You’ve seen the movies. A man clutches his chest, gasps for air, and collapses onto the floor in a dramatic heap. It’s cinematic, terrifying, and—honestly—kinda misleading. While "crushing chest pain" is definitely a classic symptom, real life is often way more subtle and, frankly, weirder than Hollywood suggests.
The truth is that the early signs of heart attack don't always feel like an emergency. Sometimes they feel like a bad burrito. Or a pulled muscle in your neck. Or just a weird sense of "off-ness" that you can't quite put your finger on.
Wait.
By the time you're on the floor, you've missed the window where medical intervention is easiest. We need to talk about what’s actually happening in the days and weeks before the big event. Because your heart is usually screaming for help long before it finally gives out.
It’s Not Always Pain (and It’s Rarely Just the Chest)
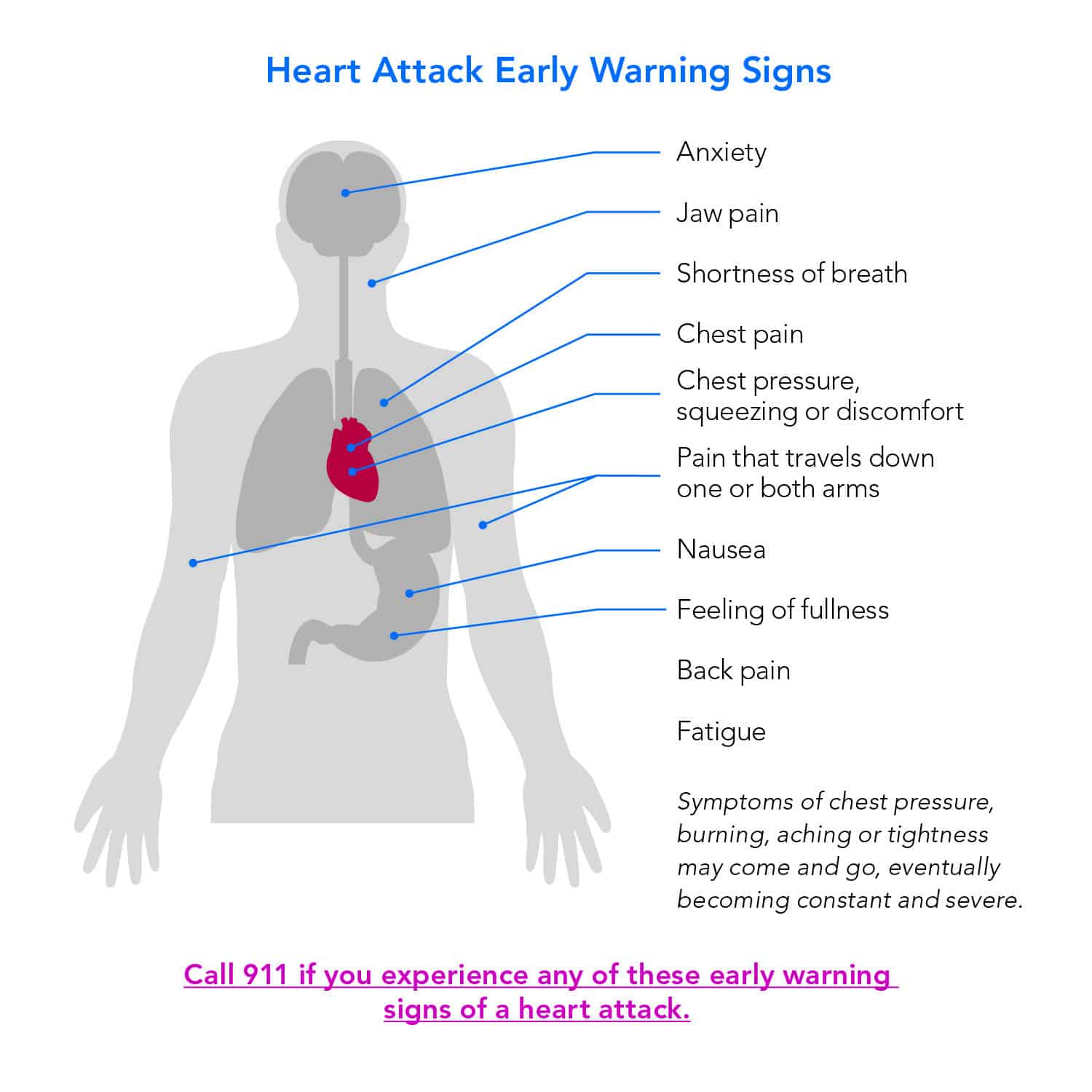
Let’s get one thing straight: the "elephant sitting on my chest" feeling is real, but it’s not the only way this plays out. According to the American Heart Association, many people experience what doctors call "prodromal symptoms." These are the red flags that show up weeks in advance.
