You’re probably here because a lab report came back with a number that looks too high, or maybe you’re just feeling incredibly wiped out after a workout and someone mentioned "lactate." It sounds scary. It sounds like something that’s eating your muscles or signaling a metabolic meltdown.
But here’s the thing. Elevated lactic acid isn't always a "call the ambulance" emergency, though sometimes it absolutely is. Context is everything. If you just ran a 400-meter sprint, your levels are going to be through the roof, and that’s just your body doing its job. If you’re sitting on the couch and your levels are high, that’s a different story entirely.
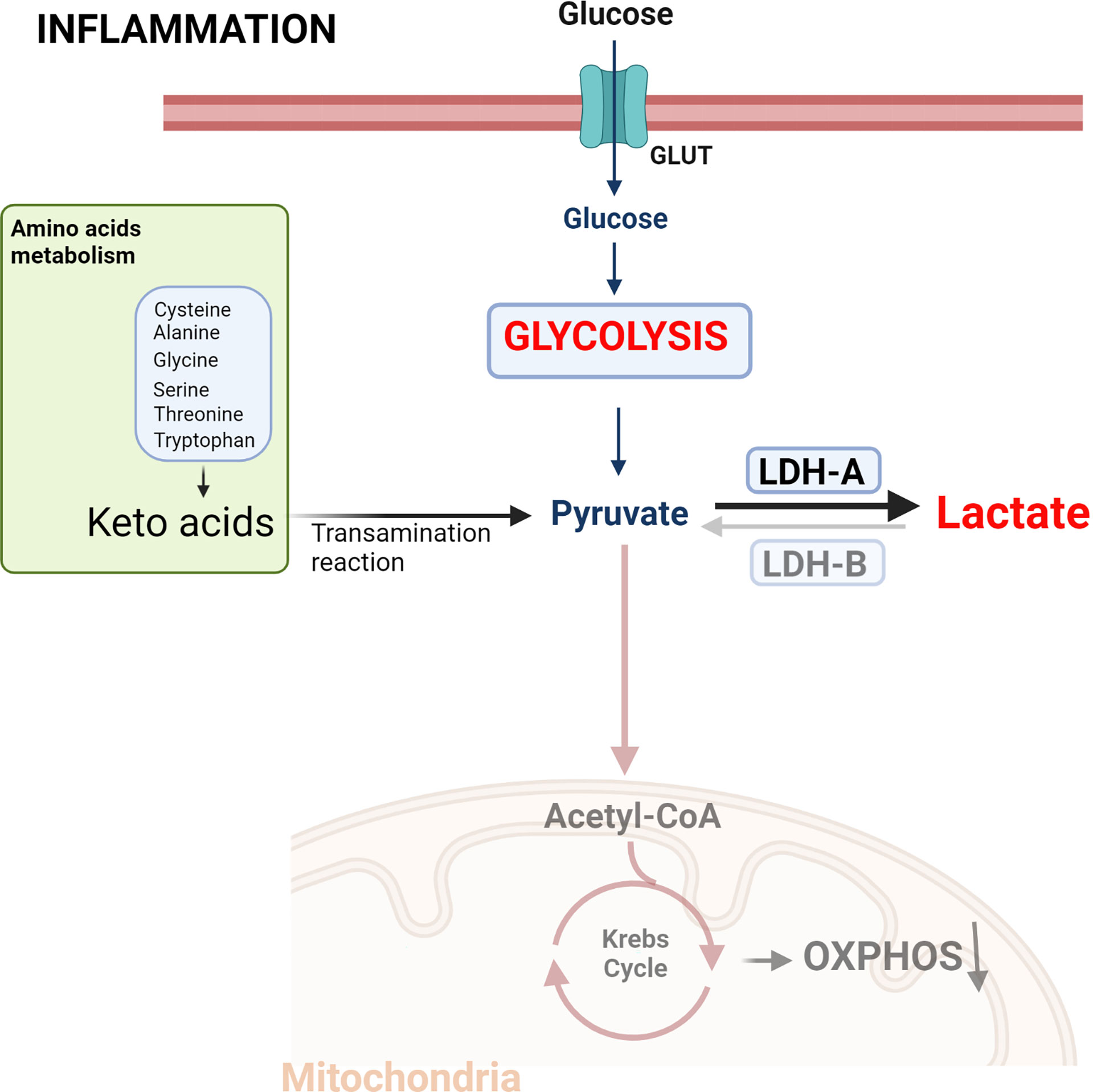
Basically, lactic acid (or more accurately, lactate) is a byproduct of how your body makes energy when oxygen is in short supply. Think of it as a backup generator. When the main power grid—aerobic metabolism—can't keep up with the demand, the backup kicks in.
The Confusion Between Lactic Acid and Lactate
We should clear this up immediately. In the medical world, doctors almost always measure lactate, not lactic acid. Technically, lactic acid releases a hydrogen ion and becomes lactate almost the second it's formed in the body. While people use the terms interchangeably, your blood test will say "Lactate."
