You’re sitting on the couch at 2:00 PM and you just can’t get up. It’s not just a "long day" kind of tired. It’s a heavy, lead-in-the-limbs exhaustion that makes the laundry look like a mountain range. If you recently started a cholesterol medication, you’re probably asking yourself: do statins make you tired or is this just part of getting older?
It’s a frustrating spot to be in. You’re trying to save your heart, but you feel like you’re losing your life to the nap schedule. Doctors often point to the data, which suggests that side effects are rare. But for the person actually feeling the brain fog and the heavy legs, "rare" doesn't mean "non-existent." We need to look at the intersection of clinical trials and real-world biology to figure out why your energy levels might be tanking.
The complicated link between statins and fatigue
Fatigue is one of those slippery symptoms. It’s hard to measure in a lab. Unlike a blood pressure reading or a cholesterol panel, exhaustion is subjective. This is exactly why the question of whether do statins make you tired has been debated in medical journals for decades.
Research published in JAMA Internal Medicine by Dr. Beatrice Golomb and her team at UC San Diego actually put some numbers to this. They looked at over 1,000 patients and found that those taking simvastatin or pravastatin were significantly more likely to report a decrease in energy and increased fatigue during exertion compared to a placebo group. Interestingly, the effect was even more pronounced in women.
💡 You might also like: Why the Anxious and Avoidant Relationship Cycle Is So Hard to Break
Why does this happen? It’s not just in your head.
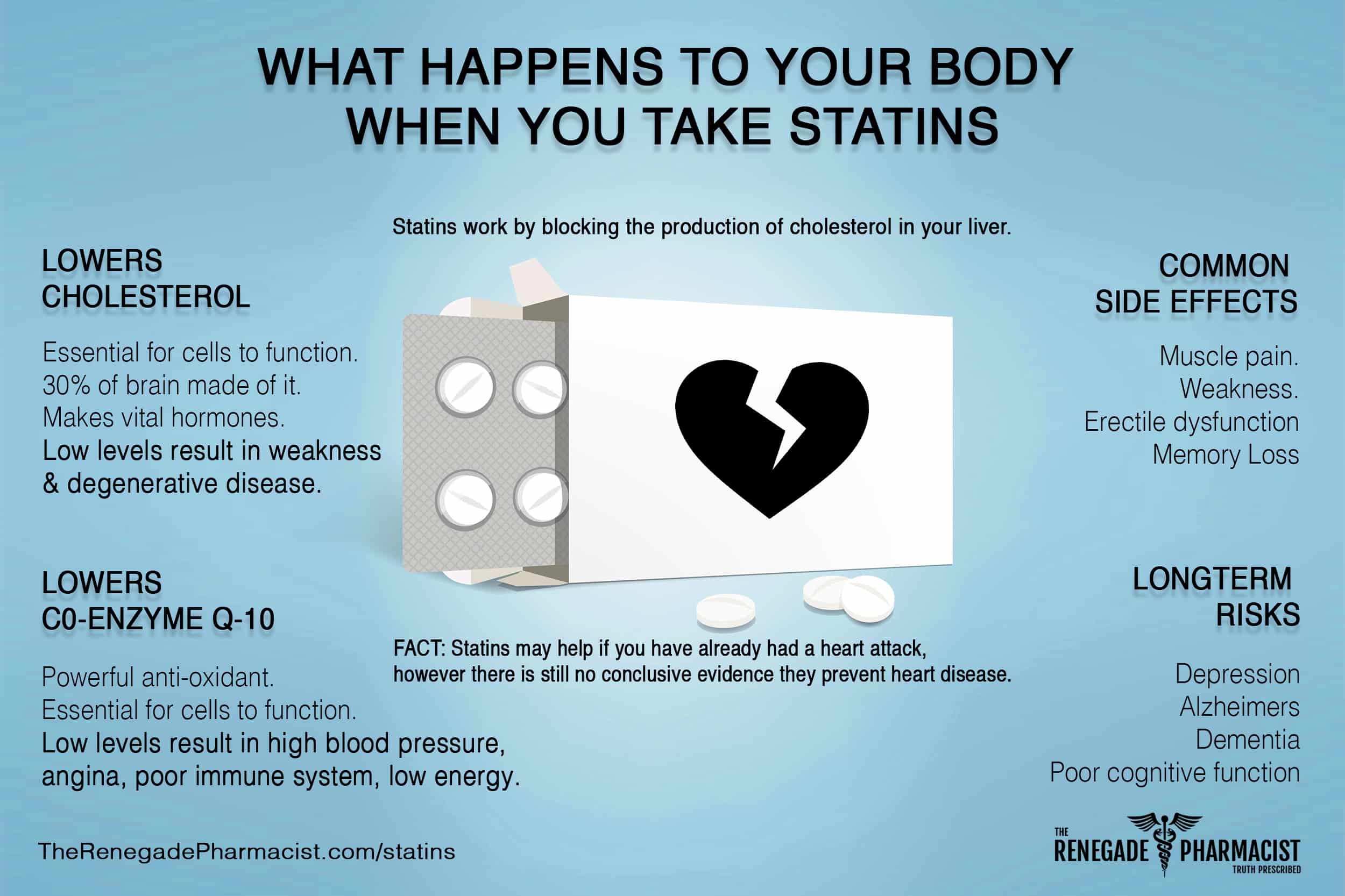
Statins work by inhibiting an enzyme called HMG-CoA reductase. This is great for lowering LDL cholesterol. However, that same pathway is responsible for producing something called Coenzyme Q10 (CoQ10). Think of CoQ10 as the spark plug for your mitochondria—the tiny power plants inside your cells. When you lower CoQ10, you might be inadvertently dimming the lights on your cellular energy production.
Not all fatigue is the same
We have to distinguish between "I feel sleepy" and "my muscles are weak."
