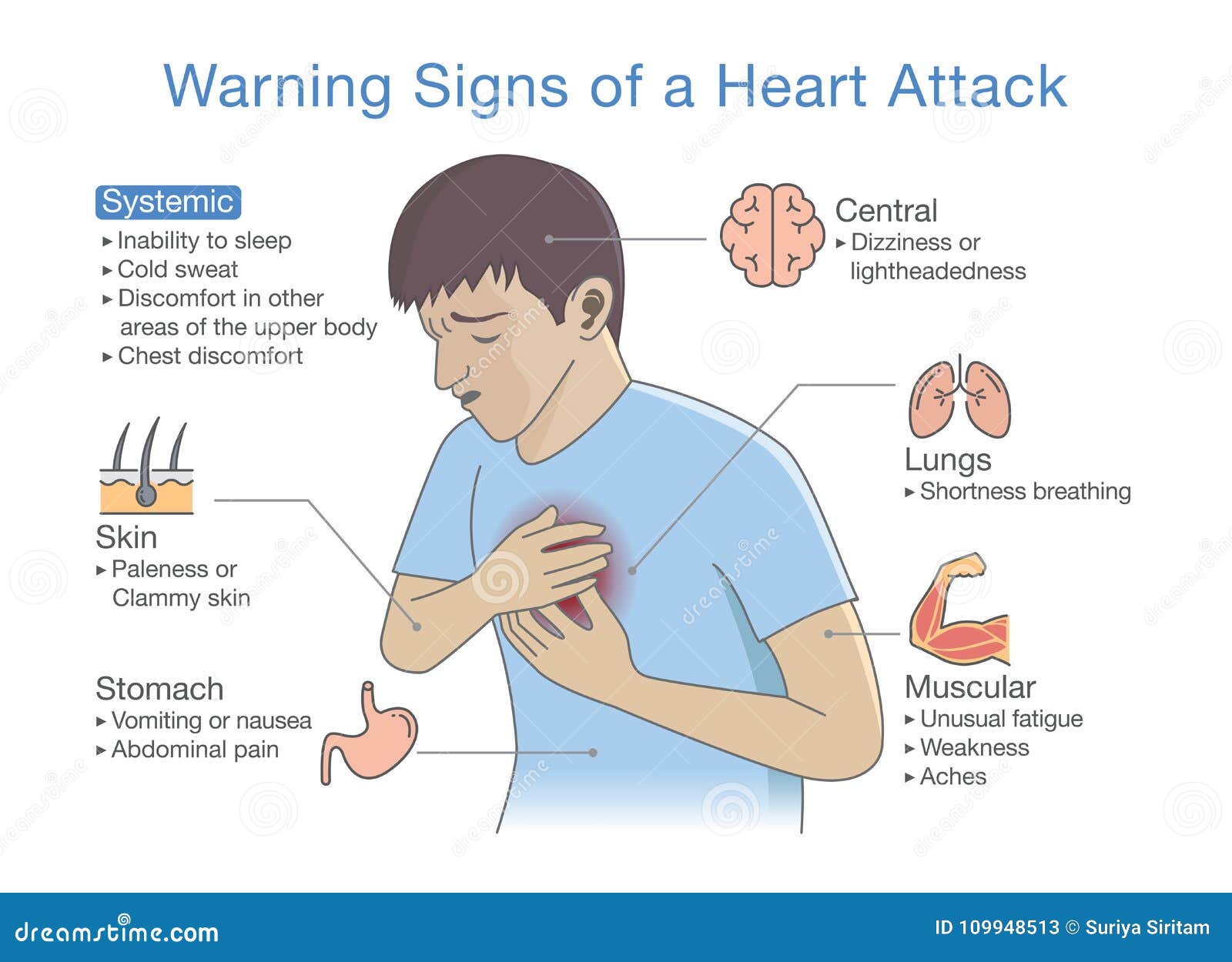
Knowing the five warning signs of a heart attack isn't just about memorizing a list from a textbook. It’s about understanding how your body actually screams for help when the blood flow to the heart muscle gets blocked. Sometimes it’s a roar. Often, it’s a whisper. If you’re waiting for the "elephant on the chest," you might miss the actual signal.
The American Heart Association (AHA) and the CDC keep hammering these points home because heart disease remains the leading killer globally. But statistics are boring. What matters is what’s happening in your chest—or your arm, or your jaw—right now.
1. That Pressure That Just Won't Quit
Chest discomfort is the classic. Everyone knows it. But "discomfort" is a broad word.
Patients often describe it as a squeezing sensation. It’s not always "pain" in the sharp, stabbing sense. Some people tell doctors it feels like a rope is being tightened around their ribcage. Others say it’s a heavy weight, like someone is standing on them.
Usually, this happens in the center or left side of the chest. It might last for more than a few minutes, or it might go away and then come roaring back. If you have a "fullness" that feels like you ate a brick, don't assume it’s the tacos you had for lunch.
✨ Don't miss: The Truth Behind RFK Autism Destroys Families Claims and the Science of Neurodiversity
The tricky part? Some people feel absolutely no chest pain at all. This is especially common in women, older adults, and people with diabetes. For them, the five warning signs of a heart attack might not even include the chest. That’s a scary thought, but it’s the reality of how biology works.
