You’re tired. Not just "I stayed up too late watching Netflix" tired, but a bone-deep exhaustion that doesn't go away after a double espresso or a solid eight hours of sleep. Maybe you’ve noticed your skin feels a bit itchier lately, or you’re heading to the bathroom way more often than usual. It’s easy to blame stress. We’re all stressed. But sometimes, these tiny, nagging shifts are actually the early signs of diabetes in women whispering for attention before they start shouting.
Diabetes doesn't always look like the dramatic symptoms you see in movies.
Honestly, for women, the red flags can be incredibly subtle because they mimic "normal" hormonal shifts. If you’re perimenopausal or just dealing with a rough PMS cycle, you might dismiss the thirst or the mood swings as just another part of being a woman. That’s a mistake. According to the CDC, about 1 in 4 people with diabetes don't even know they have it. For women, the stakes are high because high blood sugar affects our biology in ways it simply doesn't for men—impacting everything from vaginal health to heart disease risk.
The Subtle Red Flags Most People Ignore
One of the most frustrating things about spotting early signs of diabetes in women is that the symptoms often hide in plain sight. Take yeast infections, for example. If you find yourself heading to the pharmacy for an over-the-counter antifungal treatment every other month, your body might be trying to tell you that there’s too much sugar in your system.
Yeast thrives on glucose.
When your blood sugar levels are chronically high, your vaginal secretions become a literal all-you-can-eat buffet for Candida albicans. It’s not just about hygiene or "pH balance." It’s about internal chemistry. Dr. Mary Voytek, a specialist in metabolic health, often points out that recurrent vaginal or oral thrush is one of the most overlooked clinical indicators of prediabetes in female patients.
Then there’s the "Polycystic Ovary Syndrome" (PCOS) connection.
If you have PCOS, you’re already at a much higher risk. This isn't just a "fertility issue." It’s an insulin resistance issue. Women with PCOS often have higher levels of insulin circulating in their blood, which can eventually lead to Type 2 diabetes. If you notice dark, velvety patches of skin around your neck, armpits, or groin—a condition called acanthosis nigricans—that is a massive billboard for insulin resistance. It’s not dirt. It’s not a tan. It’s your skin reacting to high insulin levels.
Why Your Vision Goes Blurry (And Then Returns to Normal)