True statin-associated muscle symptoms (SAMS) are the most documented side effect. This usually presents as soreness or heaviness in the large muscle groups like the thighs or shoulders. But general lethargy—that feeling of moving through molasses—is different. Some researchers believe this could be related to how statins affect the central nervous system or even how they interact with Vitamin D levels.
Honesty matters here. For some, the fatigue is a trade-off. If you've had a heart attack, the protective benefit of a statin is massive. But if you’re taking it for primary prevention and you can no longer walk your dog because you're too wiped out, the math changes.
Why the "nocebo" effect gets so much press
You might have heard your cardiologist mention the "nocebo effect." This is the evil twin of the placebo effect. Essentially, if you expect a pill to make you tired because you read a scary forum post, you’re more likely to feel tired.
A famous study called SAMSON (Self-Abbreviated Management of Statins) used a "n-of-1" trial design where patients cycled through statins, placebos, and no pills. They found that 90% of the symptoms reported by patients were also present when they were taking the placebo.
That’s a staggering number. It suggests that our brains are incredibly powerful at manifesting physical discomfort.
But—and this is a big "but"—that doesn't account for everyone. Dismissing all fatigue as "nocebo" is lazy medicine. There are real physiological reasons why certain people, particularly those with specific genetic markers or those on high doses like 80mg of atorvastatin, might feel genuinely drained.
Specific statins and their energy impact
It’s a mistake to treat all statins like they’re the same drug. They aren't. They are divided into two main camps: lipophilic (fat-soluble) and hydrophilic (water-soluble).
- Lipophilic Statins: These include drugs like simvastatin (Zocor) and atorvastatin (Lipitor). Because they are fat-soluble, they can cross cell membranes more easily and even pass the blood-brain barrier. Some experts argue this makes them more likely to cause sleep disturbances or "brain fog."
- Hydrophilic Statins: Pravastatin (Pravachol) and rosuvastatin (Crestor) are water-soluble. They primarily stay in the liver. For people struggling with systemic fatigue, switching to a hydrophilic statin is often the first move a smart doctor makes.