2. Pain That Travels (The Referred Pain Factor)
Your nerves are messy. Sometimes the brain gets confused about where a pain signal is coming from. This is called referred pain.
When the heart is struggling, it sends signals through the spinal cord that intersect with nerves connected to your jaw, neck, back, and arms. You might feel a dull ache in your lower jaw that you mistake for a toothache. Or maybe your left arm feels heavy and tingly. It’s rarely just the left arm, though; pain can show up in both arms or even your upper stomach.
I’ve heard stories of people heading to the dentist because of jaw pain, only to realize later they were having a myocardial infarction. If the pain radiates outward from your torso, pay attention. It’s a huge red flag.
Why Does It Move?
Basically, your heart doesn't have many "touch" sensors. When it's dying for oxygen, the nervous system basically blasts an SOS signal that bleeds into neighboring pathways. It's biological cross-talk.
3. Shortness of Breath (With or Without the Pain)
You’re out of breath. But you haven't been running. You’re just standing there, and suddenly it feels like you’re trying to breathe through a straw.
🔗 Read more: Medicine Ball Set With Rack: What Your Home Gym Is Actually Missing
This is a massive one of the five warning signs of a heart attack. Often, this symptom shows up before the chest pain even starts. Sometimes it’s the only symptom.
When the heart isn't pumping effectively, pressure builds up in the chambers and can actually cause fluid to "back up" into the lungs. This makes it incredibly hard to get a full breath. If you find yourself gasping for air while doing something easy—like walking to the mailbox—your heart might be trying to tell you something critical.
4. The "Flu" That Isn't a Flu
Nausea. Lightheadedness. A cold sweat that breaks out for no reason.
People often dismiss this. They think, "Oh, I’m just coming down with a bug" or "I must be dehydrated." But if you’re suddenly clammy and pale while feeling a sense of impending doom, that’s not the flu.
Women are significantly more likely to experience these "atypical" symptoms. They might feel an overwhelming sense of fatigue—like they’ve run a marathon when they’ve only walked across the room. It’s a deep, bone-weary exhaustion.
- Sudden cold sweats
- Feeling lightheaded or dizzy (like you might faint)
- Unexplained nausea or vomiting
- An intense feeling of anxiety or "doom"
These aren't just "stress." If they hit you out of nowhere alongside any other discomfort, the clock is ticking.
💡 You might also like: Trump Says Don't Take Tylenol: Why This Medical Advice Is Stirring Controversy
5. Upper Body Discomfort and "Indigestion"
We need to talk about the "heartburn" trap.
So many people take a Tums and go to sleep, never to wake up. They thought they had acid reflux. In reality, the bottom of the heart sits right above the diaphragm, near the stomach. Irritation or lack of blood flow in that area of the heart can feel exactly like a bad case of indigestion.
The difference? Heart-related "indigestion" usually doesn't get better with an antacid. It also tends to be accompanied by a feeling of being "unwell" that you can't quite put your finger on.
A Quick Reality Check on the Five Warning Signs of a Heart Attack
If you are over 50, have high blood pressure, smoke, or have high cholesterol, you don't get the luxury of assuming it’s just gas. You just don't. The risk is too high.
What to Actually Do When the Signs Appear
If you or someone you’re with is showing these five warning signs of a heart attack, stop what you're doing.
- Call 911 immediately. Do not drive yourself to the hospital. If you black out behind the wheel, you’re a danger to yourself and everyone else. Paramedics can start treatment the second they arrive. They have the EKG; your car doesn't.
- Chew an aspirin. Unless you’re allergic or have been told by a doctor never to take it, chew (don't swallow whole) a full-strength aspirin (325mg). Chewing it gets it into your bloodstream faster. It helps thin the blood and can potentially break up the clot that's causing the attack.
- Stay calm and sit down. Stop moving. Your heart needs to rest. Every bit of exertion makes the heart demand more oxygen—oxygen it isn't getting.
- Be honest with the ER staff. Don't downplay your symptoms. Don't say "it's probably nothing." Say "I think I'm having a heart attack." This triggers a specific protocol that gets you seen faster.
The Nuance of Gender and Age
The medical community has historically failed women by focusing primarily on "male" symptoms. Research from Harvard Health and the Mayo Clinic shows that women often experience shortness of breath, pressure in the lower chest or upper abdomen, and extreme fatigue rather than the "crushing" chest pain men usually report.
Younger people aren't immune either. With the rise of sedentary lifestyles and processed diets, we're seeing more heart events in people in their 30s and 40s. If you feel these symptoms, age isn't a shield.
Actionable Next Steps
- Check your vitals: If you have a blood pressure cuff at home, use it, but don't let it delay a 911 call.
- Know your history: Ask your parents about heart issues. Genetics play a massive role in how your arteries handle plaque.
- Schedule a Calcium Score test: If you’re worried about your risk, ask your doctor about a CT Calcium Score. It’s a quick scan that looks for calcified plaque in your coronary arteries. It's one of the best predictors of future heart events.
- Keep aspirin handy: Keep a small bottle in your car and your bedside table. It’s a literal lifesaver.
Recognizing the five warning signs of a heart attack is about intuition as much as it is about biology. If something feels "off" in your chest or upper body and it’s paired with breathlessness or a cold sweat, treat it as an emergency. It's much better to be sent home from the ER with a "false alarm" than to stay home with a fatal one.