You’re probably tired. Maybe your joints ache a little more than they should, or you’ve noticed your mood takes a nosedive the second the clocks turn back in October. Most people just call it "the winter blues" or getting older. Honestly, though? It’s often just a simple case of running low on the "sunshine vitamin." But finding good sources of vitamin d isn't as straightforward as just standing outside for five minutes or eating an orange.
It’s actually kinda complicated. Vitamin D isn't even a vitamin—it’s a pro-hormone. Your body has to manufacture it, or you have to consume it in specific forms that your liver and kidneys then have to process into something usable. If you're living in Chicago or London, the sun is basically useless for D production from November to March because the atmosphere filters out the UVB rays you need. You could stand outside naked in the snow for three hours and your levels wouldn't budge.
We have a global deficiency problem. Dr. Michael Holick, a massive name in vitamin D research at Boston University, has been screaming about this for decades. He points out that about 1 billion people worldwide are deficient. That’s a staggering number. It’s not just about bone health anymore; we’re talking about immune function, insulin sensitivity, and even how your heart beats.
📖 Related: Benefits of Baby Led Weaning: Why Letting Your Infant Feed Themselves Actually Works
The Sun vs. The Plate: Where the Real D Lives
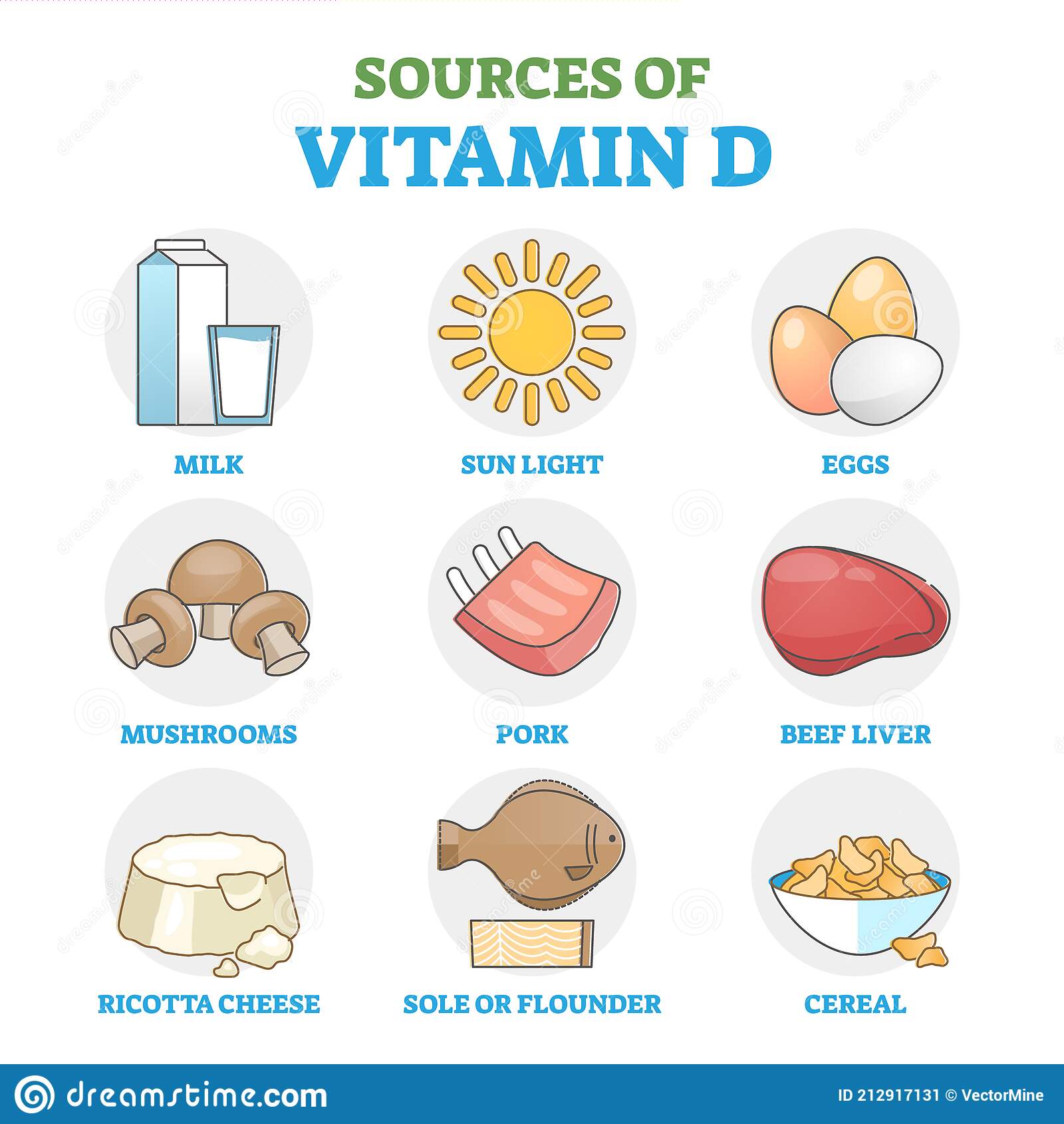
The sun is the most efficient way to get your fix. When those UVB rays hit your skin, they react with a form of cholesterol (7-dehydrocholesterol) to create Vitamin D3. But we spend 90% of our lives indoors. We wear SPF 50. We live in latitudes where the sun is too low in the sky. So, we turn to food.
The problem? Very few foods naturally contain significant amounts of this stuff. You’ve basically got fatty fish, some specific mushrooms, and then a whole bunch of "fortified" products where companies just spray some D2 or D3 onto your cereal.
Fatty Fish: The Heavy Hitters
If you like seafood, you’re in luck. Fatty fish are arguably the best good sources of vitamin d you can find at the grocery store.
Take Sockeye salmon. A 3.5-ounce serving can give you anywhere from 450 to 600 IU (International Units). However, there is a huge catch here that nobody talks about: the difference between wild-caught and farmed fish. A study published in the Journal of Steroid Biochemistry and Molecular Biology found that wild-caught salmon contained roughly 75% to 100% more vitamin D than farmed versions. Farmed fish are fed pellets. They aren't eating the plankton and smaller fish that naturally build up those D levels. If you're buying the cheap, pale-pink Atlantic salmon from the big-box store, you’re getting a fraction of the nutrients.
