Doctors hate paperwork. Honestly, it’s the worst part of the job. But when you’re dealing with something as life-threatening as diabetic ketoacidosis (DKA), the paperwork—specifically how we document dm ketoacidosis icd 10 codes—actually matters more than you might think. It’s not just about getting paid by insurance. It’s about the data that tracks how we treat metabolic disasters.
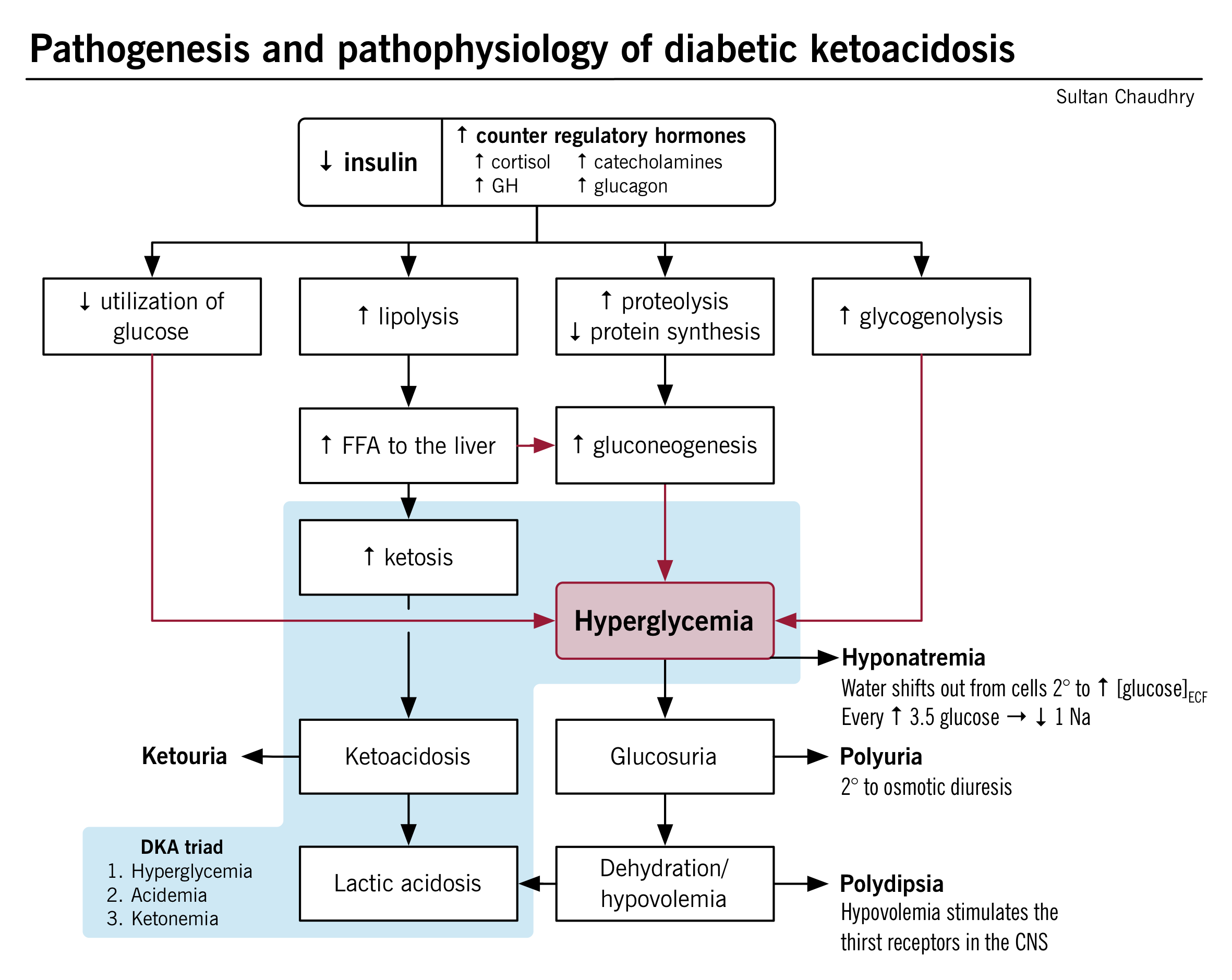
DKA is scary. Your blood turns acidic. Your cells are starving for energy even though your glucose is 600 mg/dL. You're vomiting, you're confused, and your breath smells like overripe fruit or nail polish remover. If you're a coder or a clinician, you know that "DKA" isn't just one thing. It's a complex clinical picture that requires precise classification.