Have you ever had a day where you couldn't quite focus on your computer screen, but the next day everything was fine?
📖 Related: Does Ginger Ale Help With Upset Stomach? Why Your Soda Habit Might Be Making Things Worse
That’s weird, right?
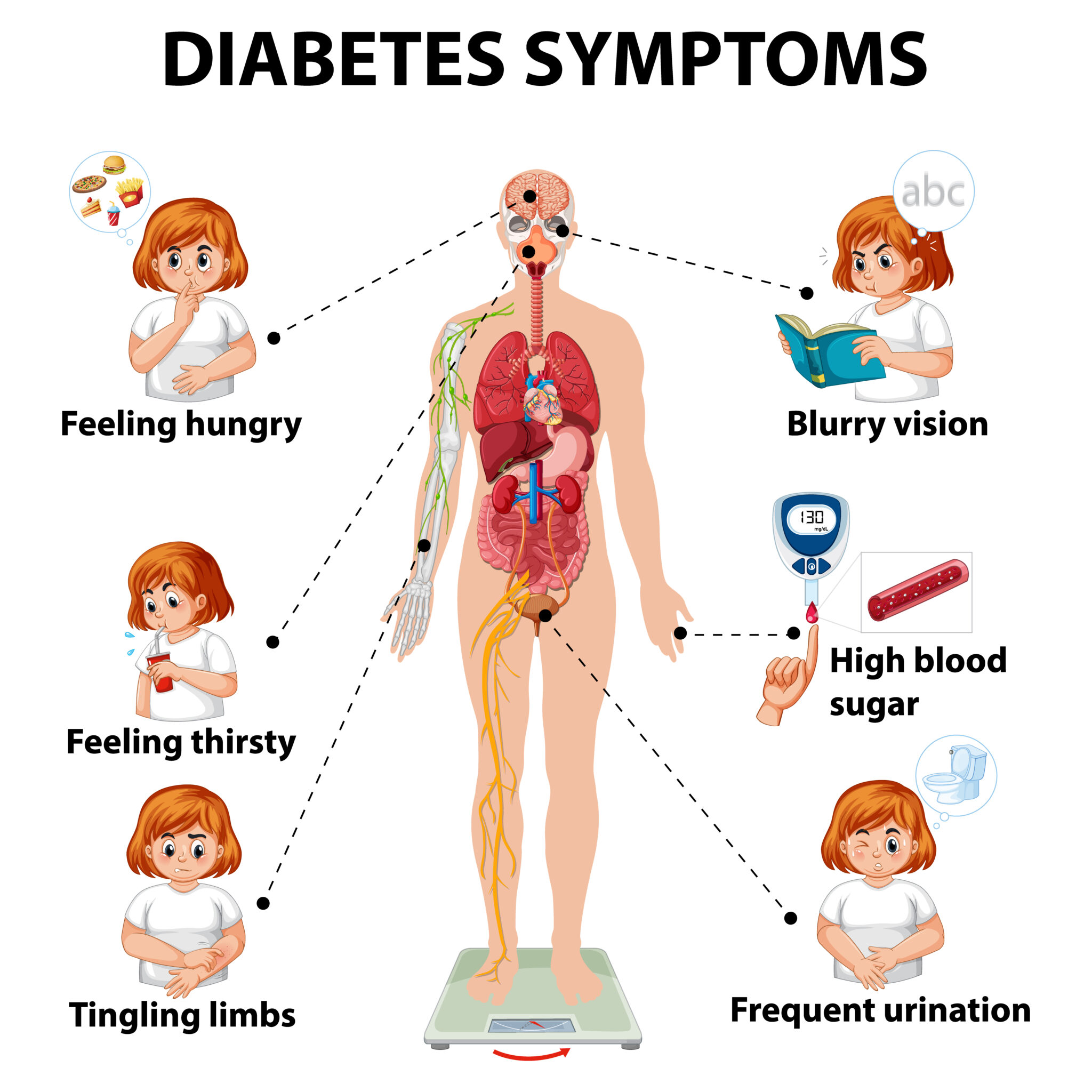
High blood glucose causes the lens of your eye to swell. This changes your ability to see clearly. When your sugar levels drop back down, the swelling subsides, and your vision "corrects" itself. This fluctuating blurriness is a classic early sign. Many women just assume they need a new glasses prescription or that they’ve spent too much time looking at their phones. In reality, your eyes are reacting to the thickness of your blood.
Beyond Thirst: The Fatigue Factor
We need to talk about the "sugar crash" that never ends. When you have diabetes or prediabetes, your body is struggling to move glucose from your bloodstream into your cells for energy. Think of it like a car with a full tank of gas but a clogged fuel line. The energy is there, but you can't use it.
You feel drained.
This isn't just "busy mom" tired. This is feeling like you’re walking through molasses.
Research from the American Diabetes Association (ADA) highlights that women often report higher levels of fatigue than men when dealing with hyperglycemia. Part of this is due to how diabetes interacts with our hormones. Fluctuating estrogen can make insulin sensitivity even more unpredictable. If you find that your fatigue spikes right before your period, it might not just be hormones; it could be your blood sugar becoming even harder to manage during that window.
- Excessive Thirst (Polydipsia): You drink a gallon of water and your mouth still feels like a desert.
- Unexplained Weight Loss: This sounds like a dream to some, but if you’re eating normally and the pounds are dropping, your body might be burning muscle and fat because it can't process sugar.
- Slow-Healing Sores: That paper cut from three weeks ago is still red and angry. High sugar levels impair circulation and nerve function, making it harder for your body to repair itself.
The Sexual Health Connection Nobody Talks About
This is the part that usually gets left out of the brochures. Early signs of diabetes in women can show up in the bedroom. High blood sugar can damage the small nerve fibers throughout your body, including those in the pelvic area.
This leads to:
👉 See also: Horizon Treadmill 7.0 AT: What Most People Get Wrong
- Vaginal Dryness: Which makes sex uncomfortable or even painful.