Swordfish is another powerhouse, often boasting over 500 IU per serving. But then you have to worry about mercury. It's a trade-off. Sardines are a better "everyday" choice. They are low on the food chain, meaning less heavy metal buildup, and they pack about 190 IU per tin. Plus, you get the calcium from the tiny bones, which works synergistically with the Vitamin D to strengthen your skeleton.
The Strange Case of Mushrooms
Mushrooms are the only plant-based source that produces vitamin D naturally. But here’s the kicker: they usually produce Vitamin D2, whereas animals (including us) produce D3. Most scientists agree D3 is more effective at raising your blood levels over the long term.
But there is a "hack." Mushrooms contain ergosterol. When exposed to UV light, they convert that into D2. Some commercial brands now sell "UV-exposed" mushrooms that have significantly higher levels. You can even do this at home. Take your store-bought portobellos, flip them gill-side up on a windowsill in direct sunlight for an hour before cooking. It sounds like woo-woo science, but it actually works. It can boost the D content by over 400%.
Why Fortified Foods are a Mixed Bag
Since natural sources are so scarce, the government stepped in decades ago to mandate or encourage fortification. This is why your milk has Vitamin D added to it.
👉 See also: Top 10 Foods Highest in Iron: What Most People Get Wrong
- Milk: Usually around 100-120 IU per cup.
- Orange Juice: Some brands add D and calcium together.
- Cereal: Total or Kellogg’s Special K often have it, but it's usually the D2 form, which isn't quite as bioavailable.
- Plant Milks: Almond, soy, and oat milks are almost always fortified now because they're trying to compete with cow's milk nutritionally.
Is it enough? Probably not. If the RDA (Recommended Dietary Allowance) is 600-800 IU, you'd have to drink a gallon of milk a day to hit the upper limits of what many functional medicine doctors actually recommend. Dr. Rhonda Patrick, a well-known biomedical scientist, often discusses how the "official" RDA might be too low for optimal health, potentially only representing the bare minimum to prevent rickets, not the amount needed for peak immune function.
