You're lying on a crinkly paper-covered table. The room is dim. A technician slathers cold, clear gel on your abdomen and starts gliding a plastic wand across your skin. On the monitor, a grainy, flickering world of black, white, and gray appears. It looks like a Rorschach test or maybe a satellite map of a distant, stormy planet. Then, the technician freezes the frame. They start clicking buttons to measure a dark, circular mass. That's it. That’s the moment you first see them. If you’ve been dealing with heavy periods or pelvic pressure, seeing fibroid tumors ultrasound images for the first time can feel like a massive relief and a terrifying mystery all at once.
Honestly, most of us have no idea what we’re looking at. To the untrained eye, a fibroid looks like a smudge. To a radiologist, it’s a story about density, blood flow, and location. These noncancerous growths—clinically known as leiomyomas—are incredibly common. Research from the National Institutes of Health (NIH) suggests that up to 80% of women will develop them by age 50. But "common" doesn't mean "simple."
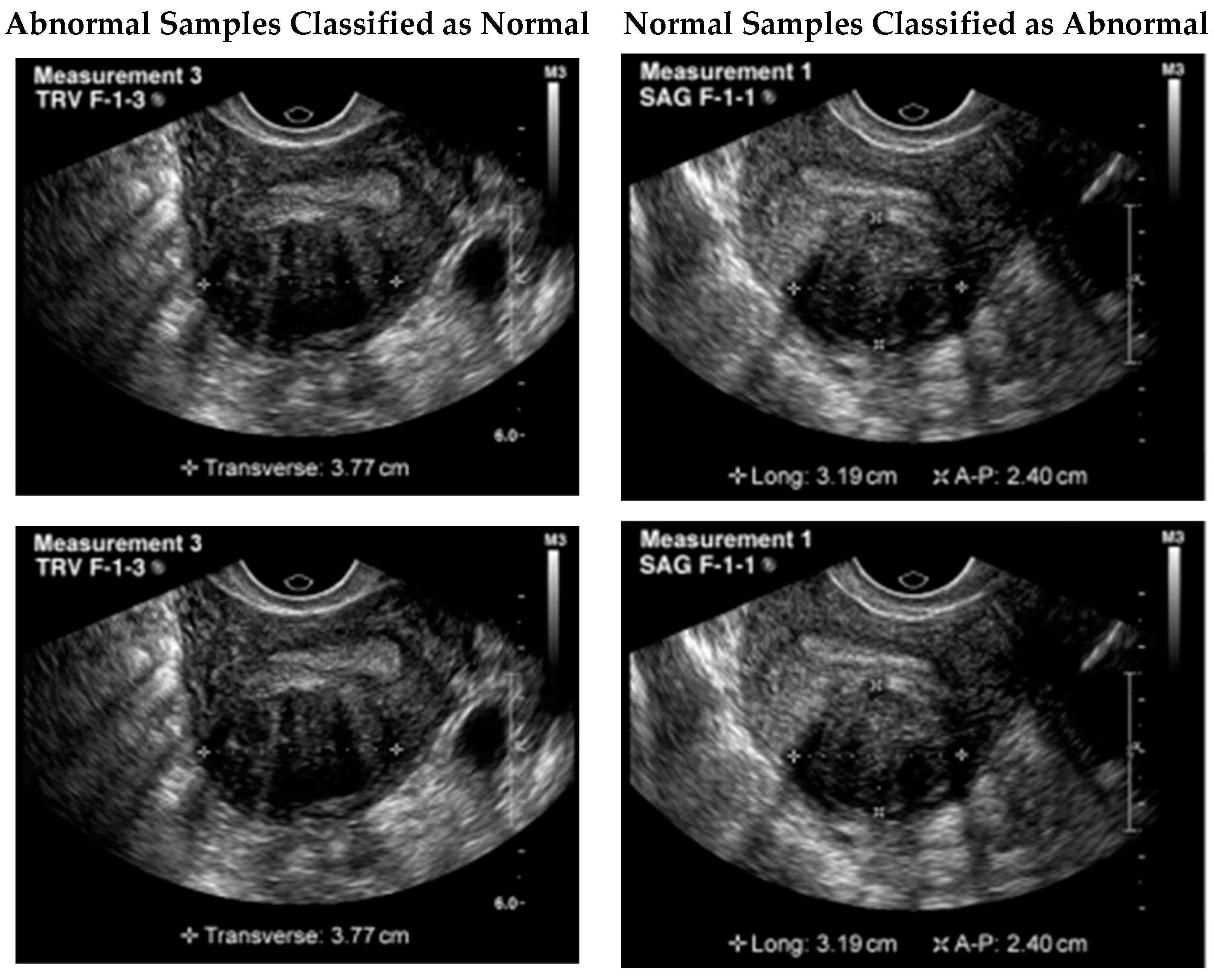
The images matter because they dictate everything that happens next.