- Decreased Libido: It’s hard to feel "in the mood" when your energy is zapped and your nerves aren't firing correctly.
- Inability to Orgasm: Nerve damage (neuropathy) can reduce sensation significantly.
It’s easy to blame a low sex drive on age, a long-term relationship, or stress. But if this is a new or worsening problem alongside things like increased thirst or frequent urination, you need to check your A1C levels.
The "Bathroom Trip" Metric
Let’s be real: how many times are you getting up at night? If you used to sleep through the night and now you’re up three times to pee, that’s a signal. Your kidneys are working overtime to filter and absorb the excess sugar. When they can't keep up, they dump that sugar into your urine, dragging fluids from your tissues along with it. This leaves you dehydrated, which makes you drink more, which makes you pee more.
It’s a cycle. A frustrating, sleep-depriving cycle.
Why Is This Happening Now?
You might be wondering why these symptoms are showing up today and not five years ago. Biology is a tipping point. For many women, the transition into perimenopause is when the early signs of diabetes in women become impossible to ignore.
Estrogen is actually protective. It helps your body use insulin more effectively.
When those estrogen levels start to dip in your 40s or 50s, your blood sugar can start to climb. This is often why women are diagnosed later than men, or why our symptoms get confused with "the change." Night sweats, for example, are a hallmark of menopause. But they are also a hallmark of nocturnal hypoglycemia (low blood sugar) or the body’s attempt to deal with high glucose.
Taking Action: What Do You Do Next?
If you’re reading this and nodding your head, don't panic. Prediabetes is reversible. Even Type 2 diabetes is manageable with the right approach. But you cannot fix what you don't measure.
First: Get the Bloodwork.
Don't just ask for a "fasting glucose" test. Ask for an A1C test. A fasting glucose test is a snapshot of one moment in time. An A1C test gives you a three-month average. It’s much harder for the "real" numbers to hide on an A1C.
✨ Don't miss: How to Treat Uneven Skin Tone Without Wasting a Fortune on TikTok Trends
Second: Watch the Carbs, Not Just the Sugar.
Everyone knows to skip the donuts. Not everyone realizes that a "healthy" large bowl of pasta or a giant fruit smoothie can spike your blood sugar just as fast. Focus on fiber and protein.
Third: Move After You Eat.
This is a game-changer. A 10-minute walk after dinner helps your muscles soak up the glucose you just ate. You don't need a marathon; you just need to move your legs.
Fourth: Monitor Your Stress.
Cortisol—the stress hormone—is the enemy of stable blood sugar. When you’re stressed, your body dumps sugar into your bloodstream for "fight or flight." If you’re just sitting at a desk feeling stressed, that sugar has nowhere to go.
Essential Metrics to Track
Forget the scale for a minute. If you’re worried about diabetes, these are the numbers that actually matter:
- A1C Level: Below 5.7% is normal. 5.7% to 6.4% is prediabetes. 6.5% or above is diabetes.
- Blood Pressure: Diabetes and high blood pressure are best friends. They usually travel together.
- Waist Circumference: For women, a waist measurement over 35 inches can indicate a higher risk of insulin resistance, regardless of your total weight.
Practical Next Steps
If you suspect something is off, start a "symptom diary" for just seven days. Note down when you feel the most tired, how many times you’re drinking water, and any skin changes. Take this log to your doctor. Doctors are busy; they love data. Instead of saying "I feel tired," you can say, "I’ve noticed I’m drinking 100 ounces of water a day and still feeling parched, and I’m waking up three times a night to use the bathroom."
That gets attention.
Check your family history too. If your mom or aunt had "borderline sugar," you have a genetic blueprint that makes you more susceptible.
Finally, prioritize your sleep. Lack of sleep directly impairs your cells' ability to respond to insulin. It's a physiological domino effect. Fix the sleep, and you give your metabolism a fighting chance to reset.
Schedule your blood work for the morning when you are fasted to get the most accurate baseline possible. If the results come back in the prediabetic range, see it as a "yellow light"—a chance to slow down and change direction before things get more complicated.