Why the DM Ketoacidosis ICD 10 Codes Are So Specific
The ICD-10-CM (Clinical Modification) system is basically a giant filing cabinet. Back in the day, ICD-9 was pretty blunt. Now? We have to be surgical. The main thing you have to know is that the code changes based on the type of diabetes the patient has. You can't just use one "catch-all" code.
✨ Don't miss: Is 98.0 F to C the New Normal or Just a Math Problem?
If the patient has Type 1 diabetes, you’re looking at the E10 series. For Type 2, it’s E11.
Most people think Type 2 diabetics don't get DKA. That's a myth. While it's way more common in Type 1, "Ketosis-Prone Type 2 Diabetes" is a real clinical phenomenon, often seen in specific populations or during periods of extreme physiological stress like a massive heart attack or sepsis. When that happens, you need the right dm ketoacidosis icd 10 designation to reflect that specific pathophysiology.
Breaking Down the E10.1 Family
For Type 1 Diabetes Mellitus with Ketoacidosis, the primary code is E10.10. This is the "default" for DKA without a coma.
But wait.
If the patient is unconscious or severely obtunded, it jumps to E10.11. That one digit makes a huge difference in clinical severity scores. There's also a code for DKA with "other complications," but honestly, most clinicians stick to the .10 or .11 variants because ketoacidosis is the primary crisis being managed.
The Type 2 Nuance
For Type 2, you use E11.10 (without coma) or E11.11 (with coma). It sounds simple. It isn't. Doctors often mislabel Type 2 patients as Type 1 just because they are in DKA. This is a big mistake in the medical record. The ICD-10 system requires us to be honest about the underlying disease process, even if the presentation looks like a classic Type 1 emergency.
Clinical Realities: What the Codes Don't Tell You
Coding is binary. Medicine is messy.
A patient rolls into the ER. They have Kussmaul breathing—those deep, labored breaths that happen because the body is desperately trying to blow off $CO_2$ to compensate for the metabolic acidosis. Their pH is 7.1. Their anion gap is through the roof.
At this moment, the doctor isn't thinking, "Is this E10 or E11?" They are hanging a saline bag and starting an insulin drip.
But here is where it gets tricky for the hospital. If the physician documents "DKA" but doesn't specify if it's Type 1 or Type 2, the medical coder has to go on a treasure hunt through the charts. This is where "querying the physician" becomes a nightmare. If the record just says dm ketoacidosis icd 10, it's technically incomplete.
✨ Don't miss: Why Most Exercises to Weight Gain Actually Fail (And What to Do Instead)
The Role of Trigger Events
DKA rarely happens in a vacuum. Usually, something pushed the patient over the edge.
- Infection: Pneumonia or UTIs are classic triggers.
- Non-adherence: Maybe they ran out of insulin because of the cost.
- New Diagnosis: About 25% of Type 1 cases are diagnosed only after the patient shows up in DKA.
- The "Brittle" Diabetic: Some people just have incredibly volatile blood sugar levels.
When you're coding, you often have to add secondary codes for these triggers. If a patient has DKA and a UTI, you need both. It paints a full picture of why the patient's metabolic state collapsed.
Common Mistakes in DKA Documentation
Errors happen. A lot.