Think about it like a flickering lightbulb before the fuse finally blows.
For a lot of folks, especially women, the early signs of heart attack look like extreme fatigue. We aren't talking about "I stayed up too late watching Netflix" tired. This is "I walked to the mailbox and now I need a nap" tired. It’s an overwhelming, bone-deep exhaustion that doesn't make sense given your activity level.
Harvard Health Publishing has noted that in a study of 515 women who had survived heart attacks, 95% said they noticed something was wrong weeks before the event. The most common symptom? Unusual fatigue. Not chest pain. Not arm numbness. Just... being tired.
The Digestive Deception
This is where it gets tricky. You might feel a burning sensation in your upper abdomen. You reach for the Tums. You assume it's the spicy tacos from lunch. But "indigestion" is one of the most common masks for a brewing cardiac event.
Why? Because the nerves in your heart and your stomach are neighbors. Your brain is notoriously bad at telling exactly where visceral pain is coming from. If the bottom of your heart isn't getting enough blood, your brain might interpret those signals as a stomach ache.
If you have persistent nausea or a "heavy" feeling in your stomach that doesn't go away with an antacid, don't ignore it. It’s better to feel silly in the ER for having gas than to stay home with an evolving myocardial infarction.
📖 Related: How to Use Kegel Balls: What Most People Get Wrong About Pelvic Floor Training
The Subtle "Warning Shots" You’re Probably Ignoring
Your body is actually pretty good at signaling distress, but we’re even better at making excuses.
"Oh, my jaw aches? Must be TMJ."
"My back hurts? I probably slept funny."
"Short of breath? I'm just out of shape."
Stop it.
When we talk about the early signs of heart attack, we have to look at the "referred pain" patterns. This is basically when your nervous system gets its wires crossed. Pain can radiate into the jaw, the neck, the back, or even just one arm. Interestingly, it isn't always the left arm. It can be the right, or both.
It feels like a dull ache. Or pressure. Or like someone is squeezing your bicep with a blood pressure cuff.
Then there’s the "sense of impending doom." This sounds like something out of a gothic novel, but it’s a documented medical phenomenon. Many patients report a sudden, overwhelming feeling that something is horribly wrong, even if they can't point to a specific pain. It’s your sympathetic nervous system hitting the panic button. If your gut is telling you that you’re about to die, listen to it.
Why Women and Diabetics Have a Harder Time
The medical world spent decades focusing on how men experience heart disease. That was a huge mistake.
Women are way more likely to have "atypical" symptoms. They might experience shortness of breath, cold sweats, or dizziness without any chest pressure at all. This leads to a dangerous delay in seeking care. If you're a woman, you've basically got to be your own loudest advocate. Doctors, historically, have been more likely to dismiss female cardiac symptoms as "anxiety."
If you feel like you're panicking but you have no reason to be, check your pulse. Check your breathing.
Then there are people with diabetes.
👉 See also: Fruits that are good to lose weight: What you’re actually missing
Diabetes can cause something called autonomic neuropathy—nerve damage. This can actually blunt the sensation of pain. A person with advanced diabetes could literally be having a heart attack and feel almost nothing. They might just feel slightly "weak" or "clammy." This is often called a "silent" heart attack, and it's just as deadly as the loud ones.