Decoding the static: Why fibroids look the way they do
When sound waves hit a fibroid, they don't just bounce back cleanly. Fibroids are made of dense, fibrous muscle tissue. This makes them look different from the surrounding myometrium (the normal muscle of the uterus). On a standard pelvic ultrasound, a fibroid usually shows up as a "hypoechoic" mass. That’s just a fancy medical way of saying it looks darker than the tissue around it because it absorbs or scatters more of the sound waves.
Sometimes they’re "isoechoic," which means they blend right in. Those are the tricky ones. A skilled sonographer has to look for the "whorled" appearance—a subtle, circular pattern in the grain of the image that looks a bit like a knot in a piece of wood.
The Transvaginal vs. Transabdominal Perspective
Doctors usually want both. Why? Because perspective is everything. The transabdominal scan gives the "big picture." It’s great for seeing massive fibroids that have grown out of the pelvis and up toward the belly button. But it's blurry. It’s like looking through a window covered in rain.
The transvaginal ultrasound is the close-up. The probe is much closer to the uterus, providing high-resolution fibroid tumors ultrasound images that can catch tiny "seedling" fibroids only a few millimeters wide. If your doctor mentions "shadowing" on the report, don't panic. It just means the fibroid is so dense that sound waves can’t pass through it, leaving a dark streak behind it on the screen. It’s actually one of the primary ways experts confirm the mass is a fibroid and not something else, like a polyp.
👉 See also: Why the Ginger and Lemon Shot Actually Works (And Why It Might Not)
Not all shadows are equal: Classifying what we see
Radiologists aren't just looking for "a bump." They are looking for where that bump sits. The location changes your symptoms and your treatment options entirely.
- Subserosal Fibroids: These are the ones that grow on the outer surface of the uterus. On an ultrasound, they look like they’re "hitching a ride" on the outside. They can get huge without affecting your period, but they might press on your bladder, making you feel like you have to pee every twenty minutes.
- Intramural Fibroids: These live deep inside the muscular wall. They make the uterus look bulky or asymmetrical. If you see an ultrasound image where the uterus looks lopsided or "globular," this is usually the culprit.
- Submucosal Fibroids: These are the troublemakers. They grow just under the uterine lining and push into the cavity where a baby would grow. Even a tiny one—the size of a grape—can cause enough bleeding to make you anemic. On the screen, these often look like they are indenting the white line (the endometrium) in the center of the uterus.
There are also "pedunculated" fibroids. These grow on a stalk. Imagine a mushroom growing off the side of the uterus. On a moving ultrasound, these can actually shift around, which is wild to see in real-time.
When the image isn't clear enough: Degeneration and Calcification
Fibroids aren't static rocks. They change. They grow, and sometimes, they outgrow their own blood supply. When this happens, the fibroid starts to "die" in the center—a process called degeneration.
This completely changes how fibroid tumors ultrasound images look. Instead of a solid dark circle, you might see "cystic" areas. These look like clear, black holes inside the fibroid, filled with fluid. It can be startling to see, but it’s a well-documented stage of fibroid life.
Then there’s calcification. This usually happens in older fibroids or after menopause. The tissue turns hard, almost like bone. On an ultrasound, these look incredibly bright white (hyperechoic) and cast a very heavy, dark shadow behind them. They are basically the "scars" of old fibroids.