One of the biggest issues is the confusion between DKA and HHS (Hyperglycemic Hyperosmolar State). HHS is a different beast. It usually happens in Type 2 patients, the glucose is much higher (often over 1000), and there's usually no significant ketoacidosis. The ICD-10 code for HHS is E11.00.
If a doctor writes "DKA" but the labs show HHS, the audit trail gets messy. DKA involves an anion gap and ketones in the blood/urine. HHS doesn't. You can't use the dm ketoacidosis icd 10 codes for an HHS patient.
Another frequent slip-up? Coding for "acidosis" separately.
You don't need a separate code for the metabolic acidosis if you've already used the DKA code. The DKA code includes the acidosis. It's built-in. Adding an extra code for "metabolic acidosis" is redundant and can actually flag an audit for "unbundling" or over-coding.
The Financial and Long-term Impact
Why do we care about these alphanumeric strings? Money and data.
Hospitals are reimbursed based on DRGs (Diagnosis-Related Groups). DKA with coma (E10.11) has a higher "weight" than DKA without coma (E10.10). This reflects the fact that a comatose patient requires more nursing care, more frequent lab draws (sometimes every hour), and likely an ICU bed.
If the documentation is sloppy, the hospital loses money. But more importantly, the patient's medical history becomes unreliable. If a patient is consistently coded as Type 2 but they keep showing up in DKA, a future doctor looking at their records might realize, "Hey, maybe this person actually has LADA (Latent Autoimmune Diabetes in Adults) and needs a different treatment plan."
A Quick Cheat Sheet for the "E" Codes
Let's look at the most common hits in the dm ketoacidosis icd 10 library:
- E10.10: Type 1 DM with ketoacidosis, no coma.
- E10.11: Type 1 DM with ketoacidosis, with coma.
- E11.10: Type 2 DM with ketoacidosis, no coma.
- E11.11: Type 2 DM with ketoacidosis, with coma.
- E13.10: Other specified DM (like post-pancreatectomy) with ketoacidosis.
There is also a "not elsewhere classified" category, but if you're using that, you're probably not looking hard enough at the patient's history.
Beyond the Code: The Human Element
We can talk about ICD-10 all day, but DKA is a traumatic event for a patient. It’s a "near-death" experience for many. When they recover, the focus shifts from the emergency room to the clinic.
The transition from an IV insulin drip to subcutaneous injections is a high-risk time. If the "bridge" isn't managed correctly, the patient can slip right back into ketoacidosis within hours. This is why clear communication between the hospitalist and the primary care doctor is vital. The ICD-10 codes help bridge that gap by providing a standardized "shorthand" for what happened.
Actionable Steps for Clinicians and Coders
If you're responsible for documenting or billing these cases, don't just "guess."
- Verify the Diabetes Type: Check the C-peptide levels or GAD antibody tests if the diagnosis is new. Don't assume Type 2 just because the patient is older or has a high BMI.
- Document the Coma Status: "Altered mental status" isn't the same as "coma" in the eyes of a coder. Be specific. If they were unresponsive, use the word "coma."
- Look for the Trigger: If there's an underlying infection, document it clearly. It changes the complexity of the case.
- Review the Labs: Ensure the pH and bicarbonate levels support a DKA diagnosis before hitting "submit" on that E10.10 code.
DKA is a metabolic fire. The dm ketoacidosis icd 10 codes are the fire department’s report. They tell us how big the fire was, what started it, and how much work it took to put it out. Accuracy here isn't just about administrative compliance—it's about the integrity of the patient's lifelong medical journey.
Next time you're looking at a chart with a bicarb of 8 and a glucose of 500, remember that those five little digits in the ICD-10 book carry a lot of weight. Get them right.
For those looking to improve their facility's accuracy, start by conducting a monthly audit of DKA cases to see where the documentation gaps are. Usually, the "Type 1 vs Type 2" distinction is where the most errors happen. Fix that, and you've fixed 80% of your coding issues.