Normal levels are usually under 2.0 millimoles per liter (mmol/L). Once you cross that threshold, you’re in the territory of hyperlactatemia. If it gets over 4.0 mmol/L and your blood starts getting acidic (low pH), that’s when we call it lactic acidosis.
That’s the serious stuff.
✨ Don't miss: High Protein in a Blood Test: What Most People Get Wrong
Why Do These Levels Spike Anyway?
There are two main "flavors" of high lactate, and doctors categorize them as Type A and Type B.
Type A is about oxygen—or a lack of it. This is the most common reason. If your tissues aren't getting enough oxygen (hypoxia) or blood flow (hypoperfusion), the cells panic and start churning out lactate. This happens in cases of severe dehydration, heart failure, or sepsis. Sepsis is a massive one. When a person has a systemic infection, doctors watch that lactate level like a hawk. A rising number often means the body is sliding into shock.
Type B is weirder. It happens even when oxygen levels seem fine. This can be caused by liver disease (because the liver is responsible for clearing lactate out of your system), certain medications like Metformin (in rare cases), or even heavy alcohol consumption.
The Exercise Factor
If you’ve ever felt that "burn" during a heavy set of squats, you’ve experienced elevated lactic acid. But don't blame the lactate for the soreness the next day. That’s a myth. Delayed Onset Muscle Soreness (DOMS) is actually caused by micro-tears in the muscle fibers, not the acid.
In fact, lactate is actually a fuel source. Your heart and brain love it. Your body recycles it through something called the Cori Cycle, where the liver turns it back into glucose. It’s a beautiful, efficient loop—unless the system gets overwhelmed.
🔗 Read more: How to take out IUD: What your doctor might not tell you about the process
When Should You Actually Worry?
If you are feeling fine and just saw a slightly high number on a routine test, it might be an outlier. Maybe the tourniquet was left on your arm too long during the blood draw. That’s a real thing—clenching your fist during the needle stick can artificially bump the number.
However, if you have symptoms like:
- Extreme weakness or fatigue
- Shortness of breath (your body trying to blow off excess acid)
- Nausea or abdominal pain
- Confusion or "brain fog"
Then the elevated lactic acid is a signal that something is fundamentally wrong with how your cells are breathing.
The Role of Sepsis and Shock
In a hospital setting, lactate is a "triage" marker. According to the Surviving Sepsis Campaign guidelines, a lactate level greater than 2 mmol/L in a patient with a suspected infection is a huge red flag. It’s often a better predictor of mortality than blood pressure is. Why? Because blood pressure can stay normal even when your internal organs are starting to starve for oxygen. Lactate is the early warning system.
Common Medications and Supplements
Believe it or not, some things you take to get healthy can mess with these levels. Metformin is the big name here. While it’s a lifesaver for millions with Type 2 diabetes, it can occasionally lead to "Metformin-associated lactic acidosis" (MALA), especially if the person has kidney issues.
💡 You might also like: How Much Sugar Are in Apples: What Most People Get Wrong
Then there are rare genetic conditions like mitochondrial diseases. These are the "power plants" of the cells. If the power plants are broken, lactate piles up like trash that never got picked up.
How Doctors Fix It
You don't "treat" high lactic acid directly with a "lactic acid pill." You treat the cause.
If it’s sepsis, you give antibiotics and IV fluids.
If it’s heart failure, you support the heart's pumping ability.
If it’s a drug reaction, you stop the drug.
Once the underlying issue is fixed, the liver usually mops up the excess lactate pretty quickly. It’s a fast-moving marker.
Actionable Steps for Management
If you’re concerned about your levels or want to optimize your metabolic health, here’s what actually helps:
- Check your hydration. Dehydration lowers blood volume, which lowers oxygen delivery to tissues. Drink water. It’s boring but vital.
- Monitor your liver health. Since the liver clears 60% to 70% of the body's lactate, a sluggish liver means higher levels. Limit alcohol and processed sugars.
- Condition your "Lactate Threshold." For athletes, training at the point where lactate begins to accumulate (the threshold) teaches your body to clear it more efficiently. This is why zone 2 and interval training are so effective.
- Review your meds. If you are on Metformin or NRTI medications (for HIV), and you feel chronically "acidic" or fatigued, talk to your doctor about checking a venous lactate level.
- B-Vitamins. Thiamine (B1) is a critical cofactor in the enzymes that process pyruvate. Without enough B1, the pathway gets "clogged," and the body shunts everything toward lactic acid. This is particularly common in heavy drinkers.
Elevated lactic acid isn't a disease in itself. It’s a smoke detector. If the alarm is going off, don't just try to quiet the noise—find out where the fire is.
Check your labs, look at your symptoms, and if you're in an acute state of distress, get to an ER. But if you just finished a HIIT class? Take a deep breath, walk it off, and let your liver do the heavy lifting.