The Supplement Strategy: D3 vs. D2
When food fails—and for most people in the Northern Hemisphere, it will—supplements are the next step. But don't just grab the cheapest bottle at the pharmacy.
You want Vitamin D3 (cholecalciferol). It’s the same form your body makes. D2 (ergocalciferol) is often what doctors prescribe in those massive 50,000 IU once-a-week doses, but research suggests D3 is better at maintaining consistent blood levels.
Also, Vitamin D is fat-soluble. If you take a dry tablet on an empty stomach with a glass of water, you’re basically flushing money down the toilet. You need fat to absorb it. Take it with your biggest meal, or look for liquid softgels that are suspended in olive oil or coconut oil.
Don't Forget the Partners: K2 and Magnesium
This is the "nuance" part that most articles skip. Taking high doses of Vitamin D in isolation can actually be counterproductive. Vitamin D helps you absorb calcium. But once that calcium is in your blood, it needs to know where to go. Without Vitamin K2, that calcium can end up in your arteries (causing calcification) or your kidneys (causing stones) instead of your bones.
Magnesium is the other piece of the puzzle. The enzymes that process Vitamin D in the liver and kidneys require magnesium to function. If you’re deficient in magnesium—which about 50% of Americans are—your Vitamin D supplements will just sit there, inactive. You'll wonder why your blood tests aren't improving despite taking 5,000 IU a day.
Factors That Kill Your Vitamin D Levels
Even if you're eating all the good sources of vitamin d, several things can sabotage your levels.
- Body Mass Index (BMI): Vitamin D is sequestered in fat cells. If you have a higher body fat percentage, the vitamin gets "trapped" in the tissue and doesn't circulate in the blood where it's needed. People with obesity often need 2-3 times more Vitamin D to reach the same blood levels as leaner individuals.
- Age: As you get older, your skin becomes less efficient at synthesizing D from the sun. A 70-year-old makes about 25% of the Vitamin D that a 20-year-old makes with the same sun exposure.
- Skin Tone: Melanin acts as a natural sunscreen. People with darker skin tones need significantly more time in the sun to produce the same amount of Vitamin D as someone with fair skin. This is a major health equity issue that often goes unaddressed in standard clinical advice.
- Gut Health: Since D is fat-soluble, anything that messes with fat absorption (like Celiac disease, Crohn’s, or even having your gallbladder removed) will tank your levels.
Real-World Action Plan
Don't guess.
The first thing you should do is ask your doctor for a 25-hydroxy vitamin D test. It’s the only way to know where you actually stand. Most labs say "30 ng/mL" is the cutoff for "normal," but many experts, including the Vitamin D Council, suggest that 40-60 ng/mL is the sweet spot for disease prevention.
Once you have your number, adjust your intake.
- Eat fatty fish twice a week. Opt for wild-caught sockeye or canned sardines.
- Sun-dry your mushrooms. It sounds weird, but the UV-boosted D2 is a great vegan-friendly top-off.
- Audit your supplements. Ensure you're taking D3 with K2 (specifically the MK-7 form) and getting enough magnesium through spinach, pumpkin seeds, or a glycinate supplement.
- Get "Smart" Sun. Use an app like "dminder" to track when the sun is actually at the right angle in your zip code to produce Vitamin D. Aim for 10-20 minutes of midday sun on your arms and legs without sunscreen, then cover up or apply SPF to avoid burn damage.
Vitamin D isn't a magic pill, but it's pretty close. By combining these good sources of vitamin d with a bit of scientific awareness regarding absorption, you can move the needle on your health significantly. Stop relying on a single glass of milk and start looking at the whole ecosystem of how this hormone works in your body.
Check your current supplement labels for the "D3" designation. If it says D2, consider switching once the bottle is empty. Next time you're at the market, look for "wild-caught" labels specifically on salmon, as the nutrient profile difference is backed by peer-reviewed data. Finally, schedule that blood test for your next physical; knowing your baseline is the only way to tailor your dosage effectively.