The limits of the screen: What ultrasound misses
We have to be real here: ultrasound is a screening tool, not a perfect map. It has limitations.
✨ Don't miss: How to Eat Chia Seeds Water: What Most People Get Wrong
One of the biggest challenges for doctors is distinguishing between a standard fibroid and adenomyosis. In adenomyosis, the uterine lining grows into the muscle wall. On a quick scan, it looks almost identical to a wall of small fibroids. A key difference experts look for is the "rain-in-the-forest" appearance or "venetian blind" shadowing, which is more common in adenomyosis than in localized fibroids.
Also, ultrasound isn't great at "mapping" for surgery. If a surgeon is going in to remove ten different fibroids, they often want an MRI. An MRI is like a 4K movie compared to the ultrasound’s old black-and-white TV. It shows exactly where the blood vessels are and helps the surgeon plan their path.
And then there’s the big "C" word: Cancer. Can an ultrasound tell the difference between a benign fibroid and a rare cancerous leiomyosarcoma? Honestly? Not definitively. Both look like dark, fleshy masses. However, doctors look for "red flags" on the ultrasound: rapid growth, irregular borders, or a high amount of blood flow inside the mass when they turn on the "Doppler" (the part of the scan that shows blue and red splashes for blood movement).
Real talk about the "Radiology Report"
When you get your results back in a patient portal, the language is terrifying. "Heterogeneous echotexture." "Mass effect on the bladder." "Posterior acoustic shadowing."
Don't let the jargon get to you. "Heterogeneous" just means the tissue isn't perfectly smooth—which we already know, because it's a fibroid. "Mass effect" just means it’s pushing on something. If you see the word "vascularity," it means the fibroid is "fed" by blood vessels. This is actually helpful information if you are considering Uterine Fibroid Embolization (UFE), a procedure where they block those specific vessels to shrink the tumor.
What should you ask at your follow-up?
Don't just let the doctor say "you have fibroids" and walk out. You need specifics. Use the information from the fibroid tumors ultrasound images to advocate for yourself.
🔗 Read more: Why the 45 degree angle bench is the missing link for your upper chest
- "Where exactly are they?" (Submucosal fibroids usually need to come out if you want to get pregnant or stop heavy bleeding).
- "What is the volume in centimeters?" (Volume is a better metric than just "length" because fibroids are 3D).
- "Is the endometrial stripe distorted?" (This tells you if the fibroids are messing with the inside of your uterus).
- "Was there any evidence of 'adnexal' involvement?" (This is doctor-speak for "are my ovaries okay?")
Actionable steps for your next scan
If you suspect you have fibroids or are going in for a follow-up, there are ways to make the imaging process more effective.
First, hydration matters. For a transabdominal scan, you need a painfully full bladder. It acts as an "acoustic window," pushing the gas-filled intestines out of the way so the sound waves can reach the uterus. If your bladder isn't full, the images will be "noisy" and hard to read.
Second, request a "Sonohysterogram" if the regular ultrasound is vague. In this procedure, the doctor injects a little bit of saline (salt water) into the uterus during the ultrasound. The water expands the cavity, making the fibroids stand out like islands in a lake. It is the gold standard for seeing if a fibroid is going to interfere with fertility.
Third, keep your own records. Fibroids are all about the "trend." A 5cm fibroid that has stayed 5cm for three years is a very different clinical situation than a 2cm fibroid that jumped to 5cm in six months. Always ask for the actual images on a disc or via a digital link, not just the written report. You might want a second opinion later, and having the original "pictures" is vital.
Lastly, remember that the image is not the patient. You can have an ultrasound that looks "messy" with a dozen small fibroids and have zero symptoms. Or you can have one tiny, perfectly round fibroid that makes your life miserable. Use the fibroid tumors ultrasound images as a guide, but treat your symptoms, not just the picture on the screen.
If your symptoms are manageable, "watchful waiting" is a totally valid path. If they aren't, the ultrasound is your first step toward a treatment plan that actually works, whether that’s hormonal therapy, non-invasive shrinking, or surgery. Knowledge is the end of the "scary mystery" phase. Now you know what those shadows actually mean.