Flu-Like Symptoms That Aren't the Flu
Ever had a cold sweat break out while you were just sitting on the couch? That’s a massive red flag.
When the heart struggles to pump blood through clogged arteries, your body puts in extra effort to keep things moving. This triggers your "fight or flight" response, which includes sweating. If you're sweating like you just ran a 5K but you're actually just watching TV, your heart might be in trouble.
Add in some lightheadedness or a feeling of being "spaced out," and you've got a recipe for a medical emergency.
What’s Actually Happening Inside?
To understand the early signs of heart attack, you have to understand the plumbing.
Most heart attacks aren't a sudden 100% blockage out of nowhere. Usually, it’s a slow buildup of plaque (atherosclerosis). A piece of that plaque might rupture, causing a blood clot to form. This clot starts to choke off the blood supply to the heart muscle.
The muscle starts to starve for oxygen. That’s when the "signs" start.
If the blockage is partial, you might get angina—chest pain that comes and goes with exertion. This is your heart saying, "Hey, I can handle sitting down, but don't you dare try to walk up those stairs." If you notice that you can't do things today that you could do easily a month ago, that’s a functional warning.
The "Wait and See" Trap
The biggest mistake people make? Waiting to see if it gets better.
Statistically, the average person waits about three hours before seeking help for heart attack symptoms. Three hours. In the cardiology world, we say "time is muscle." Every minute that blood flow is restricted, heart tissue is dying. Once it’s dead, it doesn't grow back. It turns into scar tissue, which doesn't pump.
✨ Don't miss: Resistance Bands Workout: Why Your Gym Memberships Are Feeling Extra Expensive Lately
That leads to heart failure down the road.
People hesitate because they don't want to "bother" anyone. They don't want to pay for an ambulance if it's just heartburn. They don't want to look dramatic.
Listen: The ER staff would much rather tell you that you have bad reflux than perform an emergency bypass because you waited too long.
Risk Factors You Can’t Ignore
While anyone can have a heart attack, the math is higher for some. If you have high blood pressure (the "silent killer" because it has no symptoms of its own), high cholesterol, or you smoke, your threshold for "worrying" about symptoms should be much lower.
Genetic factors matter too. If your dad had a heart attack at 45, you need to be hyper-aware of your own cardiovascular health by your 30s.
Actionable Steps: What to Do Right Now
If you suspect you or someone near you is experiencing the early signs of heart attack, stop reading and act.
- Call 911. Don't drive yourself to the hospital. If you lose consciousness behind the wheel, you're a danger to everyone. Paramedics can start treatment—including EKG monitoring and meds—the moment they arrive.
- Chew an Aspirin. Unless you're allergic, chewing a full-strength aspirin (325mg) can help thin the blood and potentially break up the clot that's forming. Chewing it gets it into your bloodstream faster than swallowing it whole.
- Sit Down and Stay Calm. Don't try to "walk it off." Physical exertion makes the heart work harder, which increases the damage if blood flow is restricted.
- Be Specific with the Doctor. When you get to the hospital, don't just say "I feel weird." Say "I have pressure in my chest and it's radiating to my jaw," or "I've been abnormally exhausted for three days and now I'm sweating."
The goal is to catch the "stuttering" heart attack before it becomes a total "ST-elevation myocardial infarction" (STEMI). Modern medicine is incredible at opening up blocked arteries with stents, but they can only fix what’s still alive.
Pay attention to the quiet signals. Your heart usually tries to warn you long before it stops. Don't wait for the movie-style collapse to take your health seriously.
Track your "normal." If your "normal" suddenly changes—if you’re more tired, more breathless, or more achy than usual for no clear reason—get a cardiac workup. A simple stress test or an EKG could quite literally save your life.
Schedule an appointment with a primary care physician to establish a baseline for your blood pressure and cholesterol. Knowing your numbers makes it much easier to spot when something is drifting off course. Keep a log of any "weird" sensations, including when they happen and what triggers them, so you can give your doctor a clear picture of your cardiovascular health.