Sometimes it’s not the drug itself but the dose. We live in an era of "high-intensity statin therapy." While this is great for plaque stabilization, it’s harder on the mitochondria. A "statin holiday"—monitored by a doctor, obviously—can often reveal if the drug is the true culprit. If the fog lifts in two weeks, you have your answer.
The CoQ10 debate: Supplement or skip?
If you ask ten doctors about CoQ10, you’ll get ten different answers.
The logic is sound: statins deplete CoQ10, so replacing it should fix the fatigue. In practice, the data is a bit of a mess. Meta-analyses have shown mixed results. Some people feel like a new person after starting 200mg of ubiquinol (the more absorbable form of CoQ10), while others notice zero difference.
Is it worth a shot? Usually, yes. It has a high safety profile. If you’re asking do statins make you tired, trying a high-quality CoQ10 supplement for a month is a relatively low-risk experiment. Just don’t expect it to be a magic wand for everyone.
Other sneaky culprits
Before blaming the Lipitor, we have to look at the "accomplices." Many people on statins are also on beta-blockers for blood pressure. Beta-blockers are notorious for causing "exercise intolerance" and general sleepiness. They literally slow your heart rate down, which can feel like someone put a governor on your engine.
Then there’s the lifestyle factor. High cholesterol often goes hand-in-hand with metabolic syndrome or insulin resistance. These conditions cause blood sugar swings that can leave you crashing by mid-afternoon. It’s easy to blame the new pill for a problem that’s actually being driven by your lunch.
How to talk to your doctor without being dismissed
Doctors love data. If you go in and say "I'm tired," they might check your TSH (thyroid) and tell you everything is fine. You have to be more specific.
📖 Related: What to Take for Stomach Pain and Diarrhea When You Can't Leave the Bathroom
Keep a log for two weeks. Note exactly when the fatigue hits. Is it an hour after taking the pill? Is it only when you try to climb stairs? Compare your activity levels now to three months ago. Use a scale of 1-10.
Ask these specific questions:
- "Could we try a hydrophilic statin like pravastatin to see if the fatigue improves?"
- "Is a lower dose combined with a different type of medication like ezetimibe (Zetia) an option for me?"
- "Can we check my Vitamin D and B12 levels to rule out other causes of exhaustion?"
Sometimes, the answer isn't stopping the statin, but changing the timing. Taking your dose at night instead of the morning can occasionally help you "sleep through" the peak of any lethargy-inducing effects.
Actionable steps for managing statin fatigue
If you’re currently struggling, don't just stop your meds. That’s dangerous, especially if you have existing heart disease. Instead, try this systematic approach:
- Switch to Ubiquinol: If you're taking standard CoQ10, switch to the ubiquinol form. Aim for 100-200mg daily. It’s better absorbed, especially as we age.
- Hydration and Electrolytes: Statins can subtly affect muscle metabolism. Ensure you’re getting enough magnesium and potassium. A simple electrolyte powder once a day can sometimes take the edge off the "heavy limb" feeling.
- The Evening Swap: If you take your statin in the morning, move it to right before bed. This is often better for your liver’s natural cholesterol production cycle anyway.
- Request a Blood Panel: Specifically ask for a CK (Creatine Kinase) test if you have muscle pain, but also check your fasting insulin. If your insulin is high, the fatigue might be metabolic, not pharmacological.
- Review the Intensity: If you are on a "fire-breathing" 80mg dose of a statin but your cardiovascular risk is moderate, ask your doctor if a 20mg or 40mg dose would be sufficient. Often, the side effects drop off significantly with a lower dose, while the cholesterol benefits remain substantial.
The reality is that do statins make you tired isn't a yes or no question. For about 5% to 10% of users, the answer is a physical "yes" based on mitochondrial interference. For others, it’s a mix of the nocebo effect and lifestyle factors. You know your body better than any clinical trial. If you feel "off," it's worth investigating the biology behind the bottle.